44 Anatomic Aspects of Spinal Cord Disorders
Disorders of the spinal cord provide one of the best opportunities in clinical neurology to apply the basic science of neuroanatomy to the diagnosis and eventual management of patients having myelopathies. Detailed knowledge of spinal cord neuroanatomy is crucial to providing appropriate care to patients with the many various myelopathies as presented in the subsequent chapter (Chapter 45).
Anatomic Correlations
External Structure
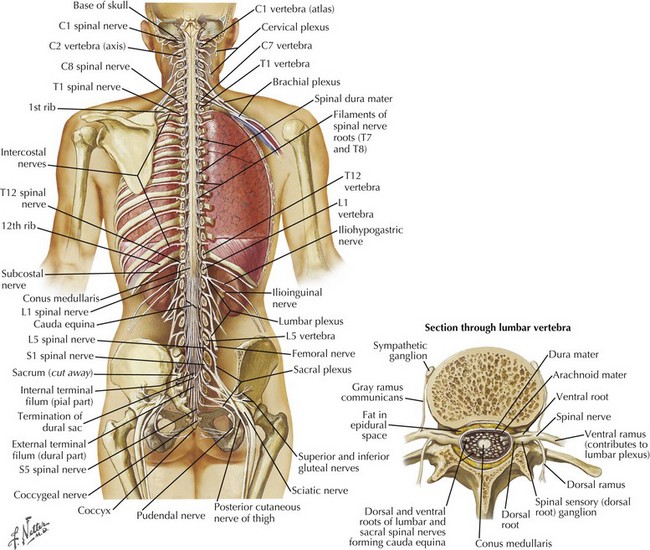
The spinal cord has major functional and teleologic importance, yet it is almost paradoxical that its total mass represents just 2% of the entire central nervous system volume. The spinal canal dimensions are slightly larger, allowing the cord to move freely within the canal during neck and back flexion/extension as its perspective changes with movement. The spinal cord per se is a cylindrical elongated structure flattened dorsoventrally, having a length of 42–45 cm (Fig. 44-1). It lies within the vertebral canal extending from the atlas, continuous with the medulla through the foramen magnum, to the level of the 1st and 2nd lumbar vertebra. Here it tapers into the conus medullaris and terminates as the cauda equina (Fig. 44-1). In conditions such as meningitis, one must not place the spinal needle above the L3 vertebra in order not to specifically damage the underlying spinal cord. It is safe to enter the spinal canal distal to this level because the spinal nerves originating from the distal cord and forming the cauda equina, as nerve roots L2-S5, are anatomically arranged so that they are gently moved aside by the passage of the needle in contrast to the fixed spinal cord that may be easily pierced by the needle insertion and thus cause significant damage.
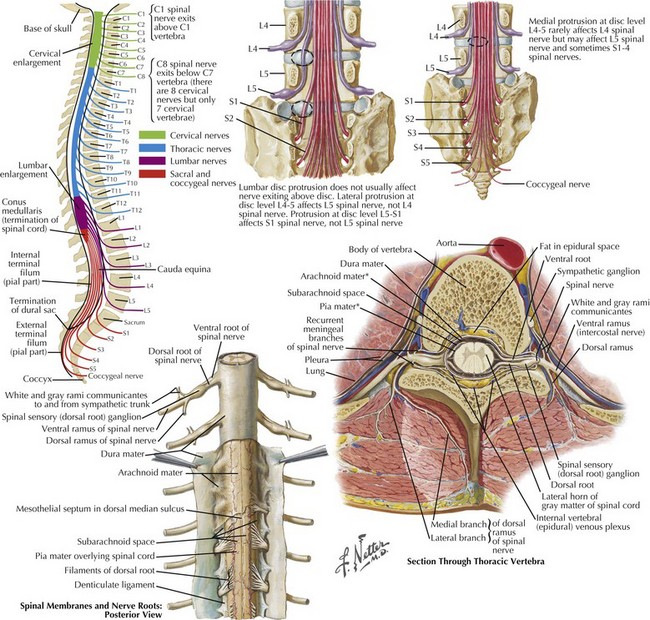
The cervical and lumbar enlargements of the spinal cord provide the nerve roots innervating, respectively, the upper and lower limbs. There are 31 pairs of spinal nerves, each having dorsal sensory and ventral motor roots that exit the cord (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal). Although there are 7 cervical vertebrae, there are 8 cervical nerve roots (Fig. 44-2). The C1-7 roots exit above their respective vertebrae whereas C8 exits below the 7th cervical vertebra and all thoracic, lumbar, and sacral roots exit below their specific vertebrae.
Three protective membranes, the meninges including the dura mater, being the outer layer, then the arachnoid, and the most inner one, the pia, surround the cord (Fig. 44-2). Cerebrospinal fluid flows between the arachnoid and pia. Epidural fat is present in the epidural space between the spinal canal and dura mater. When clinical myelopathies develop, these various disorders are classically categorized as intramedullary, that is, intrinsic to the cord, or extramedullary, occurring secondary to disorders extrinsic to the cord. Extramedullary disorders are further subdivided into those with either an intradural extramedullary locus or a purely extradural site of pathology.
Specific Spinal Tracts
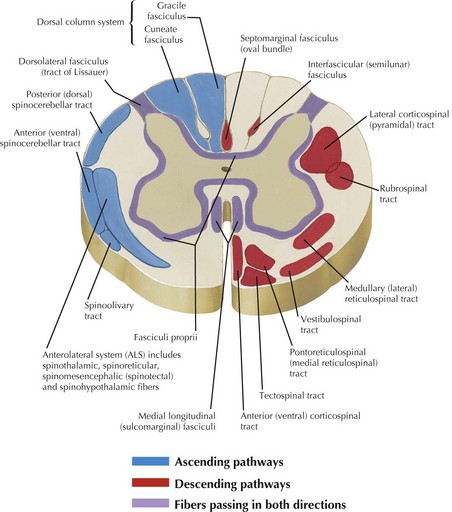
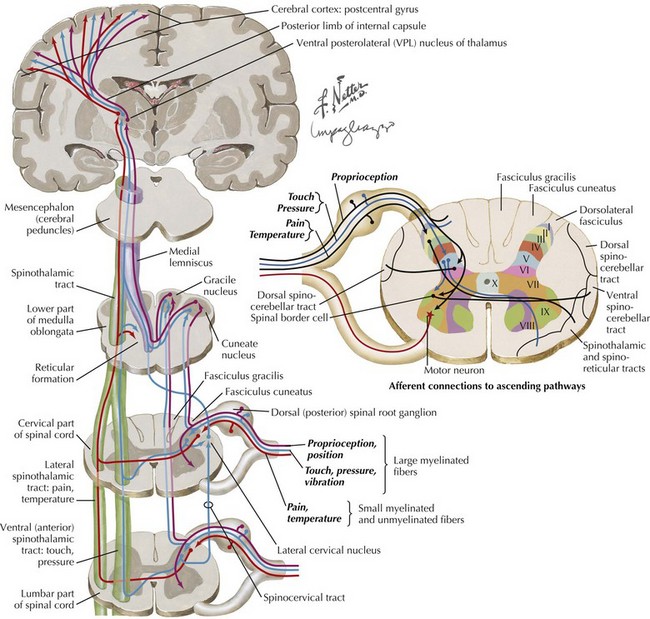
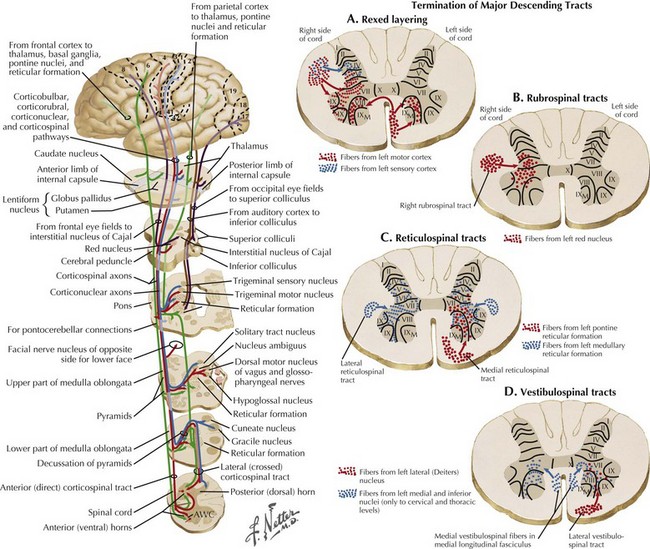
Ascending and descending tracts within the cord are interrupted at sites of cord damage (Figs. 44-3 to 44-5). The subsequent clinical sequelae develop based on the specific tracts that are affected.
Descending Motor Tracts
Corticospinal tracts are responsible for voluntary, skilled movement. They originate in the motor cortex (precentral and premotor areas 4 and 6), postcentral gyrus, and adjacent parietal cortex (see Fig. 44-5). These primary motor fibers descend via the corona radiata, posterior limb of internal capsule, pons, and into the medulla where most distally they then divide into three separate motor tracts (see Fig. 44-3). Up to 90% of these fibers descend in the lateral funiculus as the lateral corticospinal tract. Most decussate within the distal medulla; the uncrossed lateral corticospinal tract is much smaller. The anterior corticospinal tract travels in the anterior funiculus, crossing within the cord.
Tectospinal, rubrospinal, and vestibulospinal tracts (see Fig. 44-3) originate in the superior colliculus, red nucleus, and the lateral vestibular nucleus, respectively. These tracts variously affect reflex postural movements, tone in flexor muscles, and facilitate antigravity and extensor muscles.