Vignette 7
Hypnagogic Hallucination
Since his diagnosis the patient’s complaints of excessive daytime sleepiness were successfully treated using three to five 10- to 30-minute scheduled naps per day. The use of central nervous system stimulants was not deemed clinically necessary. Nevertheless, despite the use of imipramine 25 mg twice a day for cataplexy, he continued to report two to three cataplectic-like events per day. To address this issue he discontinued imipramine 2 days (rather than 2 weeks, because of safety concerns) before a formal daytime evaluation for cataplexy. During this study, published in 1996, cataplectic attacks were induced through emotional provocation (a series of jokes) while standard split-screen, video-PSG was performed as the patient was examined in a semirecumbent position to avoid injury during episodes of expected paresis/paralysis.1 He had five total events during what appeared to be REM sleep on PSG, lasting 15, 1, 1, 4, and 10 minutes, respectively. During these events he was able to verbalize that he was having a typical spell, was paralyzed, and was not sleepy, all while answering questions appropriately and retaining memory of three objects over a 1-minute period. During one of these cataplectic events he reported an out-of-body, floating hallucination, which can be fully appreciated in the accompanying video.
Discussion
The International Classification of Sleep Disorders: Diagnostic and Coding Manual, second edition (ICSD-2), describes “Narcolepsy With Cataplexy” as a “Hypersomnia of Central Origin” that is defined by the classic pentad of symptoms: excessive daytime sleepiness (often with sleep attacks), cataplexy, sleep paralysis (“hypnagogic” when going to sleep, “hypnopompic” upon awakening), hypnagogic hallucinations, and nocturnal sleep disruption (insomnia).1–4 This disorder is genetically associated with the human leukocyte antigen subtype DQB1 ∗0602 and an intrinsic loss of hypothalamic neurons containing the neuropeptide hypocretin/orexin. The low cerebrospinal fluid levels of hypocretin-1 allows for the inappropriate onset of REM (i.e., “paralyzed” or “dream”) sleep phenomena that include hypnagogic hallucinations (Vignette Figs. 7.1 and 7.2).5,6
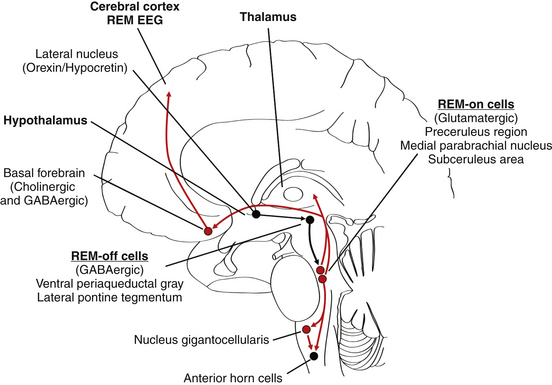
VIGNETTE FIGURE 7.1 This diagrammatical representation of the brain/brainstem in the parasagittal plane shows the very basic structures and mechanism (based upon the recently proposed “flip-flop” model of sleep state transitions by Saper et al5) hypothesized to be involved in narcolepsy with cataplexy. The paucity of orexin (hypocretin) cells in the lesioned LH results in a loss of stimulation of GABAergic REM-off cells in the vPAG/LPT complex, which leads to a disinhibition of the pontine glutamatergic REM-on cells specifically localized in the PCR, the MPBN, and the SCA (referred to as the SCA in cats and the SLD nucleus in rats; not clearly identified in humans). Subsequently, rostrally directed pathways from the PCR and the MPBN lead to the forebrain (the cerebrum, hypothalamus, and thalamus), producing a REM EEG pattern, REM-onset sleep attacks, and dreamlike hallucinations, whereas caudally directed pathways from the SCA lead to hyperpolarization of spinal cord AHCs (directly and indirectly via the NGC), producing the atonia associated with inappropriate REM-onset sleep, cataplexy, and sleep paralysis (major symptoms of narcolepsy). Black circles and lines, Nuclei and neuronal tracts normally inhibited during REM sleep; red circles and lines, nuclei and neuronal tracts normally activated during REM sleep. AHCs, Anterior horn cells; EEG, electroencephalogram; GABA, γ-aminobutyric acid; LH, lateral hypothalamus; MPBN, medial parabrachial nucleus; NGC, nucleus gigantocellularis; PCR, preceruleus region; REM, rapid eye movement; SCA, subceruleus area; SLD, sublaterodorsal; vPAG/LPT, ventral periaqueductal gray/lateral pontine tegmentum. (Modified from Dyken ME, Afifi AK, Lin-Dyken DC. Sleep-related problems in neurologic diseases. Chest. 2012;141:528-544.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







