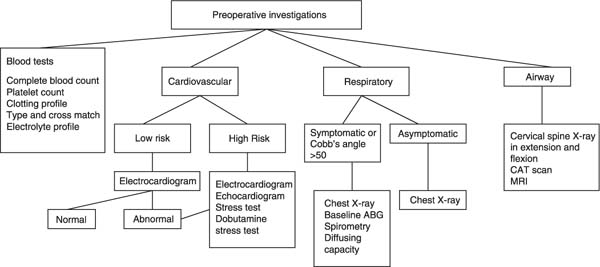
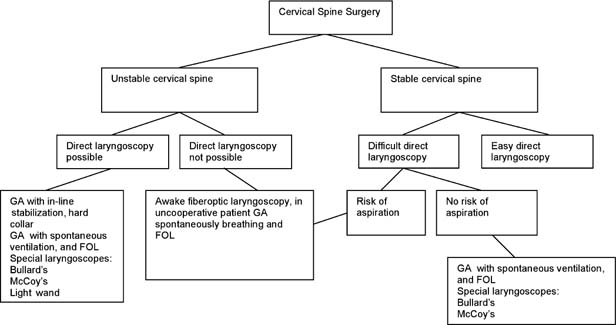
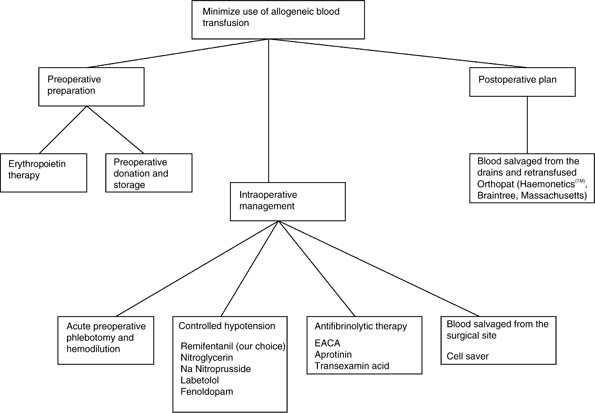
Chapter 3 This chapter reviews the critical considerations and anesthetic practices for major spine surgery. Anesthesia for spine surgery presents challenges regarding positioning, blood loss, and postoperative complications including blindness. Depression, anxiety, and fear are known to contribute to the overall experience of “pain” surrounding the perioperative period.1 A guide to a preoperative workup based on symptoms, preexisting diseases, and the extent of surgery necessary is outlined in Fig. 3–1. Harris et al.2 investigated the clinical factors associated with unexpected critical care management and prolonged hospitalization after elective cervical spine surgery in a retrospective, case controlled study of 109 patients. They found that 15% required critical care management in the early postoperative phase. Patients needing critical care had a greater incidence of preexisting myelopathy and a larger extent of decompression (2.38 levels). The presence of pulmonary disease, hypertension, cardiovascular disease, and diabetes mellitus all were associated with the need for critical care management and longer hospitalization. Interestingly, smoking was not associated with the need for postoperative critical care in this study. Thoracic spine surgery involving either or both an anterior and posterior approach, especially when the thoracic cavity is invaded, is often associated with postoperative radiographic abnormalities of the lungs.3 Figure 3–1 Guidelines for preoperative workup prior to spinal instrumentation. Figure 3–2 illustrates the decision-making tree for intubation. Whatever decision is made, the patient is well informed about the plan in advance. Recognizing the potential for instability and inserting the endotracheal tube with care, while avoiding spinal movement, appears to be more important than any particular mode of intubation in preserving neurologic function. Popitz4 proposes observing the neck posture while the patient is walking and upon sitting (in a neutral relaxed position), noting the fluidity of head and neck movements. A patient with cervical spine pathology may maintain his or her head in a relatively stiff posture due to muscle spasm or bony fusion. Instead of rotating the head toward the examiner, such a patient might rotate the whole upper body. After ascertaining that the patient has no history of neurovascular symptomatology with neck rotation or lateral flexion (as may occur with vertebrobasilar disease), active examination can begin. In patients with an unstable cervical spine, the passive range of motion of the neck should not be examined. The neck is inspected for normal position and midline alignment of the hyoid bone, thyroid cartilage, and the spinous processes. It is also examined for loss of the normal cervical lordosis and for the presence of scoliosis.4 Crosby and Lui5 reviewed 30 years of medical literature, with emphasis on the last 10 years of management of the airway in patients with unstable cervical spines. Relevant papers were selected from anesthetic, orthopaedic, rheumatologic, emergency medicine, and trauma journals. Relevant findings included the high prevalence of cervical spinal instability in trisomy 21 and rheumatoid arthritis and the relatively low incidence after trauma. Their conclusion was that with recognition of the potential for instability, performing intubations with care, while avoiding spinal movement, appeared to be more important than any particular mode of intubation in preserving neurologic function. Awake fiberoptic intubation is the technique of choice for an unstable cervical spine, prior history of difficult intubation, or the presence of a halo that complicates maintenance of a good airway. The patient should be premedicated with glycopyrrolate 0.2 mg to dry secretions. The airway is anesthetized with nebulized 4% lidocaine over 20 to 30 minutes to achieve adequate topical anesthesia with good sedation. Supplemental topical anesthesia of the oropharynx can be added with viscous lidocaine gargles and lidocaine ointment applied to the posterior part of the tongue. The nasopharynx can be anesthetized with either cocaine 4% or a combination of neosynephrine and lidocaine packing. Figure 3–2 Strategy for tracheal intubation in patients with potential cervical spine injuries. FOL, fiberoptic laryngoscopy; GA, general anesthesia. Titration of small amounts of midazolam and fentanyl can provide adequate sedation. Recently, remifentanil or dexmedetomidine have been reported to provide adequate sedation for awake fiberoptic intubations.6–8 Patients with unstable spines who are not cooperative or any patient with an unanticipated difficult airway who does not have an increased risk for gastric aspiration can be safely managed by unconscious fiberoptic intubation. All patients whose airway is anticipated to be normal or those with in-line stabilization or with a hard collar in place can be intubated safely after direct laryngoscopy after induction of unconsciousness. Nakazawa8 et al. investigated the utility of the intubating laryngeal mask airway (ILMA; LMA-Fastrachtrade, Laryngeal Mask Company, Ltd., Henley on Thames, UK) for blind endotracheal intubation in patients undergoing cervical spine surgery. They found that intubation was successfully achieved in only 82% of cases. All of these patients eventually underwent tracheal intubation using a fiberoptic bronchoscope through the ILMA. The vocal cords were fully viewed with the fiberoptic bronchoscope from the aperture of the ILMA in those cases. Postoperative sore throat and hoarseness occurred in 32.5% and 22.5% of patients, respectively, and, in all cases, these were transient. Three patients exhibited severe pharyngeal edema postoperatively. They recommended awake fiberoptic bronchoscopy as a first choice for patients with cervical spine disease with predicted difficult intubation. Patients with rheumatoid arthritis may have various forms of atlantoaxial subluxation, temporomandibular ankylosis reducing the mouth opening, and chronic cricoarytenoiditis that predispose to acute airway obstruction during intubation and extubation. Direct laryngoscopy should be avoided with known posterior and vertical atlantoaxial subluxations, whereas anterior, lateral, and rotator subluxations can tolerate direct laryngoscopy after stabilization of the neck.9 Different laryngoscope blades have been studied to determine cervical spine movement during direct laryngoscopy. They include Macintosh, Miller, McCoy10 and Bullard laryngoscopes.11 Bullard causes significant reductions in radiographic cervical spine extension as compared with the Macintosh blade. Several techniques have been described for facilitating endotracheal intubation. Saha et al.12 found the Lighted Intubating Stylet (LIS) device to be significantly faster than the fiberoptic bronchoscope for performing endotracheal intubation in awake patients with cervical spine injuries. Other devices have been tried to minimize cervical spine movement including a newly designed light wand device Trachlighttrade?(Laerdal, Armonk, New York). An intra-arterial catheter is indicated where there is greater than 20 mL/kg of blood loss expected. Additionally, to minimize intraoperative blood loss, the use of controlled hypotension mandates the use of continuous blood pressure monitoring. Frequent blood gas monitoring for acid-base balance and serial hematocrits is important for controlled hypotension. For patients having scoliosis surgery with a likelihood of significant blood loss, or for patients in whom hemodynamic changes are especially threatening because of coincident cardiovascular disease, central venous pressure (CVP) monitoring is used. CVP is a direct measure of pressure, not volume. However, pressure is assumed to reflect the ratio of blood volume to vascular compliance, and it is a way to assess “relative blood volume” in patients who are either critically ill or undergoing major surgery. Recently, Munis et al.13 validated the use of peripheral venous pressure (PVP) as a useful monitor, which correlates highly with changes in absolute blood volume. There are three main methods of neurophysiologic monitoring: the Stagnara wake-up test, somatosensory evoked potentials (SSEPs), and motor evoked potentials (MEPs). A multi-center survey conducted by the Scoliosis Research Society involving more than 51,000 surgeries14 showed that 0.127% of patients (64) had postoperative neurological deficits in spite of unchanged intraoperative sensory evoked potential (SEPs). In the same study, the rate of true-positive results (0.423%) represented the cases in which SEPs documented but did not prevent (or only partially prevented) a neurologic deficit. SEP recording relies on the averaging of responses. This delays the acquisition of a reliable signal and could delay the implementation of corrective measures that can be taken in time to reverse an injury to the spinal cord. Because neurogenic motor evoked potentials (NMEPs) can be recorded with fewer averaged trials, they provide a chance for prompt feedback to the surgeon. For this reason, the use of only SEPs for monitoring the functional integrity of the entire spinal cord is no longer considered sufficient.15 Pelosi et al.16 reported MEP and SEP monitoring in 97 patients for spinal orthopaedic operations. The majority of patients (81%) underwent surgery for correction of spinal deformity. The Stagnara wake-up test appears to add no useful information to combined MEP and SEP monitoring (i.e., there are no false negatives reported with combined SEP/MEP monitoring). Because MEPs can activate the muscles of mastication, use of a bite block or tongue padding is recommended to prevent injury to the tongue and teeth. Our preference for intraoperative anesthetic management is total intravenous anesthesia (TIVA) with concomitant use of neurophysiologic monitoring. Stable anesthesia is required so that changes to SEPs or MEPs can be interpreted reliably. A technique involving nitrous oxide 60% and isoflurane less than 0.5 minimum alveolar concentration of potent inhalation agent (MAC) is compatible with SEP monitoring but may make MEP monitoring uninterpretable. Our preference is to combine propofol with an infusion of remifentanil. In clinical trials, where patients received remifentanil for periods up to 16 hours, recovery from anesthesia was rapid, predictable, and independent of the duration of the infusion of remifentanil.17 In the seven controlled, general surgery studies, extubation occurred in a median of 5 minutes. Remifentanil can also be used for controlled hypotension and is preferred due to its lack of interference with MEPs. Intraoperative communication with the neurophysiologist is imperative. Sudden cardiovascular instability during anesthesia may result from spinal cord and brain stem reflexes, from mediastinal distortion as a result of surgical manipulation, or more commonly from blood loss, influencing SEP/MEP recordings. During extensive spinal surgery, blood loss can be considerable with typical losses of 10 to 30 mL/kg from decorticated bone and disruption of rich vascular networks. The degree of blood loss is associated with: the number of spinal levels fused,18 body weight, surgery for tumors, and raised intraabdominal pressure in the prone position.19 A strategy to conserve allogeneic blood transfusion is adopted early at the inception of planned surgery. See Fig. 3–3 for a strategy for preoperative, intraoperative, and postoperative blood conservation plan. Figure 3–3 Strategies to minimize use of allogeneic blood transfusion. Several strategies can be adopted to conserve transfusion of allogeneic blood as outlined in Fig. 3–3. A recent analysis20 from Europe retrospectively reviewed the hospital charts and blood bank records from all consecutive spine surgery patients who were referred for predonation (PD) of blood. The data were collected from 1995 to 2003. Fifty-four (7%) out of 763 patients referred for PD were rejected, and medical records were available for 680 patients who were grouped into spinal fusion (556; 82%) and scoliosis surgery (124; 18%). Recombinant erythropoietin (EPO) was administered to 120 patients (17.6%). From 1995 to 2003, PD steadily increased from 60 to 209 patients per year. Ninety-two percent of the patients were able to complete PD, 71% were transfused, and almost 80% avoided allogeneic blood transfusion. PD was more effective in fusions (86%) than in scoliosis (47%). Blood wastage was 38%, ranging from 18% for scoliosis to 42% for fusions. EPO improved the preoperative hemoglobin levels. The authors conclude that despite the limitations of the retrospective study, PD was an excellent alternative to allogeneic transfusion in spine surgery, and the effectiveness of PD could be enhanced if associated with other blood-saving techniques such as EPO. PD has been shown to reduce the requirement for allogeneic blood by up to 75% in lumbar fusion surgery.21 Disadvantages of this method include repeated visits for preoperative phlebotomy, wastage of unused blood, high cost, and possible risks of incompatibility because of clerical errors. Autologous blood donations are indeed advantageous in decreasing allogeneic blood usage of patients undergoing fusion, but additional methods of blood conservation (intraoperative salvage and preoperative EPO) seem necessary to diminish the allogeneic blood requirements further, especially in those patients undergoing instrumentation and fusion. EPO is a 34-kDa glycoprotein whose primary function is the regulation of erythrocyte production. It is essentially lineage-specific in its effects on red blood cells (RBC).22 The use of EPO to prime for autologous RBC donation has been perceived as a major step toward reducing the risks associated with blood transfusions. The use of EPO preoperatively has been demonstrated to promote an increase in the number of autologous units of blood donated. Shapiro et al.23 demonstrated that preoperative autologous donation was completed more effectively in the 24 patients receiving EPO studied prospectively. They reported statistically higher hematocrit levels during preoperative autologous donation and perioperatively (p 0.005). Homologous transfusion was decreased by 2.4 units, and hospital stay was 1.8 days shorter in patients receiving EPO in doses of 40,000 U at the time of each predonation over 4 weeks. EPO therapy has also been successfully used in children of median age 15.4 years undergoing corrective spinal surgery to facilitate autologous blood collections.24 Controlled hypotension has been used for minimizing blood loss in the past. However, a decrease in systemic blood pressure reduces spinal cord perfusion pressure. Additionally, recent published cases describing the occurrence of blindness after spinal surgery have highlighted the potential risks of deliberate hypotension. Hypotension has been shown to increase the likelihood for neurologic deficits and altered evoked potential signals in both animal and clinical settings. Hypotension may induce spinal cord ischemia even without spinal cord manipulation. Lyon et al.25
Anesthesia in Spinal Deformity Surgery
♦ Preoperative Evaluation
♦ Intubation Prior to Cervical Spine Surgery
Awake Fiberoptic-Guided Intubation
Unconscious Fiberoptic-Guided Intubation
Unconscious Direct Laryngoscopy
Intubating Laryngeal Mask Airway
Airway Management in Patients with Rheumatoid Arthritis
Other Options for Intubation
♦ Intraoperative Monitoring
Blood Gas and Blood Pressure Monitoring
Neurophysiologic Monitoring
♦ Anesthetic Management
Techniques to Minimize Use of Allogeneic Blood Transfusion
Preoperative Donation and Erythropoietin
Intraoperative Strategies
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree