Anatomy of the Cervical Spine
John Louis-Ugbo
Frank X. Pedlow Jr.
John G. Heller
The neck is the anatomic region that lies between the lower margin of the mandible and the superior nuchal line of the occipital bone above and the suprasternal notch and upper body of the clavicle below (thoracic inlet). The neck (column) consists of a ventral region, the cervix, and a dorsal region or nucha. The neck supports the weight of the head and acts as a conduit for structures traversing to and from the cranial cavity, the thoracic cavity, and the upper extremities. The musculofascial arrangement of the neck allows for the protected passage of the blood supply to the head as well as to the upper respiratory and digestive tracts while also allowing complex motion of the head and neck and between the neck’s internal structures. The skin of the neck has constant natural lines of cleavage that run horizontally across the neck and incisions along these lines tend to result in narrow scars. The cervical spinal column serves to support the head; it allows motion in multiple planes and serves a protective function for the traversing spinal cord and nerve roots. An understanding of the regional anatomy and specific biomechanics of the cervical spine is relevant to the specific diseases that affect the region as well their treatment. This chapter reviews the osseous, ligamentous, muscular, nervous, visceral, and vascular anatomy of the region.
OSSEOUS ELEMENTS OF THE CERVICAL SPINE
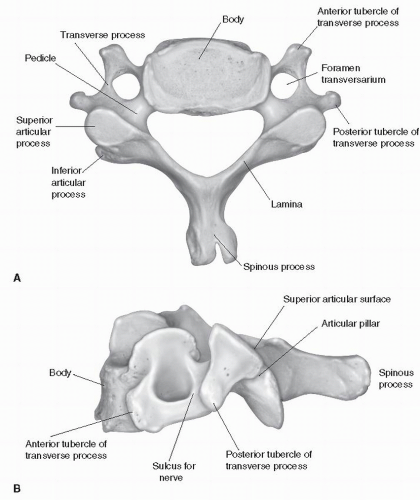
The cervical spine consists of seven vertebrae, which articulate with each other to form a strong pillar for the support of the head. The C1, C2, and C7 vertebrae present with exceptional or atypical features (atypical vertebrae), which are described below, while C3 through C6 (typical) vertebrae present with similar characteristics. A typical vertebra consists of two essential parts, namely, a ventral segment or vertebral body and a dorsal part, the vertebral or neural arch; these enclose a foramen, the vertebral foramen (Fig. 1.1). The spinal canal is formed by sequential vertebral foramina and is triangular with rounded edges. It has a greater lateral than anteroposterior (AP) width and is more spacious in the upper cervical spine, with sagittal diameters averaging 23 mm at C1 and 20 mm at C2. In comparison, the average diameter from C3 through C6 ranges between 17 and 18 mm and decreases to 15 mm at C7 (1). Thus, the cross-sectional area of the cervical spinal canal is greatest at C2 and smallest at C7. The vertebral arch consists of a pair of pedicles and a pair of laminae and supports seven processes, which include four articular, two transverse, and one spinous. The cervical vertebrae are the smallest of the true vertebrae and can be readily distinguished from those of the thoracic or lumbar regions by the presence of a foramen in each transverse process.
A typical cervical vertebra (Fig. 1.1) is characterized by the corpus vertebrae, pedicles, laminae, and spinous, articular, and transverse processes: A body or corpus vertebrae is the largest part of the vertebra and is cylindrical in shape. The upper surface is concave transversely and presents a projecting lip on either side. Its lower surface is convex from side to side and concave in the anterior-to-posterior direction, with the ventral lip of the concavity at times
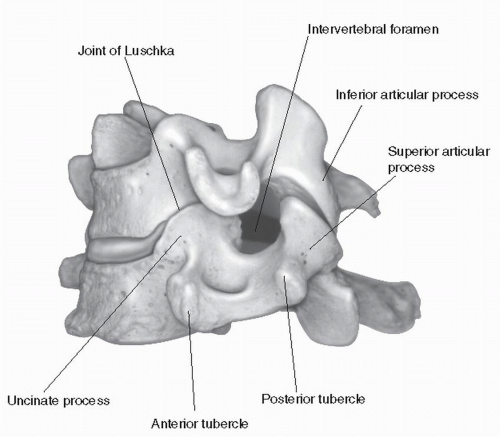
overlapping the vertebral body below, and it presents laterally shallow concavities that receive the corresponding projecting lips of the subjacent vertebra (2). The upper projection on the lateral superior surface of the caudal vertebrae is called the uncus (or hook) and is related intimately with the convex lateral inferior surface of the rostral vertebrae called the enchancure (anvil). These form articulations called the uncovertebral joints or joints of Luschka (Fig. 1.2). Ventrally, the body is convex from side to side and concave from above downward. Dorsally, it is flat from above
downward and slightly concave from side to side. The depth of the vertebral body at the inferior end plate is consistently larger than the depth of the superior end plate except at C7 (1). The upper and lower end plate width and depth increase from C2 to C7. The width ranges from 17 to 23.4 mm and depth ranges from 15.6 to 18.1 mm. Thus, the vertebral body width is usually greater than the corresponding depth. The vertebral body height on the dorsal wall in the midsagittal plane remains relatively constant from C3 through C7, ranging from 10.9 to 12.8 mm (2). Its ventral surface presents a few small apertures for the passage of nutrient vessels; on the dorsal surface is a single large, irregular aperture, or occasionally more than one, for the exit of the basivertebral veins from the body of the vertebra. The pedicles are two short, thick processes, which project backward, from either side of the vertebral body at the junction of its dorsal and lateral surfaces. From C3 to C7, the average pedicle height is 7 mm and the width 5 to 6 mm. From C3 to C7, the angle made by the pedicle with the sagittal plane decreases from 40 to 29 degrees (2). The concavities above and below the pedicles are named the vertebral notches, and when the vertebrae are articulated, the notches of each contiguous pair of bones form the intervertebral foramina.
overlapping the vertebral body below, and it presents laterally shallow concavities that receive the corresponding projecting lips of the subjacent vertebra (2). The upper projection on the lateral superior surface of the caudal vertebrae is called the uncus (or hook) and is related intimately with the convex lateral inferior surface of the rostral vertebrae called the enchancure (anvil). These form articulations called the uncovertebral joints or joints of Luschka (Fig. 1.2). Ventrally, the body is convex from side to side and concave from above downward. Dorsally, it is flat from above
downward and slightly concave from side to side. The depth of the vertebral body at the inferior end plate is consistently larger than the depth of the superior end plate except at C7 (1). The upper and lower end plate width and depth increase from C2 to C7. The width ranges from 17 to 23.4 mm and depth ranges from 15.6 to 18.1 mm. Thus, the vertebral body width is usually greater than the corresponding depth. The vertebral body height on the dorsal wall in the midsagittal plane remains relatively constant from C3 through C7, ranging from 10.9 to 12.8 mm (2). Its ventral surface presents a few small apertures for the passage of nutrient vessels; on the dorsal surface is a single large, irregular aperture, or occasionally more than one, for the exit of the basivertebral veins from the body of the vertebra. The pedicles are two short, thick processes, which project backward, from either side of the vertebral body at the junction of its dorsal and lateral surfaces. From C3 to C7, the average pedicle height is 7 mm and the width 5 to 6 mm. From C3 to C7, the angle made by the pedicle with the sagittal plane decreases from 40 to 29 degrees (2). The concavities above and below the pedicles are named the vertebral notches, and when the vertebrae are articulated, the notches of each contiguous pair of bones form the intervertebral foramina.
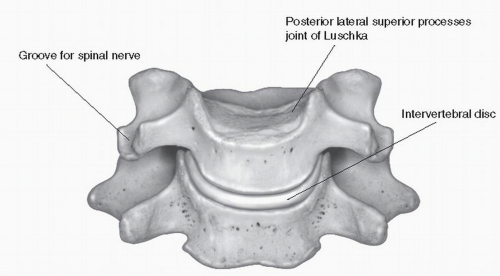 Figure 1.2. Lower cervical vertebra, showing joints of Luschka and their relation to disk, intervertebral foramen, and facets. |
The laminae that are thinner above than below consist of two broad plates directed dorsally and medialward from the pedicles and fuse in the midline to complete the vertebral or neural arch, along with the dorsal aspect of the vertebral body. Their upper borders and the lower parts of their ventral surfaces are rough for the attachment of the ligamenta flava. Cervical laminae are shorter and thinner but generally wider than those in the thoracic and lumbar spine. The laminar height (rostral-to-caudal distance) decreases from C2 to C4 and then progressively increases to C7. The minimum height at C4 is 10.4 ± 1.1 mm (3). The vertebral arch encloses the vertebral foramen that is triangular in shape and combines with foramina at other levels to form the spinal canal. The spinous process, which is short and bifid, projects downward and dorsally from the junction of the laminae and has two unequal processes, specialized for attachment of muscles and ligaments. Two superior and two inferior articular processes on either side fuse to form an articular pillar, which projects lateralward from the junction of the pedicle and lamina. The articular facets are flat and oval in shape: the superior projects backward, upward, and slightly medialward and the inferior forward, downward, and slightly lateralward (4).
The transverse processes project on either side from the point where the lamina joins the pedicle, between the superior and inferior articular processes. The transverse processes are each pierced by the foramen transversarium, which, in the upper six vertebrae, gives passage to the vertebral artery and vein and a plexus of sympathetic nerves. Each process has a ventral and a dorsal part. The ventral portion is a rib homologue; hence, it is called the costal process: it arises from the side of the body, is directed lateralward in front of the foramen, and ends in the anterior tubercle. The dorsal part, or true transverse process, springs from the vertebral arch behind the foramen and is directed forward and lateralward; it ends in a flattened vertical tubercle, the posterior tubercle. The anterior and posterior tubercles are joined, outside the foramen, by a costotransverse bar, which exhibits a deep sulcus on its upper surface for the passage of the corresponding cervical nerve root. It represents the most lateral aspect of the intervertebral foramen, which is bound superiorly and inferiorly by the pedicle, dorsally by the facets, and ventrally by the intervertebral disks, uncovertebral joints, and vertebral bodies (Fig. 1.3). The vertical diameter of the foramen is approximately 9 mm, the horizontal diameter is 4 mm, and the length ranges from 4 to 6 mm (5). Foramina exit at an angle of 45 degrees from the midsagittal plane. The costotransverse bar of the lower cervical vertebrae often has a middle scalene tubercle for attachment of a portion of the scalenus medius.
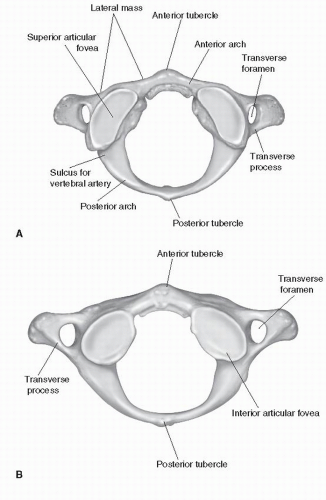
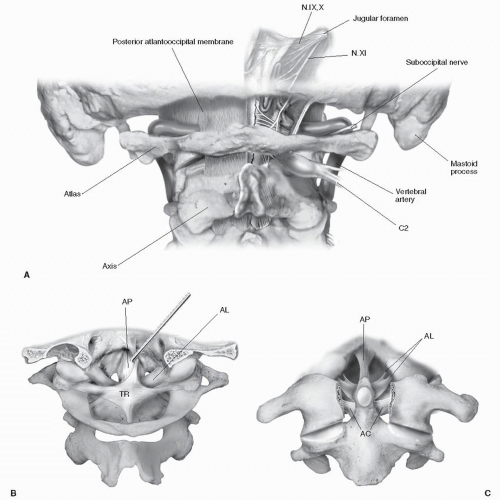
First cervical vertebra (atlas): The first cervical vertebra C1, or atlas, is a ring-shaped structure that articulates superiorly with the occipital condyles and inferiorly with the second cervical vertebra, the axis, via the atlantoaxial joints. Its peculiarities include the following: the absence of a vertebral body and spinous process, it is ring-like, and it consists of a ventral and dorsal arch and two lateral masses. It is the widest cervical vertebra, with its ventral arch approximately half as long as its dorsal arch (Fig. 1.4) Located in the midline on the ventral arch is the anterior tubercle for the attachment of the anterior longitudinal ligament (ALL) and the longus colli muscles. Its dorsal surface is concave and marked by a smooth, oval or circular facet (fovea dentis) for articulation with the odontoid process (dens) of the axis. The dorsal arch corresponds to the lamina of the other vertebrae, and it is usually less than 5 mm thick. On its upper surface is a wide groove for the vertebral artery and the first cervical nerve. The lower surface is notched, which contributes to the formation of the C2 intervertebral foramen. In 1% to 15% of the population, a bony arch may form, thereby converting this groove into the arcuate foramen, through which pass the same structures (6). The dorsal arch ends behind in the posterior tubercle, which is a rudimentary spinous process and gives origin to the rectus capitis posterior minor and attachment to the ligamentum nuchae. In up to 5% of the population, the dorsal arch of the atlas is incomplete (7), and recognition of this condition before surgical exploration is important to avoid inadvertent breach of the cervical spinal dura. The lateral masses of the atlas lie ventrally and medially, essentially forming a bony bridge between the atlantooccipital joint above and the atlantoaxial joint below. The paired foramina transversaria are located, in most instances, lateral to those found in the axis and below. The lateral masses of the atlas give rise to a superior and inferior articular facet. The superior articular facet is elongated and kidney shaped, facing inward and upward to support the occipital condyles, with which it articulates on each side. The inferior articular facets are flatter and more circular, facing downward and inward to articulate with the articular surfaces of the second cervical vertebra. The superior articular surfaces of the atlas point caudally from lateral to medial (average angle, 129.4 degrees), while the inferior articular surfaces angle cranially from lateral to medial (average angle,
130 to 135.8 degrees) (8,9) The transverse process is larger than that of other cervical vertebrae and is composed solely of a posterior tubercle that, with the costotransverse bar that attaches to the lateral mass, contains the foramen transversarium. The vertebral artery passes through the foramen transversarium of C1 before turning sharply medially and dorsally to course behind the superior articular process (5).
130 to 135.8 degrees) (8,9) The transverse process is larger than that of other cervical vertebrae and is composed solely of a posterior tubercle that, with the costotransverse bar that attaches to the lateral mass, contains the foramen transversarium. The vertebral artery passes through the foramen transversarium of C1 before turning sharply medially and dorsally to course behind the superior articular process (5).
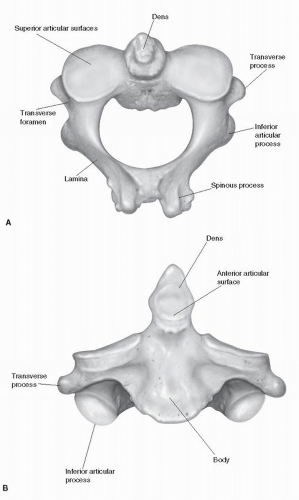
The axis or second cervical vertebra is also known as the epitrophysis because it forms the pivot upon which the first vertebra, carrying the head, rotates. It is characterized by a dens or odontoid process that projects upward from the body of C2 to articulate with the dorsal aspect of the ventral arch of C1 (Fig. 1.5). The dimensions of the dens are highly variable: Its mean height is 37.8 mm, its external transverse diameter 9.3 mm, internal transverse diameter 4.5 mm, mean AP external diameter 10.5 mm, and internal diameter 6.2 mm (10). Lateral to the dens, the body has facets that articulate with the lower surfaces of the lateral masses of C1, which are large, slightly convex, and face upward and outward. These are not true superior articular processes
because the articular surface arises directly from the body and pedicle lateral to the dens. The zone between the lamina and the lateral mass is not well defined and comprises a large pedicle that is 10 mm long and 8 mm wide (11). It projects superiorly and medially in a ventral direction. The lower surface of the lateral mass has forward-facing facets that articulate with the superior articular processes of C3. The large laminae of the axis slope caudally and laterally to the lateral masses, which often take on a more angled appearance when compared with those in the subaxial cervical spine. The spinous process is large and bifid and is often one of the largest in the cervical spine, is sometimes palpable through the skin, and can be useful for operative localization, especially after verifying that the atlas, which typically lacks any spinous portion, lies above. The transverse process ends in a single tubercle and contains a foramen transversarium. The C2 spinal nerve exits dorsal to the rostral articular surface of C2 rather than ventral to the articular complex as spinal nerves do at other levels. Large pedicles and a deeper spinal canal are two factors that allow increased mobility at C2 without cord encroachment. The density of the trabecular bone of C2 varies: It is very dense near the center of the tip of the dens and lateral masses beneath the superior articular surface and hypodense in the area of the trabecular bone immediately beneath the dens (8).
because the articular surface arises directly from the body and pedicle lateral to the dens. The zone between the lamina and the lateral mass is not well defined and comprises a large pedicle that is 10 mm long and 8 mm wide (11). It projects superiorly and medially in a ventral direction. The lower surface of the lateral mass has forward-facing facets that articulate with the superior articular processes of C3. The large laminae of the axis slope caudally and laterally to the lateral masses, which often take on a more angled appearance when compared with those in the subaxial cervical spine. The spinous process is large and bifid and is often one of the largest in the cervical spine, is sometimes palpable through the skin, and can be useful for operative localization, especially after verifying that the atlas, which typically lacks any spinous portion, lies above. The transverse process ends in a single tubercle and contains a foramen transversarium. The C2 spinal nerve exits dorsal to the rostral articular surface of C2 rather than ventral to the articular complex as spinal nerves do at other levels. Large pedicles and a deeper spinal canal are two factors that allow increased mobility at C2 without cord encroachment. The density of the trabecular bone of C2 varies: It is very dense near the center of the tip of the dens and lateral masses beneath the superior articular surface and hypodense in the area of the trabecular bone immediately beneath the dens (8).
The most distinctive characteristic of the seventh cervical vertebra is the existence of a long and prominent spinous process, hence the name vertebra prominens. This process is thick, nearly horizontal in direction, not bifurcated, but terminating in a tubercle to which the lower end of the ligamentum nuchae is attached. The transverse processes are of considerable size, their dorsal roots are large and prominent, while the ventral roots are small and faintly marked; the upper surface of each usually has a shallow sulcus for the eighth spinal nerve, and its extremity seldom presents more than a trace of bifurcation. The foramen transversarium may be as large as that in the other cervical vertebrae but is generally smaller on one or both sides; occasionally it is double, and sometimes it is absent. On the left side, it occasionally gives passage to the vertebral artery; more frequently the vertebral vein traverses it on both sides, but the usual arrangement is for both artery and vein to pass in front of the transverse process, and not through the foramen. Sometimes the ventral root of the transverse process attains a large size and exists as a separate bone, which is known as a cervical rib.
The cervicothoracic junction is a transitional region. At this level, the spinal canal decreases in size to the dimensions of the thoracic spine. The inferior articular process of C7 articulates with T1 to form a facet joint that is more thoracic in nature in that it is more perpendicular in the transverse plain. The seventh cervical vertebra also has a thinner lateral mass than other cervical vertebrae. The length, height, and width of the pedicles increase from C7 to T1 as the angle between the perpendicular of the dorsal aspect of the vertebral body and the axis of the pedicle decreases. An et al. (11) described the morphologic characteristics of the pedicles of C7, T1, and T2. The C7 pedicle has an average inner diameter of 5.2 mm in a mediolateral plane and an angulation medially in a posterior-anterior direction of 34 degrees. Xu et al. (12) found the thickness of the lateral mass of C7 to average 6.8 mm, with pedicular widths of 6.2 mm and height of 7 mm. They measured the angle between the pedicle axis and the dorsal aspect of the lateral mass to be 170 degrees in the transverse plane and 76.2 degrees in the sagittal plane (12). Jones and coworkers (13) found that cervical pedicle screws demonstrated a significantly higher resistance to pullout forces than did lateral mass screws. This variability in pedicle morphometry and orientation influences the capability of placing pedicle screws.
The occiput and occipital condyles are the paired lateral prominences of the occipital bone that form the foramen magnum together with the basioccipital segment ventrally and the supraoccipital (or squamosal) segment dorsally (14). The occipital condyles are commonly oval or bean shaped and slope inferiorly from lateral to medial in the coronal plane. The diameter of the foramen magnum is, on average, 3 cm, the same as the diameter of the cervical spinal canal at the atlas, and the distance between the midpoints of the condyles is approximately 4.5 cm (9) The condyles angle medially from dorsal to ventral, with an average angle of 55 degrees. Viewed from a dorsal viewpoint, they angle inferiorly and sit at a longitudinal angle of 117.5 degrees. Extending inferiorly from the occipital inion to the foramen magnum in the midline is a thickened, bony keel. It is important to note that, off the midline, the occipital bone is of inconsistent thickness, and biomechanical studies have demonstrated that screws placed in the keel have superior pullout strength compared with those placed laterally (15). The thickened portion of the keel extends laterally at the nuchal line, averaging 8 mm in thickness up to 2 cm from the midline; the width of this seemingly safe area for screw placement decreases caudally (16). Placement of occipital screws in the thickened midline keel can minimize the risk of breaching the inner cortex of the cranium.
The occipitoatlantal articulations are cup-shaped paired joints between the concave occipital condyles and the concave superior atlantal facets. Within the base of each occipital condyle, the hypoglossal nerve (cranial nerve [CN] XII), a meningeal branch of the ascending pharyngeal artery, and an emissary vein pass through the hypoglossal (ventral condyloid) canal. Ventral to the condyles, the condylar foramen carries anastomotic venous channels from the sigmoid sinus to the suboccipital venous plexus; dorsally, an indentation known as the condyloid fossa exists on the skull base. CNs IX to XI, the inferior petrosal sinus, the internal jugular vein, and the posterior meningeal artery travel lateral to the occipital condyles in the jugular foramen.
ARTICULATIONS OF THE CERVICAL SPINE
The cervical vertebrae are connected to one another and to the occiput by various joints and ligamentous structures. These structures combine to form distinct articular complexes at the atlantooccipital and the atlantoaxial levels. Intervertebral disks are located between the vertebral bodies of all cervical vertebrae except at C1 and C2 (Fig. 1.6). The craniovertebral junction is a complex region
that incorporates the occiput (Oc)-C1-C2 portions of the spine. It is a transition between the cranium and the mobile cervical spine. The bony confines of this region encompass the transition of the brainstem to the cervical spinal cord. This is the most mobile region of the cervical spine, and it functions as a “funnel” that is uniquely adapted to stability and motion. The Oc-C1-C2 complex is the most mobile portion of the cervical spine (Fig. 1.6).
that incorporates the occiput (Oc)-C1-C2 portions of the spine. It is a transition between the cranium and the mobile cervical spine. The bony confines of this region encompass the transition of the brainstem to the cervical spinal cord. This is the most mobile region of the cervical spine, and it functions as a “funnel” that is uniquely adapted to stability and motion. The Oc-C1-C2 complex is the most mobile portion of the cervical spine (Fig. 1.6).
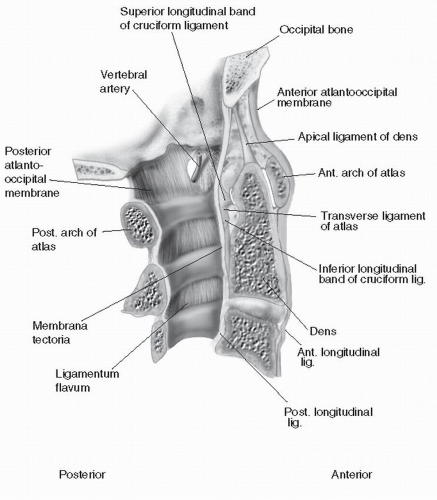 Figure 1.6. Median section at craniocervical junction, revealing atlantooccipital and atlantoaxial ligaments and membranes. |
The atlantooccipital complex is composed of two membranous attachments between C1 and the occiput and the two synovial atlantooccipital joints laterally. The atlantooccipital joints are formed between the superior articular facet of the atlas and the occipital condyle. These joints contain a synovial membrane and are surrounded by a capsular ligament. Also contributing to the complex are the anterior and posterior atlantooccipital membranes connecting the ventral and dorsal arch of C1 with the corresponding margin of the foramen magnum. The anterior atlantooccipital membrane blends on its lateral edges with the capsular ligaments of the synovial joints and inferiorly with the ALL. The dorsal atlantooccipital membrane blends laterally with the capsular ligaments of the synovial joints and is pierced on each side just above the dorsal arch of C1 by the vertebral artery in the first cervical nerve (Fig. 1.7). The primary movement at Oc-C1 is flexion and extension. Mean movement is 23 to 24.5 degrees. Flexion is limited by impingement of the tip of the dens on the foramen magnum, while extension is limited by the tectorial membrane. Lateral bending averages 3.4 to 5.5 degrees per side. This movement is resisted by the Oc-C1 articulation and the alar ligaments. Axial rotation is 2.4 to 7.2 degrees per side and is also limited by the Oc-C1 articulation and the alar ligaments (7,17)
The atlantoaxial complex is composed of three synovial joints, one median and two lateral (Fig. 1.7). The lateral atlantoaxial joints consist of encapsulated synovial joints between the inferior articular facets of C1 and the superior articular surfaces of C2. The capsules are reinforced dorsally by accessory ligaments that extend from the dorsal aspect of C2 rostrally and laterally to the lateral masses of C1. The median atlantoaxial joint forms between the ventral arch and transverse ligament of C1 and the dens. It is a pivot joint with synovial membrane and capsular ligaments ventral and dorsal to the dens. The cruciate (cruciform ligament) is composed of the transverse ligament of the atlas and the superior and inferior ligamentous extensions that connect it to the ventral edges of the foramen magnum and dorsal aspects of the C2 body, respectively. The transverse ligament attaches laterally to tubercles located on the dorsal aspect of the ventral arch of C1, where it blends with the lateral mass (Fig. 1.8) (18,19). The length of the transverse ligament averages 21.9 mm. Ventral sagittal translation is primarily limited by the transverse ligament, and secondary stabilizers include the alar and capsular ligaments. Sagittal translation is usually held to 3 mm or less in adults. The primary movement at C1-C2 is axial rotation. Mean rotational movement is 23.3 to 38.9 degrees per side (7). Movement is limited by the C1-C2
articulation, the ipsilateral transverse ligament, the contralateral alar ligament, and the capsular ligaments.
articulation, the ipsilateral transverse ligament, the contralateral alar ligament, and the capsular ligaments.
The axis has three other connections to the occipital bone (Oc-C2 complex). The apical ligament extends from the tip of the dens to the ventral edge of the foramen magnum and has an average length of 23.5 mm and a 20-degree ventral tilt (18). The alar ligaments extend from the tip of the dens to the medial aspects of each occipital condyle, with a small insertion also on the lateral mass of the atlas (19). They average 10.3 mm long. Sometimes there is a ligamentous connection between the base of the dens and the ventral arch of the atlas, called the anterior atlantodental ligament (19). The tectorial membranes extend from the dorsal body of C2 and the posterior longitudinal ligament (PLL) to the upper surface of the basilar portion of the occipital bone and the ventral aspect of the foramen
magnum. This membrane covers all other occipitoaxial ligaments as well as the dens. Thus, ventral to the spinal canal at the level of the craniocervical junction, the ligaments are arranged with the anterior atlantooccipital membrane most ventrally followed (in an anterior-to-posterior direction) by the apical alar, the cruciate, and, most dorsally, the tectorial (19).
magnum. This membrane covers all other occipitoaxial ligaments as well as the dens. Thus, ventral to the spinal canal at the level of the craniocervical junction, the ligaments are arranged with the anterior atlantooccipital membrane most ventrally followed (in an anterior-to-posterior direction) by the apical alar, the cruciate, and, most dorsally, the tectorial (19).
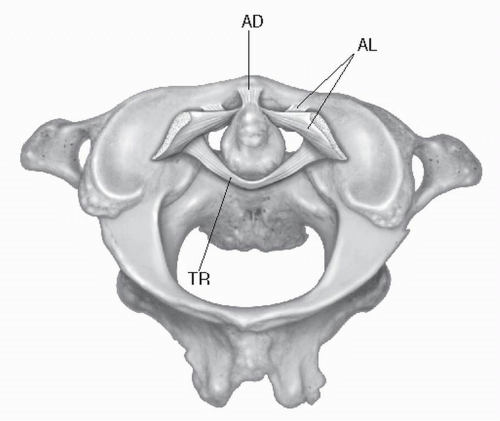 Figure 1.8. Axial view of cervicocranium from above, demonstrating the relations among the transverse (TR), alar (AR), and atlantodental (AD) ligaments. |
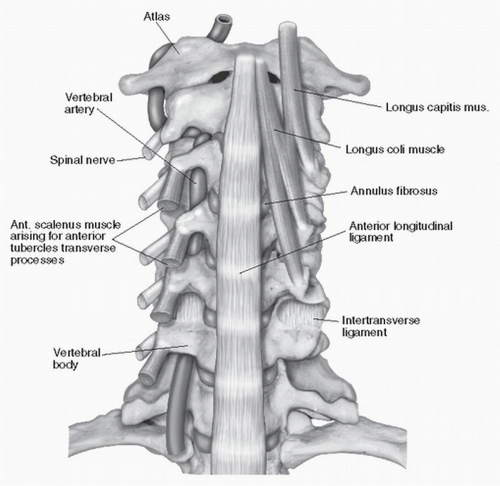
The bodies of the cervical vertebrae are connected by two longitudinal ligaments and the intervertebral disks. The ALL is a broad, thick ligament that runs longitudinally ventral to the vertebral body and disk (Fig. 1.9). It is joined loosely to the periosteum of the ventral vertebral bodies and closely to the annulus fibrosis of the anterior vertebral disk and attaches superiorly to the anterior tubercle of the atlas. The PLL lies within the vertebral canal on the dorsal aspect of the vertebral bodies and intervertebral disks. Superiorly, it is continuous with the tectorial membrane and thus attaches to the occipital bone and ventral aspect of the foramen magnum. As it descends, it narrows behind each vertebral body but spreads out at the disk level, where it is adherent to the annulus fibrosis. Hayashi et al. (20) described two layers: a superficial and deep layer. The deep layer surrounds the vertebral body and laterally is continuous with the lateral extension of the ALL in the intervertebral foramen. A more superficial layer is closely related to the dura mater and laterally separates from the deep layer, enveloping the dura mater, nerve roots, and vertebral artery. The venous plexus is located between the layers of the PLL—not in the epidural space, as previously thought (21).
The intervertebral disks are fibrocartilaginous joints that create shock-absorbing pads or cushions between the borders of adjacent cervical vertebrae, with the most cephalad disk at the C2-C3 level. Each disk consists of an inner nucleus pulposus surrounded by a circumferential annulus fibrosis; the border between the two becomes more difficult to distinguish with increasing age
and degeneration. These two components are separated from the vertebral bone above and below by a thin cartilage end plate. The nucleus pulposus is a semigelatinous central portion that contains collagen fibers, connective tissue cells, and cartilage cells with large amounts of amorphous extracellular material. It is held in shape by the cartilage end plates, the annulus fibrosis, and the uncovertebral joints laterally. The annulus fibrosis consists of spirally arranged and layered laminar collagenous fiber bundles with each ring of fiber arranged at right angles to the previous. The fibers are connected circumferentially to the vertebral end plate and to the anterior and PLLs. Dorsolaterally, the cervical disks are bound by the uncovertebral process, and inferiorly and superiorly the annulus fibrosis is firmly attached to adjacent vertebral end plates. End plates consist of a thin layer of hyaline cartilage resting on the subchondral bone of the vertebral body, which distributes stress over the body. The cartilage plays a role in the growth of the vertebral body and nutrition for the disk (22,23). Tanaka et al. (22) characterized the relation of the disk to the nerve root at the intervertebral foramen in the middle to lower cervical spine. At the entrance zone of the intervertebral foramen, the C4-C5 disk was most likely proximal to the C5 nerve root (33%) or just ventral to the C5 nerve root (67%). For the C5-C6 disk and the C6-C7 disk, the relation between the disk and the nerve root was most likely an axillary type (72% and 89%, respectively). With the C8 nerve root, 78% of nerve roots did not contact the C7-T1 disk at the entrance zone of the foramen but contacted the disk at the lateral exit zone of the foramen.
and degeneration. These two components are separated from the vertebral bone above and below by a thin cartilage end plate. The nucleus pulposus is a semigelatinous central portion that contains collagen fibers, connective tissue cells, and cartilage cells with large amounts of amorphous extracellular material. It is held in shape by the cartilage end plates, the annulus fibrosis, and the uncovertebral joints laterally. The annulus fibrosis consists of spirally arranged and layered laminar collagenous fiber bundles with each ring of fiber arranged at right angles to the previous. The fibers are connected circumferentially to the vertebral end plate and to the anterior and PLLs. Dorsolaterally, the cervical disks are bound by the uncovertebral process, and inferiorly and superiorly the annulus fibrosis is firmly attached to adjacent vertebral end plates. End plates consist of a thin layer of hyaline cartilage resting on the subchondral bone of the vertebral body, which distributes stress over the body. The cartilage plays a role in the growth of the vertebral body and nutrition for the disk (22,23). Tanaka et al. (22) characterized the relation of the disk to the nerve root at the intervertebral foramen in the middle to lower cervical spine. At the entrance zone of the intervertebral foramen, the C4-C5 disk was most likely proximal to the C5 nerve root (33%) or just ventral to the C5 nerve root (67%). For the C5-C6 disk and the C6-C7 disk, the relation between the disk and the nerve root was most likely an axillary type (72% and 89%, respectively). With the C8 nerve root, 78% of nerve roots did not contact the C7-T1 disk at the entrance zone of the foramen but contacted the disk at the lateral exit zone of the foramen.
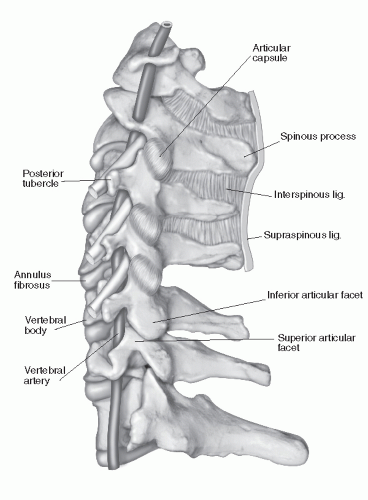 Figure 1.10. Lateral view of cervical spine, demonstrating facets and capsular and interspinous ligaments. |
The vertebral arches are connected by the synovial joints between articular processes of adjacent vertebrae and by the accessory ligaments between the laminae, the transverse processes, and the spinous processes (Fig. 1.10). The facet joints, or zygapophyseal joints, are diarthrodial joints with articular cartilage and menisci and are formed between the adjacent articular processes of sequential vertebral levels. Each zygapophyseal joint is surrounded by a fibrous capsule and is lined by a synovial membrane. Different types of menisci have been described in the cervical facet joints based on age, location, and degree of degeneration (24). Mechanical, receptive, and nociceptive nerve endings have been located in the facet capsules of cervical zygapophyseal joints (25). The facet joints of the cervical region are oriented more horizontally than those in other regions of the spine. The upper facet joints begin with an angle approximately 45 degrees superiorly in the transverse plane and gradually assume a more vertical position as they descend to the thoracic region. The superior articular facet faces from a generally more medial toward a lateral projection as the cervical spine is descended. Facet
widths increase from C3 to T1, with facet depth greatest in the upper three vertebrae and then decreasing from C5 to T1 (26). The interfacet distance varies between 9 and 16 mm (average, 13 mm). The capsular ligament of each facet is oriented dorsally at a 45-degree angle to the transverse plane (16).
widths increase from C3 to T1, with facet depth greatest in the upper three vertebrae and then decreasing from C5 to T1 (26). The interfacet distance varies between 9 and 16 mm (average, 13 mm). The capsular ligament of each facet is oriented dorsally at a 45-degree angle to the transverse plane (16).
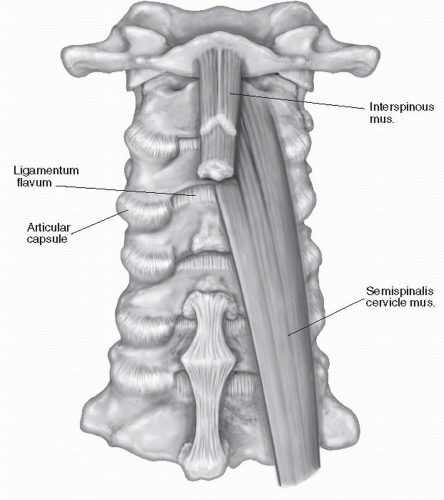 Figure 1.11. Posterior view of cervical spine, revealing ligamentum flavum as it blends into articular capsule of the facet joints. |
The supraspinous ligament of the thoracic region continues into the cervical region as the ligamentum nuchae. This is a triangular membrane that forms a median fibroseptum between the muscles of the two sides of the dorsal cervical region. It extends approximately from the external occipital protuberance to the spine of the seventh cervical vertebra. There are deep attachments to the external occipital crest, the posterior tubercle of the atlas, and the spinous processes of C2 through C7. The interspinous ligament is poorly developed in the cervical region and is found between the spinous processes from the ligamentum flavum to the tip of the process. It often has a thin, filmy appearance. The intertransverse ligaments between the transverse processes of the cervical spine are also weak and replaced by the intertransversalis muscles (27). The ligamentum flavum consists mainly of elastic fibers and connects the inferior and superior aspects of adjacent laminae, extending laterally to blend into the capsule of the facet joints (Fig. 1.11). The ligaments arise from the undersurface of the lamina above and insert on the superior edge of the lamina below. The ligamenta flava are discontinuous in the midline; the small fissure allows the exit of veins (27).
FASCIA AND MUSCULATURE OF THE CERVICAL SPINE
CERVICAL FASCIA
Deep to the skin of the cervical spine is the superficial fascia, which is continuous over the clavicle with the superficial fascia of the pectoral and deltoid regions. All fasciae deep to the superficial fascia are considered deep cervical fasciae. Deep to the superficial fascia, structures are anatomically compartmentalized by an organized deep fascia and potential interfascial spaces. This allows the complex motion and functions of the neck and its structures and allows dissection between fascial planes with an awareness of the structures that cross compartments. Descriptions and nomenclature vary in descriptions of the arrangement of fascial layers in the cervical spine (28, 29 and 30). In general, there are three principle fascial layers: a superficial, a pretracheal, and a prevertebral layer. In the ventrolateral aspect of the neck, where these layers are fairly associated with each other, they form the carotid sheath, the only paired compartment in the neck (30).
The superficial layer of cervical fascia surrounds all other fascial compartments in the neck. Superiorly, it is attached to the external occipital protuberance, the superior nuchal line, the ligamentum nuchae, and the spinous processes of the cervical vertebrae. Ventrally and medially, it is attached to the mastoid process and the lower border of the mandible as well as the zygomatic arch, the styloid process, and
hyoid bone. Its inferior attachments are to the clavicle, the sternum, the acromion, and the spine of the scapula. In its circumferential pattern, it divides to surround both the trapezius and the sternocleidomastoid and forms the roof of the posterior and anterior triangles of the neck. About the sternum, it divides into a superior and deep layer, which attaches to the front and back of the manubrium. The interval between these two fascial layers is termed the suprasternal space. The cutaneous nerves of the neck enter the superficial layer of cervical fascia at the dorsal border of the sternocleidomastoid. The major superficial veins of the neck run largely superficial to it (28,30).
hyoid bone. Its inferior attachments are to the clavicle, the sternum, the acromion, and the spine of the scapula. In its circumferential pattern, it divides to surround both the trapezius and the sternocleidomastoid and forms the roof of the posterior and anterior triangles of the neck. About the sternum, it divides into a superior and deep layer, which attaches to the front and back of the manubrium. The interval between these two fascial layers is termed the suprasternal space. The cutaneous nerves of the neck enter the superficial layer of cervical fascia at the dorsal border of the sternocleidomastoid. The major superficial veins of the neck run largely superficial to it (28,30).
The pretracheal layer of cervical fascia, or the middle layer of deep fascia, encases the infrahyoid or strap muscles of the cervical spine. It is the most ventral fascial compartment inside the outer investing layer of fascia and is just ventral to the visceral compartment of fascia. It joins the visceral fascia at musculature insertions. The pretracheal or visceral fascia surrounds the thyroid gland and forms its sheath. It surrounds the trachea and esophagus as well as the larynx and pharynx. At approximately the level of C6, the larynx meets the trachea and the pharynx meets the esophagus. The retropharyngeal space is the space located between the prevertebral and visceral fascia at the pharyngeal level (30).
The prevertebral or deep layer of the deep cervical fascia encases the cervical spine and all musculature ventrally and dorsally associated with its movements. Dorsally, it is attached to the ligamentum nuchae in the midline. Ventrally, it is attached to the ALL of the ventral cervical spine and covers the longus capitis and colli muscles. Some authors refer to an additional fascial layer, the alar fascia, located ventral to the vertebral bodies between the prevertebral and pretracheal fascia. Laterally, the prevertebral fascia encases the scalene muscles and attaches to the transverse processes of the cervical vertebrae and also forms the floor of the posterior triangle. As the brachial plexus and the subclavian artery course toward the axilla, they are encased within a prolongation of the prevertebral fascial layer, which forms the axillary neurovascular sheath (30,31). Superiorly, the prevertebral fascia attaches to the external occipital protuberance, the superior nuchal line, the mastoid process, and the base of the skull. Inferiorly, it attaches to the outer aspects of the first and second rib in the thorax and the pleural dome.
The carotid sheath is a condensation of connective tissue that encases the carotid artery, the internal jugular vein, and the vagus nerve. It is located lateral to the visceral compartment and ventral to the prevertebral fascial compartment. The carotid sheath is fused with the investing fascia ventrally and ventromedially it is fused with the pretracheal fascia. Dorsally, it has a loose attachment with the prevertebral fascia. Branches of the external carotid artery leave the carotid sheath starting at the level of the upper border of the thyroid cartilage. The superior laryngeal branch of the vagus nerve travels behind both carotid arteries before leaving the carotid sheath and traveling to the visceral fascia and eventually dividing into its terminal branches. The hypoglossal nerve passes superficial to both carotid arteries, whereas the glossopharyngeal nerve passes between the carotid arteries, penetrating the carotid sheath. The cervical sympathetic chain is located on the longus colli and is related to the dorsal surface of the carotid sheath; it is imbedded in the prevertebral fascia (30,31).
Fascial spaces in the neck vary in their description in various literatures (30). The potential space in front of the trachea and behind the infrahyoid muscles and pretracheal is usually called the pretracheal space. It is limited above by the attachment of fascia and muscles to the thyroid cartilage and below by blending with the ventral mediastinum fascia. The retropharyngeal space lies behind the esophagus and ventral to the prevertebral fascia. It extends above to the base of the skull and below to the dorsal mediastinum; thus, infections originating from the pharynx or cervical vertebral bodies or disks can travel into the thoracic cavity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree