Chapter 97 Adult Thoracic and Lumbar Deformity
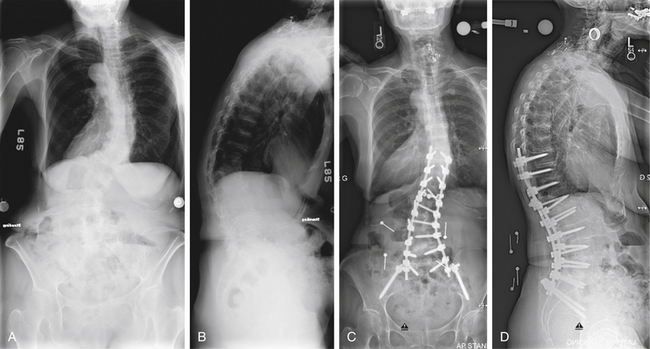
Deformity of the spine implies abnormality of proper spinal alignment that can lead to pain, instability, and neurologic and/or physiologic dysfunction. The deformity can occur in any plane (axial, coronal, or sagittal) and often involves a combination of abnormalities in multiple planes, as demonstrated by the patient in Figure 97-1. An accurate and accepted nomenclature is useful for describing deformities. Table 97-1 defines some common terms used in deformity and is in part adapted from the work of the Scoliosis Research Society (SRS) Terminology Committee and Working Group on Spinal Classification.1,2 Spinal deformity is a broad term that encompasses a variety of pathologies. Scoliosis is defined classically as “lateral curvature of the spine.” However, the pathophysiology of scoliosis can create a three-dimensional deformity involving abnormal spinal curvature (coronal deformity), rotation (axial deformity), and often kyphosis (sagittal deformity). Abnormal spinal profile in the sagittal plane (kyphosis or lordosis) can result in sagittal imbalance. In uncompensated hyperkyphosis, the normal upright posture of head over pelvis and feet (sagittal balance) is shifted forward. Spondylolisthesis is a regional abnormality in the sagittal plane in which one vertebra is displaced ventrally or dorsally in relation to an adjacent level.
TABLE 97-1 Glossary of Terms Frequently Used in Deformity
| Term | Meaning |
|---|---|
| Scoliosis | Lateral curvature of the spine (now recognized to be a three-dimensional deformity) |
| Kyphosis | Dorsal convex angulation of the spine |
| Hyperkyphosis | Kyphosis greater than the normal range |
| Hypokyphosis | Kyphosis of the thoracic spine less than the normal range |
| Lordosis | Ventral convex angulation of the spine |
| Hyperlordosis | Lordosis greater than the normal range |
| Hypolordosis | Lordosis of the cervical or lumbar spine less than the normal range |
| Kyphoscoliosis | Nonidiopathic scoliosis associated with an area of true hyperkyphosis |
| Lordoscoliosis | Scoliosis associated with an area of lordosis |
| Major curve | Curve with the largest Cobb measurement on upright long cassette radiograph of the spine |
| Minor curve | Any curve that does not have the largest Cobb measurement on upright long cassette radiograph of the spine |
| Structural curve | Measured spinal curve in the coronal plane in which the Cobb measurement fails to correct past zero on supine maximal voluntary lateral side-bending radiograph |
| Compensatory curve | Minor curve above or below a major curve that may or may not be structural |
| End vertebrae | Vertebrae that define the ends of a curve in a frontal or sagittal projection |
| Cephalad end vertebra | First vertebra in the cephalad direction from a curve apex whose superior surface is tilted maximally toward the concavity of the curve |
| Caudad end vertebra | First vertebra in the caudad direction from a curve apex whose inferior surface is tilted maximally toward the concavity of the curve |
| Neutral vertebra | Vertebra without axial rotation (in reference to the most cephalad and caudal vertebrae that are not rotated in a curve) |
| Apical vertebra | In a curve, the vertebra most deviated laterally from the vertical axis that passes through the patient’s sacrum (central sacral line) |
| Apical disc | In a curve, the disc most deviated laterally from the vertical axis of the patient that passes through the sacrum (central sacral line) |
| Stable vertebra | Thoracic or lumbar vertebra cephalad to a lumbar scoliosis that is most closely bisected by a vertically directed central sacral line assuming the pelvis is level. Alternatively, both pedicles of this vertebra should lie between vertical reference lines drawn from the sacroiliac joints. |
| Central sacral line (central sacral vertical line) | Vertical line in a frontal radiograph that passes through the center of the sacrum (identified by suitable landmarks, preferably on the first sacral segment) |
| C7 plumb line | Vertical line in a frontal radiograph drawn from the center of C7 (i.e., spinous process) down, which is used to measure compensation (coronal balance) relative to the central sacral line |
| Vertical line in a lateral radiograph drawn from the C7 centroid |
Spinal deformity has multiple causes, including, but not limited to, (1) unknown factors likely related to genetic presusceptibility (as in adolescent idiopathic scoliosis), (2) congenital abnormalities, (3) neuromuscular conditions (i.e., cerebral palsy, spinal cord injury), or (4) conditions associated with spinal cord dysfunction such as myelomeningocele. Deformity can also result as a consequence of trauma (i.e., posttraumatic kyphosis), infection, malignancy, degeneration, or iatrogenic causes. Table 97-2 lists some of these causes. The goal of deformity surgery, despite the etiology, is the relief of the patient’s symptoms while achieving a balanced spine.
TABLE 97-2 Etiology of Deformity
| Deformity | Etiology |
|---|---|
| Idiopathic scoliosis Infantile (2 months to 3 years of age) Juvenile (3 to 10 years of age) Adolescent (>10 years of age) Adult (after skeletal maturity) | Unknown factors likely related to genetic presusceptibility subtype classified by age of onset |
| Congenital scoliosis | In utero derangement of vertebral formation or segmentation |
| Neuromuscular scoliosis | Result of neurologic injury such as spinal cord injury, cerebral palsy, or conditions associated with spinal cord dysfunction (myelomeningocele, tethered cord, spinal dysraphisim) |
| Posttraumatic deformity | Following fracture with progressive vertebral collapse and angulation |
| Postinfectious deformity | Following vertebral osteomyelitis/discitis with vertebral destruction following tuberculosis infection (Pott disease) |
| Degenerative scoliosis and kyphosis | Consequence of advanced degenerative changes |
| Iatrogenic deformity | Consequence of previous interventions (i.e., laminectomy) |
Conditions often detected and treated in the pediatric population, such as adolescent idiopathic scoliosis, Scheuermann kyphosis, congenital scoliosis, neuromuscular scoliosis, and scoliosis associated with other congenital syndromes (syndromic), are discussed in greater detail elsewhere in this text. This chapter will focus on the clinical and radiographic diagnosis, classification, and nonoperative management of adult thoracic and lumbar spinal deformity, with attention paid to scoliosis and kyphosis. Symptomatic deformity in adults is most frequently a consequence of advanced degenerative disease and is termed degenerative or de novo scoliosis. Curves are thought to result as a consequence of asymmetrical degeneration of lumbar discs and facet joints.3 The operative techniques used in treatment of adult thoracic and lumbar deformity are discussed in a later chapter.
Clinical Evaluation of the Adult Patient with Spinal Deformity
Key components of the physical examination include an assessment of the patient’s gait, a musculoskeletal evaluation, and a thorough neurologic examination. Signs of myelopathy such as hyperreflexia, clonus, and an impaired gait may be present in patients with severe thoracic or concomitant cervical disease. Other conditions that may contribute to the deformity such as a leg length discrepancy should be sought. The cosmetic appearance of the deformity is also a considerable factor in the psychosocial well-being of the patient. The importance of appearance is accepted in children but has yet to be thoroughly evaluated in adults.4,5
Diagnostic Imaging
Diagnostic imaging is crucial in the evaluation and management of patients with thoracic or lumbar deformity. A multimodal approach, including MRI and CT, is often used. However, much information can be elucidated from standard radiographs.
Conventional Radiographs
Standing frontal (anteroposterior or posteroanterior) and sagittal (lateral) whole spine (i.e., 14 × 36-inch long cassette or digitally stitched) radiographs are required in the proper evaluation of patients with spinal deformity. Radiographs should show the occiput and shoulders superiorly and the pelvis, including femoral heads, inferiorly.6 Standing views should be taken in a standardized position with the patient’s hips and knees in extension to remove potential compensation of sagittal imbalance. Frontal radiographs are oriented with the patient’s right side on the right side of the screen or view box. This orientation allows the observer to view the film as if he or she is standing behind the patient examining the spine, or as he or she would see it while performing surgery using a dorsal approach. Sagittal radiographs are oriented with the patient facing right. Proper orientation of full-length scoliosis radiographs is demonstrated in Figure 97-2.
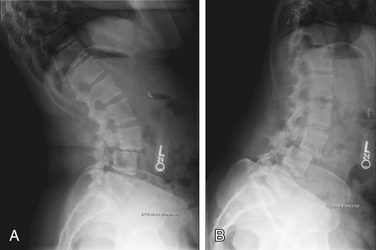
A comparison between the degree of deformity between weight-bearing and non–weight-bearing films (i.e., supine) gives some information regarding the rigidity of the deformity. Additional views to help determine stiffness of the deformity can be useful. These views include supine lateral bending films, bending films over a bolster, fulcrum bending films, and push and traction views. In the evaluation of spondylolisthesis, dynamic lateral views, shown in Figure 97-3, of the lumbar spine are used to help determine the degree of instability. Additional plain radiographic views that are useful in deformity include oblique views to visualize the pars interarticularis, the Ferguson view to better visualize the sacral region, and the Stagnara or Leeds view (an oblique view through the apical region of a scoliotic curve that accounts for rotation) to better visualize the pedicles.
Advanced Imaging
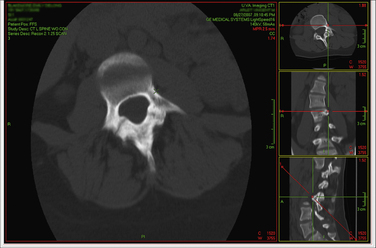
Advances in imaging software such as multiplanar rendering (MPR) allow the surgeon to view multislice CT and MRI data in multiple and adjustable planes. This allows for more accurate preoperative measurement of pedicle diameter and a greater appreciation of the disease process, as shown in Figure 97-4. Three-dimensional reconstructions can easily be created to aid in operative planning. It is also possible to have models of an individual patient’s spine fabricated and surgery simulated prior to the patient reaching the operating room.7,8 In our opinion, thin-cut CT myelography plus MPR provides extremely useful information in operative planning for deformity.
Diagnostic Imaging Conventions and Measurements
The location of a sagittal or coronal deformity is defined by the location of the apex of the curve. The apex is the disc or vertebra that is maximally displaced and minimally angulated. A deformity is considered thoracic if it has an apex between the T2 and the T11-12 disc, thoracolumbar if the apex lies between the T12 and L1 vertebrae, and lumbar if the apex is at or distal to the L1-2 disc.6 In scoliosis, the curve is described based on the side of its convexity. Convex to the right is known as dextroscoliosis, and convex to the left is known as levoscoliosis. Rarely is there just a single curve in scoliosis. The largest curve is called the “main” curve, which is typically structural (e.g., the curve does not correct completely on bending radiographs). Compensatory curves develop in response to the main structural curve and serve the purpose of maintaining spinal balance. Compensatory curves may or may not be structural.
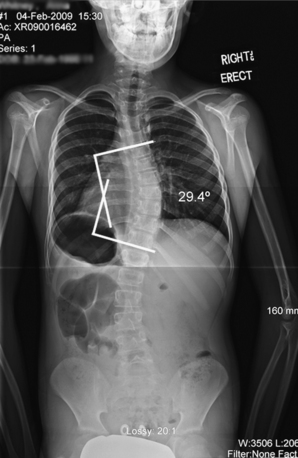
Curve degree is measured via the Cobb method as illustrated in Figure 97-5. Originally described by John Cobb in 1948, the technique involves selecting vertebrae maximally tilted into the curve (end vertebrae). Lines are drawn parallel to the superior end plate of the cephalad end vertebra and the inferior end plate of the caudal end vertebra. If the end plates are not clearly visualized, an alternative technique is to use the pedicle margins as the basis for these lines.9 Bisecting perpendicular lines from the end-plate lines are drawn and the angle determined. The Cobb technique is classically thought to have an inherent error of 3 to 5 degrees; therefore, a change in angle between consecutive films has to be greater than 5 degrees to be considered a true change. Intraobserver error ranges between 1% and 5%, and interobserver error can be as high as 10 degrees.10 Modern Picture Archive and Communication Systems (PACS) workstations and image viewers have tools to measure Cobb angles digitally. To date, studies comparing Cobb angle measurements of primary and secondary curves on digital radiographs and traditional radiographs have shown no statistical difference in the intraobserver or interobserver variance between the two techniques.11–13 New systems that automatically measure the Cobb angle and determine rotation are currently under development and may be able to reduce intraobserver and interobserver variability.14 Proximal and distal neutral vertebrae (not rotated in the axial plane) as well as stable vertebrae (vertebrae above and below the end vertebra that is bisected by the central sacral vertical line [CSVL]) should also be determined because these are used to help select fusion levels in operative planning.
The Cobb method, although initially described for measurement of coronal deformity, is also used to measure degree of lordosis and kyphosis in the sagittal plane. In patients with a normal spinal profile, thoracic kyphosis typically measures between 30 and 35 degrees and lumbar lordosis ranges between 35 and 50 degrees. Approximately two thirds of the total lordosis of the lumbar spine occurs at L4-S1.15
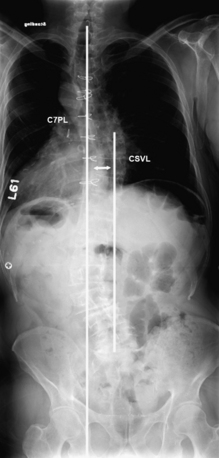
Spinal balance in the coronal and sagittal planes is determined through the use of vertical reference lines. The CSVL is a line drawn up through the center of the sacrum parallel to the edge of the film (e.g., perpendicular to the floor). The C7 plumb line (C7PL) on a frontal radiograph is a vertical line drawn down from the midportion of the C7 vertebral body (approximated by the spinous process, or more accurately through determination of the centroid). Coronal balance, demonstrated in Figure 97-6, is determined by measuring the distance between these reference lines. By convention, a difference with the C7PL to the left is considered negative and a difference toward the right is positive.
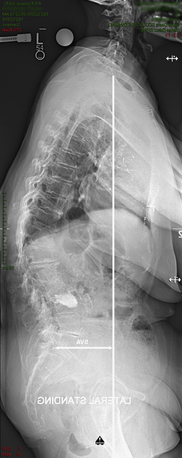
Sagittal balance, shown in Figure 97-7, is determined on a lateral radiograph by measuring the distance between the C7PL, drawn from the centroid (geometric center of the vertebrae) of C7 down and the dorsal/rostral corner of the sacrum. This difference is known as the sagittal vertical axis (SVA). The balance is considered positive if the C7PL falls ventral to this reference point and negative if it falls dorsal to it. Normal mean SVA offset is +0.5 cm and lies within a tight range between −1.0 and +1.0 cm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree