52 A Case Study Approach to the Role of Spinal Deformity Correction in the Aging Spine
KEY POINTS
Introduction
Adult degenerative deformity usually presents as a mild curve, which is rarely greater than 30 degrees unless it is superimposed on an adolescent-onset curve. Symptomatic lumbar curves tend to be larger in the idiopathic group than in the degenerative group.1 Degenerative disc disease and osteoporosis are major contributing factors in adult-onset deformity. In these adult deformities, vertebral structural changes with lateral olisthesis are typically associated with degenerative disc and facet joint arthrosis. Adult deformity may also present as a sequela after a decompression for spinal stenosis or spinal fusion for degenerative disc disease. In primary as well as secondary deformities, the degenerative process plays a central role and leads to loss of lumbar lordosis, not infrequently progressing to thoracolumbar kyphosis.
Natural History
Idiopathic Curves
Untreated adolescent idiopathic curves are known to progress after skeletal maturity 2–4. On long-term follow-up of patients with adolescent scoliosis at the University of Iowa, Weinstein et al reported that 68% of the curves progressed after maturity. Thoracic curves progressed at 1 degree per year, thoracolumbar at 0.5 degree per year. Factors associated with curve progression were Cobb angle greater than 30 degrees, apical vertebral rotation more than 30%, presence of lateral olisthesis, and a poorly seated L5 vertebra over S1 in lumbar curves 4.
Degenerative Curves
Pritchett and Bortell reported on the natural history of degenerative scoliosis in 200 patients. The number of vertebrae involved in the curve were from 3 to 6 (mean 3), with the apex commonly located between L2 and L3, and with 68% of the curves being left-sided. While degenerative spondylolisthesis was noted in half the patients, lateral listhesis was even more common (78%). They found that all the curves with the intercrestal line passing through L5 or the L4-5 interspace with vertebral rotation of 2 or more on the Nash and Moe scale progressed, as did curves greater than 30 degrees with lateral listhesis of 6 mm or more 5.
Korovessis et al. followed up 91 adults with de novo spinal deformity for a period of 3.7 years. The average curve size was 16.5 degrees (range 10° to 36°). Risk factors for progression were lateral olisthesis, a high Harrington factor (the Cobb angle divided by the number of vertebrae involved in the curve), and the disc index 6. In a similar study, Perennou et al. also reported a curve progression of 10 degrees or more in 73% of their patients over a follow-up period of 10 to 30 years, at an average of 3 degrees per year 7.
Imaging Evaluation
Radiographic studies for diagnosis and evaluation of adult scoliosis include full-length standing radiographs, bending films, hyperextension films, CT myelograms, and MRI. Assessment of bone mineral density will provide information regarding the presence and severity of osteporosis.
Standing radiographs with hips and knees in extension are necessary to evaluate the extent of the deformity and to assess sagittal and coronal balance. Supine side-bending radiographs may not be useful in degenerative scoliosis, but are useful in idiopathic scoliosis to assess curve rigidity and flexibility. Other options include traction views and fulcrum-bending views.8 Curve location, curve magnitude, number of levels involved, curve direction, and rotation should be evaluated on the radiographs. The presence of anterolisthesis, the maximum lateral olisthesis, the height of the residual disc spaces, and the presence of osteoporotic compression fractures are the radiographic factors that impact curve progression.
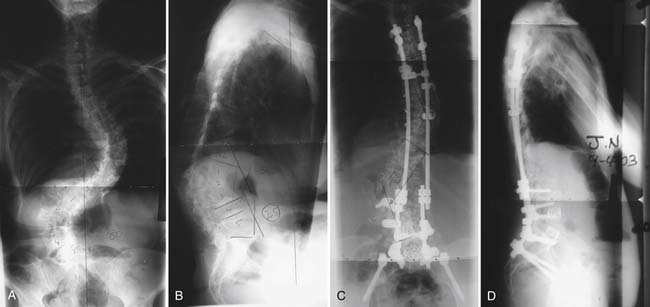
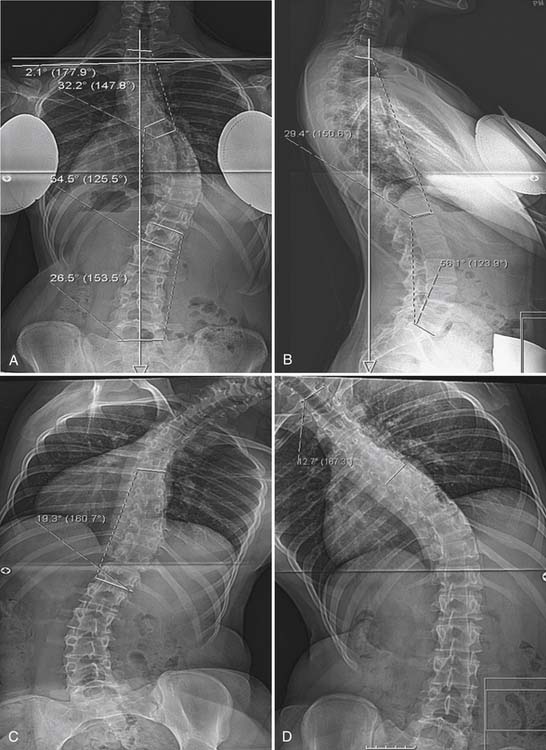
Achievement of coronal and sagittal balance is more important in adults than correction of deformity. Coronal balance is defined by the distance of the C7 plumb line from the central sacral vertical line (CSVL) on standing radiographs. Lateral trunk shift (LTS) measurement is also useful in thoracolumbar curves and is defined as the distance between the midpoint of the horizontal line drawn to the edges of the ribs at the apex of the deformity and the CSVL. (Figure 52-2)
The Role of Conservative Management
A commonly described prerequisite to surgical intervention is the lack of response to conservative care. Even though multiple nonsurgical options are advocated for adult scoliosis, there is currently a lack of evidence in the literature regarding the efficacy of these treatment options. Everett et al reviewed the literature on nonsurgical treatment options for adult scoliosis. They concluded that in the conservative treatment of adult deformity, there is level IV evidence for the role of physical therapy, bracing, and chiropractic care, while there is level III evidence for injections .9
Indications for Surgery
The second category is that of patients over the age of 50, who present mostly with degenerative curves or with idiopathic curves worsened by superimposed degenerative changes. In these patients, surgery is most likely to be indicated for progressive deformities with sagittal or coronal plane imbalance, or for refractory back or radicular pain with or without symptoms of spinal stenosis. Although compromised pulmonary function has also been suggested as an indication, Korvessis et al did not find any difference in pulmonary function in adult scoliosis patients compared with age-related changes in normal persons at an average of 23 years follow-up.6
Surgical Planning
A multitude of factors impact surgical decision-making in this patient population. Achievement of coronal and sagittal balance is the most important goal for many patients. A balanced spine orients the skull so that it is placed over the pelvis. This reduces paraspinal muscle fatigue and pain, improves patient satisfaction, improves cosmesis, and reduces the risk of complications associated with persistent decompensation in the sagittal or coronal plane. A well-balanced spine in the sagittal plane has been found to correlate with a better self-image score in adult deformity patients.10 While extensive surgery might be required to achieve an adequately decompressed and well-balanced spine, the individual surgical plan needs to be matched with the overall health, medical fitness, and expectations from surgery for every patient. Medical and social factors that are known to correlate with poor outcome are nutritional deficiency,11 chronic respiratory conditions,12 diabetes,13 smoking,14,15 coronary or cerebrovascular artery disease, and osteoporosis.16 Osteopenia is a major concern, especially if significant deformity correction is one of the goals. Segmental fixation can create a large surface area for force transmission and possibly prevent fixation failure. Medical treatment of osteoporosis with daily subcutaneous injections of parathyroid hormone for 2 to 6 weeks has been shown to enhance spinal fusion, in animal models.17,18
If an anterior and posterior fusion is planned, a same-day procedure is preferable to a staged procedure, as nutritional status has been found to take 6 to 12 weeks to return to the baseline after posterior surgery.19 Use of parenteral nutrition has been advocated if a staged procedure is planned, to improve the nutritional status before the second stage.20
The Role of Decompression Only in Adult Scoliosis Surgery
In carefully selected patients with degenerative scoliosis, performing a decompression alone without an instrumented fusion may be an option. If the patient presents with symptoms of neurogenic claudication and minimal back pain, it is possible that the patient will get relief with a trial of epidural steroids. If such patients have collapsed disc spaces without any evidence of anterolisthesis or lateral listhesis, they can be treated with decompression alone or decompression with an in situ fusion without instrumentation. Frazier et al. assessed the relationship between preoperative scoliosis and clinical outcome after a decompression only procedure for spinal stenosis in 90 patients with degenerative scoliosis. They inferred that the presence of preoperative scoliosis was associated with less improvement in back pain in these patients postoperatively; however, there was no correlation between preoperative scoliosis and satisfaction or improvement in leg pain and walking capacity after a decompression-only procedure 21.
The Role of Deformity in the Clinical Presentation
Early studies indicated that the incidence of back pain in adult scoliosis patients is about the same as in age-matched controls. Kostuik found a 60% incidence of back pain in adult patients with scoliosis, which was similar to that noted in patients without spinal deformity22. In other studies, patients with adult scoliosis were found to have more severe back pain as compared to controls, especially if the curve progressed beyond 45 degrees23. In more recent studies, Weinstein et al. have reported that chronic back pain was present in 61% of the scoliotic patients as compared to 35% of the controls24. Schwab et al. found a highly significant correlation between the severity of pain in adult scoliosis patients and the presence of lateral olisthesis and obliquity of L3 and L4 endplates on plain radiographs1. Jackson et al. had found the fractional lumbosacral curves most disabling and painful. They reported that while scoliosis greater than 40 degrees and kyphosis greater than 50 degrees correlated with pain, rotational deformity had the highest correlation with pain25. More recently, Buttermann et al. analyzed the correlation between degenerative disc findings on MRI with pain in scoliosis patients. In adult scoliosis patients, they found that the pain typically corresponded to the apex of the curve or to the lumbosacral junction. They found a higher incidence of disc degeneration and inflammatory end plate changes in adult scoliotics than asymptomatic controls. When compared with symptomatic patients with disc degeneration without a deformity, adults with scoliosis had a higher incidence of disc degeneration and inflammatory end plate changes at proximal lumbar levels (T12 – L3)26.
The role of osteoporosis in the causation of adult deformity is well known. Osteoporotic fractures may cause pain, in addition to their contribution to the deformity. Radicular pain in the lower extremities is caused by degenerative changes in adult scoliosis. Root entrapment is more common in the concavity of the curve 7,25. In 200 patients with adult scoliosis, Pritchett et al. had found a 72% incidence of neurogenic claudication and a 45% incidence of neurological symptoms in the lower limbs, most commonly paresthesias 5.
Spinal balance in sagittal and coronal plane can be adversely affected in adult scoliosis. Poor spinal balance is known to worsen the functional status in these patients, and can be quite disabling. Pain in adult scoliosis may arise from muscle fatigue due to abnormal biomechanics caused by the deformed and poorly balanced spine. Glassman et al studied the impact of spinal balance on clinical symptoms in 298 adult scoliosis patients with or without prior surgery. They reported that positive sagittal balance led to greater pain, poor function, and poor self image in patients with or without prior surgery while coronal balance of more than 4 cm correlated with greater pain and poor function. Additionally, the severity of symptoms was found to increase linearly with worsening sagittal imbalance. In terms of location, thoracic curves were better tolerated than thoracolumbar or lumbar curves; however, the magnitude of the curve had a poor correlation with functional status 27,28. In patients with adult degenerative lumbar or thoracolumbar scoliosis, Ploumis et al. reported that coronal imbalance more than 5 cm affected bodily function and moderate to severe lateral olisthesis (more than 6 mm) correlated with higher bodily pain, while sagittal balance did not show a good correlation with functional results 29. In another study, positive sagittal balance (C7 plumbline more than 6 cm) in patients with adult scoliosis has been correlated with worse Oswestry Disability Index scores (ODI), while there was no correlation found between ODI and coronal imbalance. However none of the patients in this study had coronal imbalance worse than 4 cm.30. Loss of lumbar lordosis and thoracolumbar kyphosis have also been found to have a positive correlation with self-reported pain scores in adult scoliosis patients1.
In addition to pain and spinal balance abnormalities, adult deformity can lead to significant body image and cosmesis issues. Deformity has been known to promote a negative body image, which can lead to difficulties in physical functioning and social interaction. Body image is known to be a significant issue with scoliosis patients31,32 Psychosocial studies in adult scoliosis patients have reveled difficulties in social and intimate relationships due to physical difficulties in participation, fear of injury, or self-consciousness33–35 . Attempts have been made to correlate radiographic deformity parameters with health-related quality of life (HRQL) and body image score in adult deformity patients. Except for the sagittal profile, other radiographic measures are found to correlate poorly with HRQL and body image scores in adults1,27,33. Walter Reed Visual Assessment Score (WRVAS) is a visual scale for patients’ assessment of deformity. It has been suggested that, in adults, the WRVAS is a more accurate reflection of the impact of scoliosis deformity on patient body image and HRQL than radiographic indicators. Tones et al. reported that the items of the WRVAS shared a consistent negative correlation with the Physical Functioning, Vitality, and General Health subscales of the SF-36v2, and the Physical Component Summary score in adult scoliosis patients. They also reported that older participants perceived their deformities as more severe than younger participants 26,36.
The importance of these issues from the patients’ perspective is exemplified by postoperative outcome studies in patients who have surgical correction of the deformity. Bridwell et al. had used SRS 22, ODI and SF-12 to assess outcome after surgery in 56 adult scoliosis patients at 1- and 2-year follow-up. They concluded based on these scores that surgical treatment significantly improved pain, self image, and function. They found that the greatest responsiveness to the change after surgery was demonstrated by self image domain, then the SRS total score and pain scores.37.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree