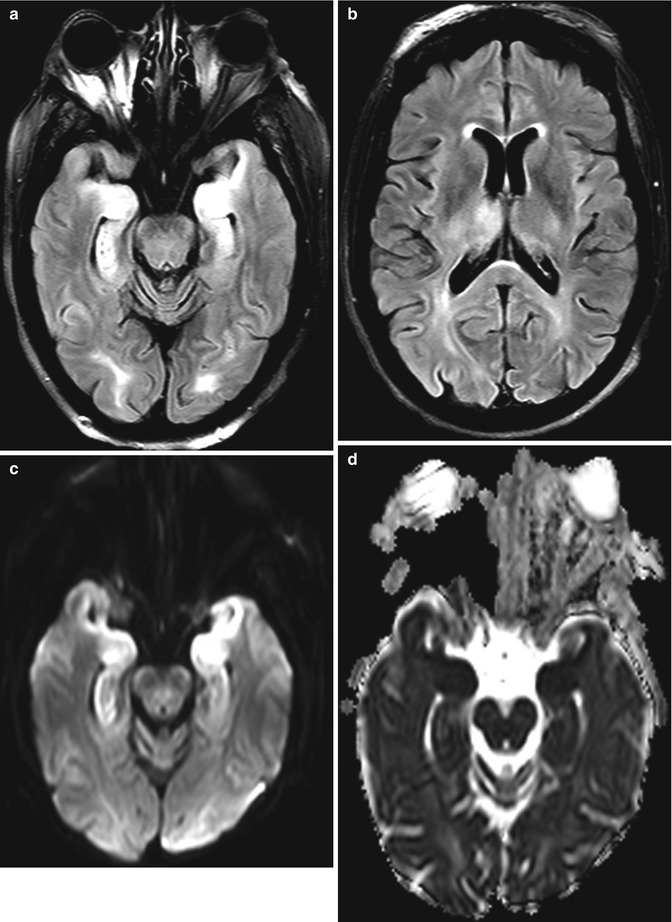
Fig. 49.1
Cerebral edema secondary to fulminant acute liver failure associated with acetaminophen overdose. Axial CT image obtained at the time of presentation soon after ingestion (a) demonstrates an unremarkable appearance of the brain. Axial CT images obtained 4 days (b) and 7 days (c) after ingestion demonstrate progressive loss of gray-white differentiation and severe diffuse cerebral cytotoxic edema secondary to acute liver failure with markedly elevated ammonia levels. There is also progressive effacement of the lateral ventricles secondary to diffuse brain edema
49.4 Differential Diagnosis
Other causes of hyperammonemia include acute hepatic encephalopathy from other cases, such as alcohol and valproate toxicity (refer to Chaps. 2 and 28), as well as citrullinemia and proximal urea cycle disorders. Otherwise, the differential considerations for cerebral edema secondary to acetaminophen overdose on imaging include diffuse hypoxic-ischemic injury (Fig. 49.2), posterior reversible encephalopathy syndrome (refer to Chap. 23), seizure activity (Fig. 49.3), and Creutzfeldt-Jakob disease (Fig. 49.4). Seizure activity can result in reversible cortical FLAIR and DWI hyperintensity, which can be localized or generalized, and with or without associated contrast enhancement. Although Creutzfeldt-Jakob disease can produce T2 cortical and/or deep gray matter hyperintensity and restricted diffusion, it classically presents with rapidly progressive dementia.
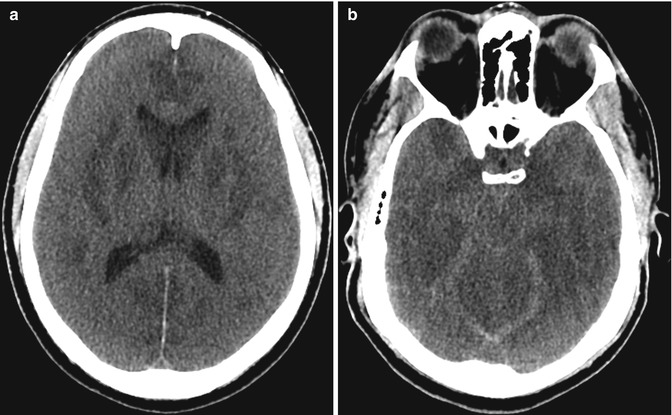
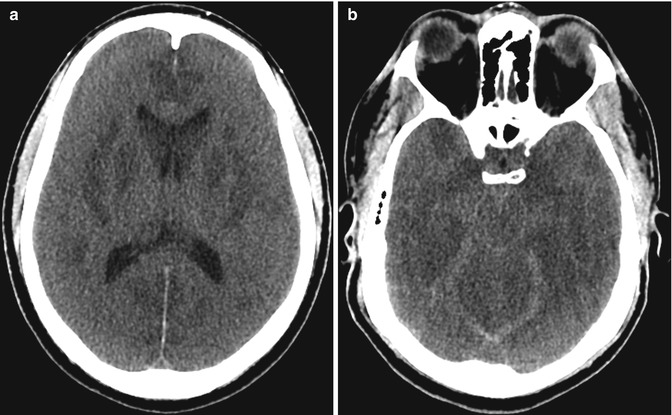
Fig. 49.2
Hypoxic-ischemic encephalopathy. The patient has a history of insulin-dependent diabetes mellitus status post cardiac arrest secondary to DKA status post resuscitation. Axial CT images (a, b) show diffuse cerebral edema with sulcal, ventricular, and basal cistern effacement, as well as more pronounced areas of hypoattenuation within the bilateral basal ganglia