CHAPTER 74 Neuroimaging in Psychiatry
OVERVIEW
In this chapter we will review neuroimaging modalities that can be used in clinical psychiatry (including the structural neuroimaging modalities computed tomography [CT] and magnetic resonance imaging [MRI], as well as the functional neuroimaging modalities, e.g., positron emission tomography [PET] and single-photon emission computed tomography [SPECT]). We will briefly review the underlying technology for each imaging modality and then will discuss the clinical utility of each. We will conclude with a brief review regarding the use of these, and other, neuroimaging modalities in the context of research. This chapter is an extension of prior reviews we have written on these topics.1–6
STRUCTURAL NEUROIMAGING MODALITIES
Computed Tomography
Technology
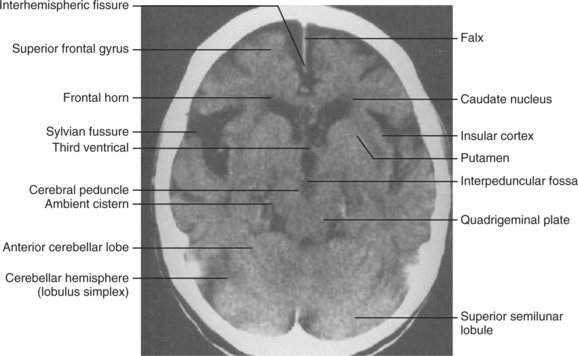
Computed tomography (CT) uses multiple serially acquired x-rays that are attenuated to varying degrees depending on the material through which they pass.7,8 For example, low-attenuation materials (such as air or fluid) appear dark on a CT image, whereas high-attenuation materials (such as bone) appear white. Gradations within the spectrum of attenuation allow for the visual differentiation of brain tissue (Figure 74-1). The serially acquired x-rays are obtained in a rotating axial manner, and these data are then reconstructed using computerized algorithms. The resulting CT image is therefore always an axial image; the capacity to reconstruct or reslice these data to present them from sagittal or coronal perspectives is typically limited because the in-plane resolution is much superior to the slice thickness at which the data have been acquired. The spatial resolution of CT has improved over the years, reaching 1 mm or better in-plane.
Contrast
In some clinical situations CT contrast can be used. CT contrast is typically (but not always) ionic contrast that is radiopaque (i.e., very high x-ray attenuation, meaning that it appears white on the CT image). The CT contrast agent is introduced intravenously. Therefore, CT contrast is especially useful for visualization of lesions that compromise the integrity of the blood-brain barrier (e.g., cerebrovascular accidents, tumors, and inflammation).9 Nonionic contrast is also available, but is more expensive than is ionic contrast. However, ionic contrast is associated with a greater risk of side effects.7 With ionic contrast, idiosyncratic reactions (including nausea, flushing, hypotension, urticaria, and sometimes frank anaphylaxis) occur in approximately 5% of cases. Those at highest risk for idiosyncratic reactions include the young and the old (less than 1 year of age or greater than 60 years of age) and those with a history of cerebrovascular disease, asthma, allergies, and, of course, prior contrast reactions.10 Ionic contrast is also associated with chemotoxic reactions that can occur in the kidney and the brain. Chemotoxic reactions in the kidney include impaired renal function and renal failure. The main risk factor for renal chemotoxic reactions to ionic contrast is preexisting renal insufficiency.11 Chemotoxic reactions in the brain typically manifest as seizures. These usually only occur in 1 in every 10,000 cases, but may occur in 1% to 5% of cases where gross disruption of the blood-brain barrier exists.12
Clinical Utility
CT is particularly useful for the detection of acute bleeding (less than 24 to 72 hours old) or acute trauma, but (as reviewed by Park and Gonzalez8) it is not the modality of choice for subacute bleeding (more than 72 hours old) or for patients who are markedly anemic (i.e., with a hemoglobin less than approximately 10 g/dl). MRI (described later) is superior to CT for most other clinical situations. It should also be noted that CT uses ionizing radiation; thus, it is strongly contraindicated in pregnancy and it is relatively contraindicated in children. However, CT is appropriate when MRI is contraindicated (e.g., with paramagnetic prostheses).
Magnetic Resonance Imaging
Technology
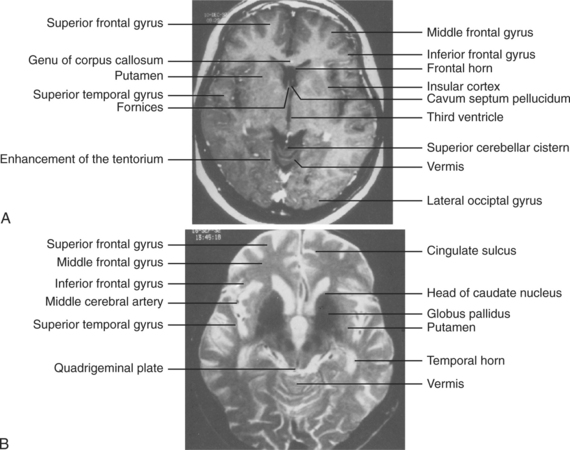
Magnetic resonance imaging (MRI) does not use radiation; instead it uses strong magnetic fields and the magnetic properties of hydrogen atoms to create structural images.13,14 Hydrogen atoms in water act as small magnets and align themselves in the same direction when within a magnetic field. The introduction of brief radiofrequency pulses perturbs this alignment. The relaxation of the hydrogen atoms moves them back into alignment after the radiofrequency pulse is removed; this process emits energy signals that are used to construct the images. This relaxation can occur at different rates, with each relaxation rate resulting in imaging data that may be optimal for different clinical circumstances. For example, T1-weighted and T2-weighted images are two commonly used MRI parameters. T1-weighted images are best for visualizing normal anatomy, whereas T2-weighted images are better for detecting pathology (Figure 74-2). In contrast to CT images (which can only be viewed in the axial plane), MRI images can be reconstructed in multiple planes (i.e., axial, sagittal, and coronal) for more comprehensive viewing.
Magnetic Resonance Contrast
Gadolinium is used as a contrast agent with MRI because it has paramagnetic properties that result in easy visualization.15 Gadolinium is introduced intravenously and thus it is useful for visualizing vasculature. In turn, gadolinium is particularly useful for detecting pathology associated with disruption of the blood-brain barrier or an individual’s vasculature. Gadolinium is much safer than is ionic CT contrast, with far fewer adverse events.
Clinical Utility
Other than acute bleeds and acute trauma, for which CT is the imaging modality of choice, MRI is preferred. As reviewed by Goldstein and Price,14 in comparison to CT, MRI provides better differentiation of white from gray matter (and thus is superior for the identification of white matter lesions) and is superior for visualizing the posterior fossa and brainstem. MRI may soon become the imaging modality of choice for suspected acute bleeds as well. Newer magnetic resonance acquisition methods (such as diffusion weighted imaging [DWI]) are highly sensitive for the detection of acute lesions and distinguishing them from chronic infarcts.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree