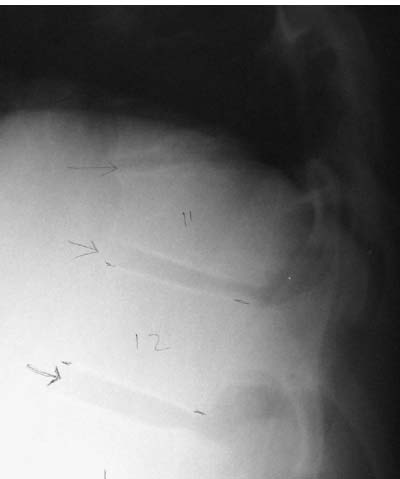
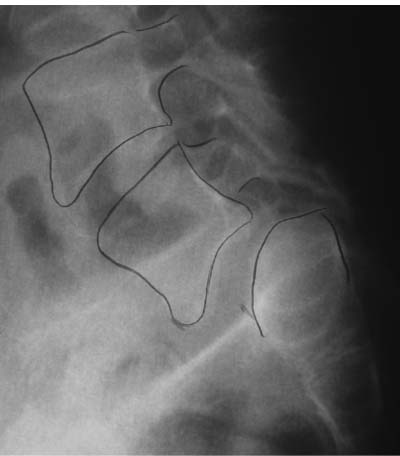
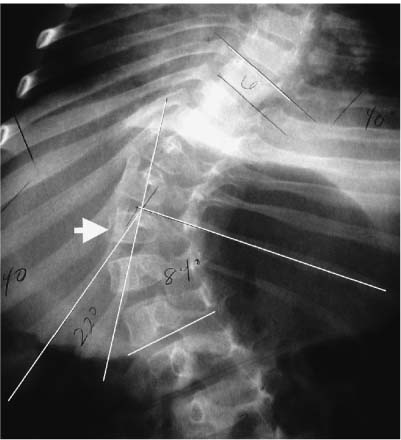
Chapter 5 Spinal deformity presents several treatment challenges to the spine surgeon. Surgical planning focuses primarily on the methods and maneuvers deemed necessary to correct coronal and sagittal imbalances. These methods iatrogenically alter the spatial relationships of the vertebrae to one another, the head, and the pelvis through corrective forces applied with implanted spinal instrumentation. Various forms are available, including screws, hooks, rods, and plates that can be inserted into the anterior or posterior elements through several different approaches. Among other factors, the relative safety and efficacy of instrumented correction of spinal deformity is influenced by the acceptability of the implants into or onto the vertebra. In their conception, spinal implants are designed in anticipation of normal anatomy. By definition, however, intervertebral relationships with spinal deformity are not normal. Furthermore, the morphology of the vertebral elements themselves is often abnormal, most characteristically exhibited as side-to-side asymmetry.1–6 To additionally complicate matters, these anatomical variants can cause deviant relationships of neural and vascular structures to the spinal column.7–9 With growing interest in the origin and treatment of spinal deformity, knowledge concerning associated anatomical variants has recently increased. It is the purpose of the authors to review this emerging body of literature. By offering the reader a more thorough understanding of potentially unusual anatomy, the spine surgeon may plan a more effective and safe treatment plan. In the thoracic spine, kyphosis normally ranges from 20 to 40 degrees. This is largely the result of gentle anteroposterior wedging of the thoracic vertebral bodies, in contrast with the lumbar spine in which normal lordosis ranging from 40 to 60 degrees is produced primarily by wedging of the disk spaces. By definition, Scheuermann’s kyphosis entails at least 5 degrees of kyphosis produced by pronounced sagittal asymmetry of three or more consecutive vertebral bodies (Fig. 5–1). Beyond diagnosing the disorder, the wedging of the vertebral bodies can have important intraoperative implications. When sizing and contouring anterior interbody devices, it should be recognized that after the hyperkyphosis has been corrected (usually through a posterior segmental construct), the intervertebral space will ultimately be trapezoidal, being much wider anteriorly than posteriorly. Figure 5–1 Lateral radiograph of a patient with Scheuermann’s kyphosis demonstrating the characteristically wedged vertebral bodies. Though they are not pathognomonic, another common feature of Scheuermann’s disease is the presence of end-plate deformities known as Schmorl’s nodes. It is believed they represent central herniations of disk into the vertebral body, possibly from weakening of the underlying cancellous bone. They can be readily recognized on plain films as radiolucencies within the vertebra surrounded by varying degrees of sclerotic bone.10 On magnetic resonance (MR) images, hypointensive (dark) disk material can be seen invaginating the vertebral body through the end plate. Surgically, Schmorl’s nodes represent a weakened end plate that may not survive aggressive maneuvers to remove the disk during fusion preparation. Care should be taken to avoid inadvertent curettage of the vertebral body during surgery. Isthmic spondylolisthesis can be associated with several anatomical variants, such as an elongated pars and incompetent posterior arch. The slipped vertebral body, most commonly L5, can have a trapezoidal shape (Fig. 5–2). It has been suggested that this is a reactive change to the inherent instability caused by incompetence of the posterior neural arch.11 The presence and degree of vertebral body wedging has been correlated with the grade or severity of the slip.12 The superior aspect of S1 often has an associated deformity in which the end plate is rounded or “domed.”11 It has been suggested that the aberrant morphology can contribute to the propensity of listhesis. In addition to possible prognostic significance, vertebral body malformation can have surgical implications. When performing interbody fusions, either from a posterior or anterior approach, it may be necessary to recontour the opposing end plates to better accept the flat surfaces of a bone graft strut or cage device. Figure 5–2 Isthmic spondylolisthesis can be associated with a wedge-shaped L5 vertebral body and a domed superior S1 vertebral body. This appears to be more common with high-grade slips. Although it is unclear whether it is a cause or effect,1 morphologic asymmetry exists among and within the individual vertebra of patients with idiopathic scoliosis.5,6,13 The vertebral body has been demonstrated to exhibit side-to-side asymmetry in patients with right thoracic scoliotic curves.14,15 This appears to be most pronounced at the apex of the curve.5 Others have suggested that sagittal asymmetry of the vertebral body also exists, finding that the apical thoracic vertebra can be lordotically wedged with anterior greater than posterior heights.16 Vertebral body asymmetry may in fact be a secondary effect of spinal deformity. In a longitudinal prospective study, Xiong et al.14 found that asymmetry tended to regress over a 2-year period after posterior segmental corrective surgery. Intraoperatively, morphological asymmetry of the vertebral body may have implications on insertion of vertebral body screws or interbody grafts. Rib deformities are associated with scoliotic curves. The intimate interaction of the posterior aspects of the ribs, both at the costovertebral and costotransverse junctions, make them obligatorily vulnerable to changes in spinal column alignment. Rib humps are primarily the result of rotation of the vertebral bodies and thus the associated ribs.17 The inter-costal space becomes narrowed on the concave side of the curve; inversely, they are widened along the curve concavity. Because the ribs are not rigidly fixed to the vertebrae, once they have abutted, increasingly severe curves will cause angling of the rib in relation to the vertebrae. This costovertebral angle (Fig. 5–3) has been used as an indicator of curve severity. In the minority of cases, the most prominent apical rib is associated with the most rotated apical vertebra; usually, it is either a level above or below.18 These anatomical considerations may be important when planning rib thoracoplasty or rib head resection. Pedicle screws have become an increasingly popular method of segmental fixation for spinal deformity correction. Pedicle screws are considered to be somewhat controversial in non-deformed spines; their insertion even more so in the deformed spine. Patients are typically younger, with smaller pedicular dimensions that may not be large enough to accept standardsized implants. To further complicate matters, pedicle morphology can be altered with spinal deformities, most notably idiopathic scoliosis.2,3,5,6,13,14,19 Figure 5–3 Anteroposterior radiograph that clearly demonstrates the differing rib-vertebral angles on either side of the curve in a patient with scoliosis. In patients with right-sided idiopathic thoracic scoliosis, Liljenqvist et al.5 found that the pedicles were significantly thinner on the concave side of the curve. Specifically, concave pedicles had transverse endosteal widths (the most useful measurement in relation to pedicle screw containment) measuring between 2.3 mm to 3.2 mm; on the convex side the range was between 3.9 mm to 4.4 mm. In the lumbar spine, the pedicles were roughly symmetric. In a previous study,6
Anatomical Variants with Spinal Deformity
♦ Vertebral Body
Scheuermann’s Disease
Isthmic Spondylolisthesis
Idiopathic Scoliosis
♦ Ribs
♦ Pedicles
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree