♦ Preoperative
Imaging
Computed Tomography Scan/Computed Tomography Angiogram
- Confirm evidence of subarachnoidal hemorrhage (SAH) in patients with a suspected aneurysmal bleed.
- In ruptured aneurysms evaluate for hydrocephalus. Rationale: Operating on patients with untreated hydrocephalus will increase the complication rate (contusions, intracranial hemorrhages [ICHs]) related to traction; therefore, treat preoperatively and intraoperatively with ventricular or spinal drain.
- In ruptured aneurysms evaluate for an intracerebral hemorrhage. Rationale: Confirm site of hemorrhage (e.g., gyrus rectus, intrahemispheric for anterior communicating [ACOM] aneurysms) and evaluate for need to remove ICH at the time of clipping.
- In both ruptured and unruptured aneurysms, look for evidence of calcification of the aneurysm. Rationale: This may imply that simple clipping may not be possible due to calcification of the neck. Consider preparing for cerebral bypass.
- Evaluate aneurysm configuration on three-dimensional (3D) reconstructions. Rationale: May obviate need for digital subtraction angiography in operative planning in select cases (large ICH requiring emergent evacuation or 3D reconstruction of particularly good quality).
Digital Subtraction Angiogram
- Confirm evidence of aneurysm.
- Document size. Rationale: Increased size is associated with increased complications and giant aneurysms (> 2.5 cm) occasionally require additional measures to treat aneurysm. Very large aneurysms with no calcification or intra-aneurysmal thrombus may need and/or benefit from adenosine cardiac arrest to collapse aneurysmal wall to facilitate clipping, if temporary clipping not possible because of its size. Giant aneurysms with a large amount of calcification or intra-aneurysmal thrombus may need or benefit from cardiac arrest to collapse wall and remove thrombus to facilitate clipping.
- Determine A1 dominance. Rationale: The aim is to approach aneurysm toward the neck and not the dome. As the aneurysm usually points away from the dominant side, this also allows for intraoperative control (temporary clipping of dominant A1) in case of premature rupture.
- Determine direction of aneurysm projection. Rationale: In addition to what is discussed previously, certain projections require additional thought. Inferior projection requires extra care in frontal retraction to avoid rupture, early gyrus rectus resection may lessen tension on the aneurysm during retraction, and the aneurysm dome may obstruct view of contralateral A1. Superior projection requires the preparation of fenestrated clips because these aneurysms often project posteriorly and often have a broad neck; placement of a straight clip risks damage to the ipsilateral A2 segment; and orbitozygomatic approach may also be required to reduce brain retraction.
- Mayfield head holder, major craniotomy tray, high-speed drill, preferred retractor system, permanent and temporary aneurysm clips in a variety of shapes and sizes, bayonet scissors, microsuckers, and Rhoton dissectors (Codman)
Operating Room Set-up
- Intraoperative angiography used for most ACOM aneurysms
Anesthetic Issues
- Perioperative antibiotics half hour prior to incision. Rationale: Prevents infection.
- Anticonvulsant therapy: maintenance or load with intravenous (IV) phenytoin 18 mg/kg. Rationale: Prevents postoperative seizure.
- Hyperventilation to pCO2 28 to 32 mm Hg. Rationale: Allows for further brain relaxation to prevent retraction injuries.
- IV mannitol 1 g/kg at skin incision. Rationale: Relaxes the brain, facilitates elevation of bone flap, and prevents retraction injury.
- Management of blood pressure: avoid hypertension and hypotension except in special situations. Rationale: Helps prevent a rehemorrhage or hemorrhage. In poor grades and those with vasospasm, maintain moderate hypertension (systolic blood pressure 140 to 160 mm Hg) after clipping. During temporary clipping, moderate hypertension is also preferred to increase collateral circulation.
- Choice of anesthetic agents: in unruptured or grade one SAH patients with a slackened brain, most agents can be used. In poor grades, or those with brain swelling, IV agents such as propofol should be used with limitation of inhalation agents. Rationale: Prevents retraction injury and facilitates operative exposure.
- Use cerebral protection: barbiturates, propofol, and mild hypothermia (33° to 35° C) during temporary clipping. Rationale: Prevents ischemic complications.
♦ Intraoperative
Cerebrospinal Fluid Drainage
- Lumbar drain for all cases; ventricular drainage for those ruptured aneurysm patients with hydrocephalus. Rationale: Facilitates brain relaxation and prevents retraction injury.
Positioning
- Patient should be positioned supine, with head elevated and fixed in Mayfield skull clamp, and rotated 45 degrees away with the malar eminence being the highest point. This ensures venous drainage is not compromised.
- Electric bed allows for repositioning for surgeon’s comfort and approach.
- Standard pterional skin incision with interfascial or subfascial technique to preserve frontalis branch of the facial nerve.
- Perform supraorbital craniotomy. This is similar to a standard pterional craniotomy except that the frontal exposure goes to the supraorbital notch. After stripping the dura from the orbital roof and sphenoid wing, the orbital roof is drilled away until a thin egg shell remains over the orbit. The sphenoid wing is also drilled away until the superior orbital fissure is exposed. Rationale: This allows for less brain retraction because of a larger working space.
- In large aneurysms, in particular superior pointing aneurysms, remove the orbit either alone or as part of an orbitozygomatic craniotomy. Rationale: This allows for more working space, in particular allowing the surgeon to look more superiorly with less brain retraction.
- After a C-shaped dural opening, protect the brain with a nonstick substance (i.e., Telfa) and place self retaining retractor on frontal lobe at junction of olfactory and optic nerves. A small temporal retractor may also be placed.
- Arachnoid is then opened over the ipsilateral optic nerve and expanded to free the optic nerve, expose the carotid artery, and split the sylvian fissure inside out until the ipsilateral A1 is identified. This allows for temporary clipping in case of premature rupture.
- Resect the gyrus rectus by cauterizing and incising the pia medially and parallel to the olfactory nerve, and then perform a subpial resection of the gyrus until the ipsilateral A1 and A2 are exposed. Bleeding must be controlled with Surgicel and not cautery to prevent an inadvertent perforator injury, such as Heubner.
- Place a frontal retractor medially into the cavity just superior to the A1. Pia can then be bluntly dissected off the ipsilateral A1 and A2.
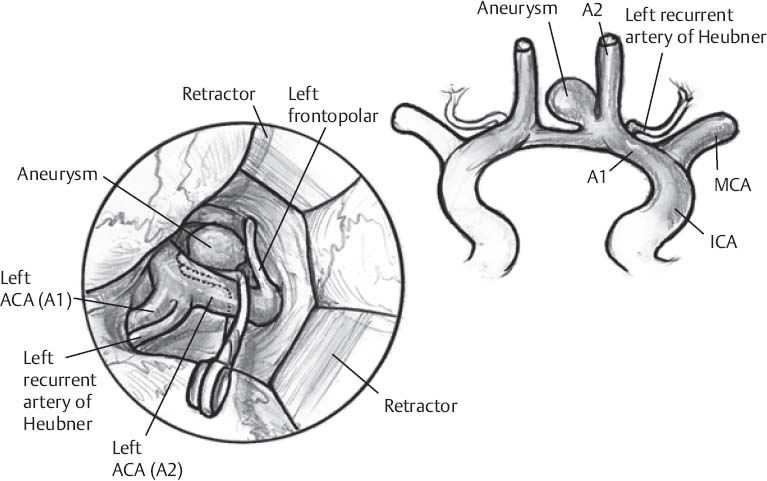
- Dissect the aneurysm neck safely. This is done by understanding the 3D anatomy and, most importantly, the direction the aneurysm points (Fig. 21.1). Always dissect away from the direction of the dome (e.g., with superiorly pointing aneurysms) and dissect the inferior wall of the ACOM first; for inferiorly pointing aneurysms, dissect the superior aspect of the ACOM first. Rationale: This will prevent rupture of the aneurysm during early dissection.
- Once the aneurysm neck is exposed, expose the contralateral A1 and A2 (Fig. 21.1). Rationale: To prevent inadvertent occlusion with the aneurysm clip, these must be well visualized prior to clip placement.
- Prepare the aneurysm neck for clipping by understanding the local anatomy; that is, know the location and orientation of the A1s, A2s, recurrent arteries, and perforators to prevent an inadvertent occlusion. Decide on the type of clip that is going to be required to achieve the goal of excluding the aneurysm from circulation while preserving patency in all other vessels.
- Clip the aneurysm with a blade that is long enough to exclude the aneurysm while not inadvertently clipping normal vessels. Also, always clip parallel to the communicator, as this will prevent kinking of the A2 and a postoperative stroke. Occasionally, a fenestrated clip must be used over the ipsilateral A1 or A2, particularly in a superiorly pointing aneurysm (Fig. 21.1).
- Confirm adequate clipping and filling of normal vessels with intraoperative Doppler and intraoperative angiography prior to a standard closing.
Only gold members can continue reading. Log In or Register to continue








