Chapter 5 Adaptation and sport
Sheehan (1990) has written: ‘All of us are athletes, only some of us are training and some are not’.
Hasselman (1995) notes that 30% of office visits to primary care sports medicine practices relate to muscle strain. And with ‘pain’ being the single most common symptom presented to health-care providers of all fields, it is worth reflecting that sport and leisure activity mishaps and overuse account for a great deal of that pain.
In this chapter, some important general influences of sport on the musculoskeletal system will be reviewed, as well as the relation between different types of dysfunction and specific sporting/exercise activities. It will not, however, be possible to evaluate all possible sporting influences on adaptation and dysfunction. The examples chosen are designed to provide insights into broad themes, among the most important of which is the topic of overuse in general, with specific reference to over-training in young people. ‘Young people’ in this context means those who have not yet completed their primary growing stages, with a cut-off point at approximately age 21. People differ and some continue to grow beyond that age, and certainly most continue to mature, but ossification of bones is usually complete by 21. As Hodson (1999) says: ‘Active epiphyses (growth plates) are weakest during puberty and at the end of growth, as they lose their elasticity. Bones are not fully mature until 18–21 years of age’. Examples from athletics, gymnastics and soccer, in particular, provide graphic evidence of the perils of doing too much, especially if this is too soon.
An osteopathic perspective
Allen (1997) offers an osteopathic perspective on sporting-related injuries and dysfunction, which is easily translatable into the context of other manual therapy disciplines. He starts from the principle that the human body has an inherent capacity to cope with (and successfully adapt to) most of the normal demands of the environment. However, it is necessary to recognize that:
Feinberg (1997), a chiropractor, discusses the natural history of recovery from soft tissue injury.
It is critical that active treatment of structures which are in a state of reorganization and repair should not be initiated too early, before there is a sufficient degree of structural integrity in the tissues. Figure 5.1 provides a schematic representation of the stages of repair, which is, of course, a generalization since some will pass through these stages more rapidly while many will be delayed in the recovery process, sometimes due to ill-advised activity or because treatment was initiated too early.
Specific adaptation to imposed demand (‘training’)
Norris (2000) offers the mnemonic SAID (Specific Adaptation to Imposed Demand), which describes the changes that occur in the body in response to particular training and sporting activities. This mnemonic has, of course, wider implications than sports since it can be applied to any regularly performed task or activity, such as playing a musical instrument, working with a computer keyboard, mouse or trackball, using a work-or hobby-related tool (such as a paint brush, used for home improvement or artistic purposes), digging a garden or performing household activities such as vacuuming – or doing any other prolonged or repetitive activity.
Evidence of healthy adaptation to exercise has emerged from research into the benefits noted in conditions as diverse as hypertension, obesity, diabetes, chronic pulmonary disease and a variety of psychological disorders (Allen 1997). However, when potentially beneficial exercise is itself misapplied, problems emerge. If training is undertaken when musculoskeletal imbalance or poor muscular coordination already exists, when the individual or the tissues being worked are in a fatigued state, if there has been inadequate rehabilitation from previous injuries, if the training approach is inappropriate or if training is being poorly applied through inadequate skill, then overtraining or ‘overreaching’ may well result.
Latent trigger points may serve as an adaptional mechanism, forming when specific demands necessitate, for instance, when additional tension is needed to stabilize a hypermobile joint. Although this offers needed assistance locally, one could question the more global consequences of such a feature. Lucas et al (2004) investigated the role of latent trigger points in altered muscle activation patterns. Looking at deficiencies in proximal segments of the upper extremity kinetic chain and whether these might be associated with changes in more distal segments in order to preserve the same movement outcome at the most distal segment, they determined that latent trigger points (LTrs) display the ability to alter the timing of muscle activation, even in muscles further down the kinetic chain. This is clinically relevant, since latent trigger points commonly present without pain. The practitioner and patient (athlete) may be unaware that they exist, although the consequences of their presence may substantially alter performance.
Training variations
There are three broad exercise areas that characterize different training variations.
• Strength training involves high-resistance, low-repetition exercise.
• Endurance training involves low-resistance, high-repetition exercise.
• Sprint training involves a combination of strength and endurance exercises.
Each variation involves different muscle fiber types. According to Ball & Harrington (1998): ‘It appears that most types of training lead to a change in fiber type towards [either] a slower isoform, e.g. Type IIb [fast twitch, fatigue sensitive] [or] Type IIa [fast twitch, fatigue sensitive] [or] Type I [slow twitch, fatigue resistant]’. (See Volume 1, Chapter 2 for discussion of muscle physiology.)
The problems that emerge from overtraining and overuse injuries have multiple predisposing causes including repetitive specific movements, often involving forces greater than those to which the tissues are normally exposed. Even though loads may be within the physiological tolerance of the tissues they are sometimes repeated so frequently as to deny the tissues adequate recovery time. Such chronic loading ‘generates a prolonged period of tissue inflammation and cellular proliferation which does not allow the maturation of injured tissues and resolution of the injury’ (Gross 1992).
Strength training
The types of damage that can occur in strength training are multiple, including microtrauma (e.g. myofibrillar splitting) often resulting from concentric contractions, for example in triceps brachii (MacDougall 1986).
Eccentric exercise patterns (as in lowering weights slowly, as the arms extend) within a strength training program can cause significant tissue damage. Research has shown that z-discs (which separate sarcomeres) may be disrupted and damaged (Ball & Harrington 1998) (see Fig. 5.2).
Degenerative changes in muscle have been noted for approximately 7 days following excessive eccentric exercise (Jones & Newham 1986).
The rate at which tissue damage resolves (i.e. inflammatory phase = 4–6 days; regeneration = from approximately days 5 to 14 and lasting several weeks; remodeling phase after day 21 (see Fig. 5.1)) suggests that the recovery period following exercise-induced microtrauma, and the automatic inflammatory response that results, preclude early application of uncontrolled or aggressive stretching, frictional techniques or deep tissue work, which could delay reorganization and recovery. However, mild elongation and movement of the tissues during this phase is critical so that the connective tissue reorganizes along parallel lines rather than in random patterns that may ultimately restrict movement (DeLany 2000, Lederman 1997, Oschman 1997, Weiss 1961).
Lymph drainage techniques, which may be initiated immediately, encourage the removal of excessive fluid and waste from repair, and reduce potential damage from localized edema (Wallace et al 1997).
Endurance training
The extent to which endurance running, for example, can lead to functional regression is demonstrated by evidence that maximum peak work capacity declines by up to 50% for up to a week following running a marathon (Sherman et al 1984).
Athletes who continue to train vigorously following a marathon show a significantly slower rate of recovery compared to those who rest or who avoid demanding activity for at least a week. The sort of tissue damage that occurs involves necrosis of the muscle, thought to be caused by the significant degree of eccentric activity, especially when running downhill (Hikida & Staron 1983).
Tendon damage may result from endurance (as well as resistance) training. Ball & Harrington (1998) report that: ‘Failure to adapt to external stressors in the Achilles tendon has been characterized by degenerative changes, fibrosis and metaplastic calcification of the tendon’.
Overtraining issues
It is clear that high-intensity training can lead to physiological as well as psychological adaptations and these adaptations are not always beneficial. Detrimental training effects may result from the relative immaturity of the individual (as in the examples relating to young soccer players and gymnasts later in this chapter) or to the phenomenon of overtraining syndrome (OTS). Overtraining is a potential cause of a great many symptoms and two particular aspects of this phenomenon are explored in Boxes 5.1 and 5.2 (overtraining in female athletes and overtraining in young people). In both categories very severe repercussions can develop.
Box 5.2 The overtrained child
Griffin & Unnithan (1999) have evaluated the problem of the overtrained child, a phenomenon which they define as follows: ‘Overtraining has been used as a term to describe both the process of excessive training and the resulting condition of “staleness” or “burnout”.’ They note that multiple ‘positive’ and ‘negative’ factors can affect an athlete’s training state, leading to the ‘exhaustion’ phase of Selye’s adaptation syndrome (Selye 1956) (see Fig. 5.3).
Figure 5.3 Positive and negative factors that affect an athlete’s training state
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):93).
The features of overtraining identified by Griffin & Unnithan are similar to those involved in the ‘female athlete’ discussion in Box 5.1 and include signs and symptoms to which the practitioner should be alert.
General overtraining symptoms:
• weight loss and loss of appetite
• tiredness and disturbed sleep pattern
• greater susceptibility to illness or allergic reactions
• general decline in performance during training and competition
• decline in schoolwork standard
Specific overtraining signs (Griffin 1999, Maglischo 1993):
• increased resting heart rate of 5–10 beats/min
• reduced maximal heart rate of approximately 10 beats/min
• increased exercising heart rate by as much as 24 beats/min
• increased time for heart to return to normal at rest
• increased resting blood lactate levels
• increased submaximal levels of blood lactate
• large reductions in blood lactate at maximal exercise
• increase in submaximal oxygen consumption
Griffin & Unnithan (1999) note specifically that often: ‘By the time overtraining has been diagnosed it is usually too late, the damage has already been done. Training duration and intensity should be immediately reduced, but it is not advisable to stop training completely’. Stopping training for a highly motivated individual might increase anxiety and compound the problem. Weeks and sometimes months may be required to rehabilitate a chronically overtrained young athlete.
Maglischo (1993) has suggested the following principles be applied.
• 80% of training should be at basic endurance levels.
• Get sufficient rest (and adequate sleep).
• Resolve emotional conflicts that may be compounding the problem (which may involve academic pressures).
• Increase carbohydrate consumption. Research shows nutrition to be a key factor and a balanced diet containing 55–65% carbohydrate (mainly complex carbohydrates such as wholemeal bread and pasta), 12–15% protein and under 30% fat is suggested.
• Check for nutritional deficiencies, particularly iron.
• Take a 1-week break from all training if the condition is severe.
Overuse injuries have localized effects, as a rule, while overtraining leads to excessive generalized stress being applied to the athelete’s adaptive mechanisms as a whole. This ‘stress overload’ may reach the point of breakdown, leading to a condition that often manifests with chronic fatigue and reduced performance efficiency as key markers. Although the overtrained female and the overtrained child are the objects of attention in the surveys in Boxes 5.1 and 5.2, the background information contained in these boxes is broadly relevant to all athletes, young or adult, professional or amateur.
Overuse injuries and the young soccer player
Alan Hodson (1999), Head of Sports Medicine, Medical Education Centre, British Football Association, defines an overuse injury as ‘one which involves certain bones or muscles/tendons of the body, which develops over a period of time, due to too much repetitive activity. The injury becomes worse with continued activity at the same level’.
The features that lead to overuse injuries can be summarized to include:
How widespread is the problem of overuse injury in youngsters?
There are an estimated 2.6 million emergency department visits annually in the United States for sports-related injuries in patients aged 5 to 24 years, with the highest percentage occurring in 5– to 14-year-old male athletes. (Damore et al 2003) The sports associated with the highest number of visits are basketball, cycling, football, and soccer (Burt & Overpeck 2001).
Skeletally immature athletes acquire many of the same injuries sustained by adults, but are also at risk of damaging their growth plates, apophyses, and joint surfaces. Overuse injuries represent chronic injuries related to repetitive stress on tissues of the musculoskeletal system, with insufficient recovery time, so overwhelming normal repair processes (Soprano & Fuchs 2007).
Overuse injuries in young athletes often occur when there has been a rapid increase in training, such as may occur during sports camps, or during high levels of athletic training. Extrinsic factors that may contribute to overuse injuries include the relative hardness of training surfaces, inappropriate equipment, and poor coaching (see Chapter 4, the ‘close environment’) (Soprano & Fuchs 2007).
Intrinsic factors include extremity malalignment, such as excess femoral anteversion or foot hyperpronation, scoliosis, decreased flexibility, excessive ligament laxity (see Box 1.3, Chapter 1), muscle weakness or imbalance, and female gender (Busch et al 2004).
• Clinical inquiry should focus on the location and character of the pain, the type of sport played, as well as the intensity, duration, and frequency of participation.
• Clinical examination should focus on signs of inflammation, strength, range of motion of involved joints, and movements that exacerbate symptoms, as well as overall posture and use patterns (gait, etc.).
• Treatment of overuse injuries should include relative rest, possibly confined to a decrease in the intensity and/or frequency of the suspected activity, rather than total avoidance.
• In addition, strategies to reduce inflammation, as well as to retain and regain strength, while maintaining and enhancing range of motion are required.
• In the United Kingdom, in 1992, 34 young soccer players took part in a competition to gain scholarships as part of the British Football Association’s (FA) National School of Excellence scheme. The examination of the youngsters was undertaken by the FA’s Medical Division who found that of the 34 trialists, 12 (35%) were suffering from overuse injuries.
• Five had spondylolisthesis of the lumbar spine which was potentially career threatening (Fig. 5.4).
• Two had tibial growth plate problems in the knee area.
• One had a fibular stress fracture.
• Two had Osgood–Schlatter’s disease (Fig. 5.5).
• One had Sever’s disease (osteochondrosis of the ankle area) (Fig. 5.6).
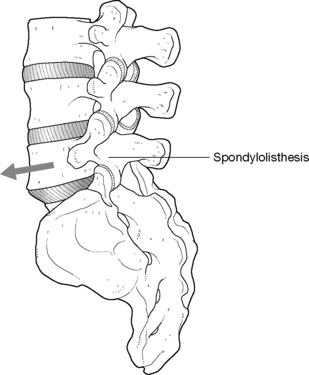
Figure 5.4 Spondylolisthesis
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):89).
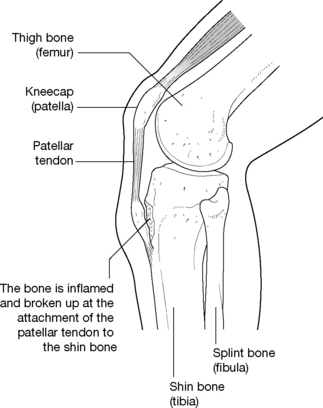
Figure 5.5 The overuse condition of Osgood–Schlatter’s disease
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
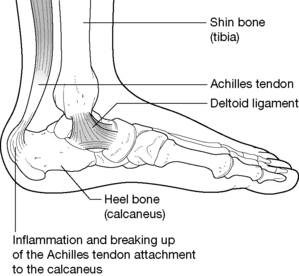
Figure 5.6 The overuse condition of Sever’s disease
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
• Six had Osgood–Schlatter’s disease.
• One had a cruciate ligament problem.
• One had knee and ankle pain.
• One had a tibial growth plate problem.
There is also a particular risk of avulsion injuries, as repetitive action may produce damage where powerful muscles attach to bone (Fig. 5.7).
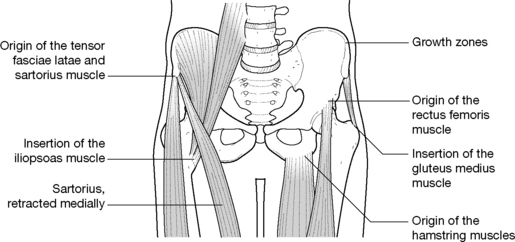
Figure 5.7 Sites of possible avulsion injuries
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):89).
Another major risk for immature musculoskeletal systems is for damage to occur to the knee joint through overuse injury. Some conditions are relatively rare but extremely serious, such as osteochondritis dessicans, in which the articular cartilage of the joint is damaged (Fig. 5.8). Raissakia et al (2007) observe that growth cartilage, articular cartilage and apophyseal insertions are the least resistant sites to repetitive microtrauma in the immature skeleton. Tendonitis, stress fractures, osteochondritis and traction apophysitis are all examples of overuse injuries that are more prevalent in adolescents (Raissakia et al 2007).
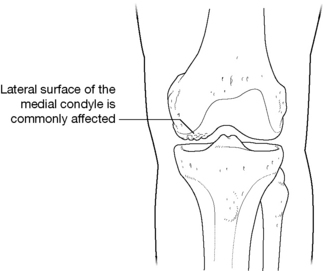
Figure 5.8 Osteochondritis dessicans
(reproduced with permission from Journal of Bodywork and Movement Therapies3(2):88).
If the articular cartilage of the patella itself is damaged the condition known as chondromalacia patellae may develop. Apart from pain in the knee, the young patient may demonstrate loss of strength and even atrophy of the quadriceps (Fig. 5.9).
Prevention of overuse injuries
Hodson (1999) provides suggestions that are summarized below as to what to be aware of and what to do if young people demonstrate signs of overuse injury. He urges therapists and practitioners to remain alert to the risks: ‘Careers can be shortened by non-recognition or poor action in the early years. It is the responsibility of the coach, manager, therapist, administrator and parent to acknowledge the particular susceptibility of young players to injury’. Benny Vaughn AT comments (personal communication 2001):
Signs of overuse injury in young soccer players
• Problems usually become apparent slowly, rather than appearing suddenly, and symptoms continue when the player continues to train, rather than easing off, as would be normal for residual stiffness/discomfort related to an old trauma.
• Aching discomfort is the main symptom, usually in the area of the injury.
• Specific movements may produce pain.
• There is seldom a history of direct trauma.
• The player will frequently complain of localized aching and stiffness during or after competition or training.
• Several days may pass before these symptoms abate after a match/training session.
• Direct pressure over the injured area may be very tender.
• If the overuse injury affects a knee or ankle there may be visible swelling.
• There will often be a history of missed training sessions or matches because of the overuse injury.
• The problem persists and worsens with continued training.
• If symptoms such as these are present in a young active athlete, medical advice should be sought from someone active in sports medicine, so that a suitable course of action can be formulated. It is worth emphasizing that overuse patterns such as those described are a likely predisposing feature of the evolution of myofascial trigger points, which are commonly involved as part of the symptom picture of overtrained individuals, as in all overuse syndrome patterns (Simons et al 1999).
Handling overuse injuries
• Signs and symptoms of pain, such as swelling, tenderness and aching, should never be ignored as they represent the body’s response to a problem; if addressed early, intervention might prevent the termination of a promising career.
• The number of training sessions and competitive events should be limited to what is thought to be a safe level based on the age and the physical demands involved, in consultation with experts in the sport.
• The activities involved in training and playing soccer, or any sport, should be directed as much at enjoyment as at ‘success’.
Tibial stress fracture
A stress fracture involves a hairline or very thin, partial or complete fracture of a bone as a result of its inability to withstand the imposition on it of rhythmic, repetitive, submaximal forces over time. Most research into stress fractures has involved athletics and the military so there is little reliable data as to the frequency of stress fracture in the general population. The incidence of stress fractures is reported to make up 10% of all sports-related injuries (Matheson et al 1986).
McBryde (1976) reported that 95% of all stress fractures in athletes involve the lower extremity, with the upper third of the tibia (the site of approximately 50% of all stress fractures seen in adolescents), the metatarsals and the fibula being the most common sites. Causes can include:
• sudden increases in training or activity
• inappropriately hard playing or running surfaces
• nutritional and/or menstrual status. (Lloyd & Triantafyllou (1986) report that deficiencies of calcium and other nutrients in the diet of amenorrheic gymnasts, ballet dancers and female distance runners contribute to stress fractures occurring due to loss of bone density. See also Box 5.1 on overtraining issues in female athletes.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree