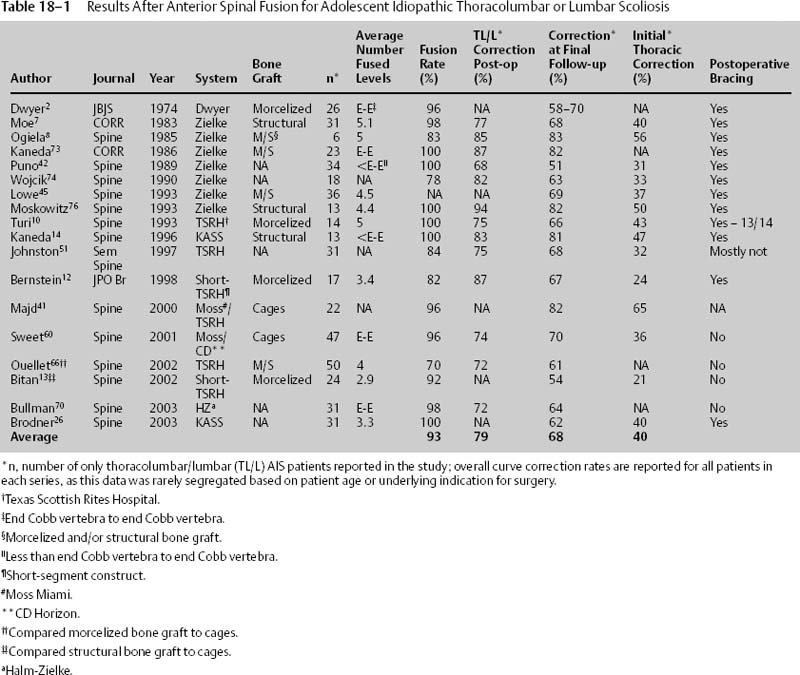
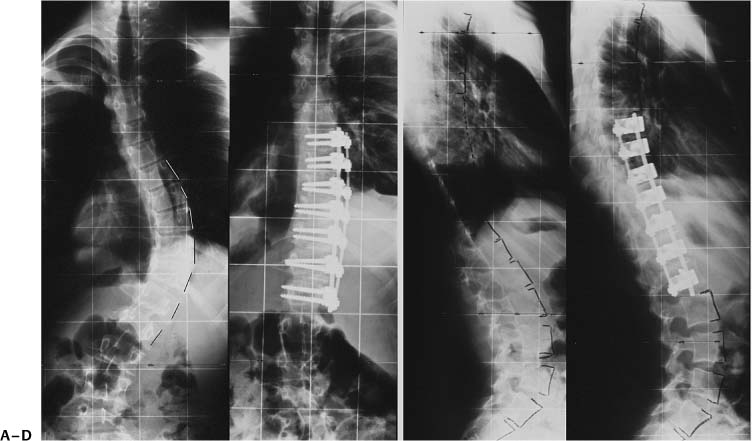
Chapter 18 In 1964, Dwyer was the first to perform an instrumented anterior spinal fusion (ASF) for scoliosis.1 Subsequently, he reported similar coronal correction of thoracolumbar and lumbar curves after ASF to that achieved with posterior spinal fusion (PSF) using Harrington’s technique.2,3 However, this system, which consisted of screws that were connected via a flexible titanium cable, provided insufficient rigidity and resulted in high rates of hardware failure and pseudarthrosis.1 Further, it proved to be kyphogenic. In the 1970s, Zielke improved on Dwyer’s technique by exchanging the titanium cable for a semirigid rod.4–6 Consequently, the bicortical screws (Dwyer’s original method) could now be more rigidly connected, thus permitting optimization of Zielke’s “ventrale derotations-spondylodese” technique. This technique advocated anterior translation and derotation of the apical vertebra, thus resulting in improved “lordisation” of the lumbar curve by converting a coronal scoliotic curve into a well-balanced normal lumbar contour.6,7 Moe was the first to report on the Zielke system for thoracolumbar and lumbar scoliosis in the United States.7 He, too, achieved three-plane correction superior to standard posterior spinal instrumentation techniques while fusing fewer vertebral levels.7 Other authors have reported similar results, with curve correction of 59 to 83% and fusion rates of 70 to 100% (Table 18–1). The improved coronal and sagittal correction, as well as the enhanced construct rigidity, significantly improves mechanical loading across the anterior vertebral column and theoretically leads to a higher fusion rate.8,9 In 1985, the Texas Scottish Rite Hospital (TSRH) anterior instrumentation system was introduced (Medtronic Sofamor Danek, Memphis, TN, USA). This system introduced a larger rod (6.35 mm), which predominantly increased construct stability in rotation and flexion-extension.9–11 However, the rigid rod proved to be more difficult to contour, especially in situ.9 Nonetheless, Hall introduced short-segment anterior fusion using this system.12 He advocated overcorrection at the apex of the curve, fusing an average of only 3.4 levels, and reported coronal and sagittal plane correction similar to those achieved using longer constructs. Bitan et al. achieved similar results with the short-segment technique but without over-correcting the instrumented segment.13 The next major advance was the introduction of the dual-rod Kaneda anterior scoliosis system (KASS)14 (Depuy Acromed, Rayhnam, MA, USA). He modified his fracture/tumor system to improve upon the perceived weaknesses of the Zielke system in scoliosis surgery, specifically: (1) weak implants, (2) suboptimal sagittal plane correction, and (3) unacceptable correction losses at long-term follow-up.14 This system includes two flexible (4-mm) rods for improved stability while maintaining implant flexibility. Halm and Liljenqvist similarly modified the Zielke system by adding a second (rigid) rod. They have also reported 2-year results comparable with KASS15,16 (Fig. 18–1). Multiple other dual-rod anterior systems are now available, each offering improved construct stability, elimination of postoperative bracing, and decreased pseudarthrosis rates. A thorough history and physical examination remains the hallmark of any scoliosis evaluation. This includes evaluation of trunk asymmetry and rotation, shoulder balance, and curve flexibility. In addition, most patients will decompen-sate or shift toward the curve convexity. Clinical correlation with the radiographs is also important, especially when correcting trunk shift and shoulder balance. The menarchal status, peak height velocity, Risser sign, and triradiate cartilage status are all markers of skeletal maturity and should also be noted from the history and radiographic evaluation.17–20 Of these markers, an open triradiate cartilage is most predictive of continued curve progression, crankshafting, and decompensation after spinal arthrodesis.19,20 Standard posterior-anterior (PA) or anterior-posterior (AP) and lateral standing and supine side-bending radiographs are required for preoperative planning. It is generally recommended that the lowest instrumented vertebra (LIV) should correct to within 5 to 10 degrees of horizontal on reverse side-bending to prevent decompensation and excessive disk wedging.21–24 Correction of the planned lowest instrumented vertebra to <5 degrees on reverse side-bending is correlated with improved curve correction, better horizontalization of the end vertebra, and better correction of the lumbosacral fractional curve.24 This is especially true for thoracolumbar and lumbar scoliosis. The push-prone and traction films can provide important information regarding the flexibility of both the major and minor curves.25,26 The push-prone view has been shown to predict the postoperative alignment and position of the lowest instrumented vertebra better than supine side-bending views.24 Additionally, these films can help predict the response of the compensatory curves to selective fusion of the primary curve.24,25 Information obtained from the push-prone radiograph was equivalent to or better than two side-bending radiographs at predicting the final postoperative coronal alignment. However, both techniques underestimate the ultimate correction obtained with segmental ASF with instrumentation for thoracolumbar/lumbar curves by 7 to 13%.24,25 Alternatively, axial traction views provide a better prediction of curve correction for large curves (>50 to 60 degrees), and a similar preoperative “stretch film” is required for the Gaines vertebral bone-on-bone fusion technique.25,26 Attention to the vertebral rotation and apparent thoracolumbar kyphosis on the standing lateral radiograph is also paramount in preoperative thoracolumbar and lumbar curve assessment. Figure 18–1 (A to D) Preoperative and postoperative radiographs of a 14-year-old who underwent anterior spinal fusion using the Halm-Zielke anterior spinal instrumentation system (DePuy Spine SARL, Neuchatel, Switzerland). As for vertebral rotation, the Nash-Moe and Perdriolle methods are most commonly used.27 However, the method of Aaro and Dahlborn, which measures the axis of apical vertebral body rotation compared with a sagittal reference line on computed tomography (CT) scanning, yields the best assessment of vertebral rotation.28,29 This technique is not ideal, however, as it is performed in the supine position, not the standing position. We do not promote the routine use of CT for the evaluation and treatment of scoliosis with ASF, as CT scans are impractical and expensive. Furthermore, they result in excessive radiation exposure.30,31 In general, thoracolumbar and lumbar curves 40 to 45 degrees in skeletally immature patients are indicated for arthrodesis to prevent further curve progression. However, there are no absolute indications for selecting an anterior or posterior approach in these curve types. During the past 30 years, ASF has become a favored treatment for idiopathic thoracolumbar and lumbar curves because it offers excellent coronal and rotational correction while fusing fewer levels.32–35 This approach also preserves the integrity of the posterior spinal musculature. Further, posterior fusions ending at L3 or above have been shown to have a decreased incidence of low back pain later in life, hence ASF has been an appealing approach if extension to L4 or L5 would be necessary with a posterior fusion.21,36,37 Whereas an anterior or posterior approach can be used to treat most cases of idiopathic thoracolumbar/lumbar scoliosis, some cases preferentially respond to PSF. Patients with asymptomatic spondylolisthesis may benefit from the distal fusion level (s) saved with an anterior approach,33,34 whereas patients with symptomatic spondylolisthesis may best be approached posteriorly as this permits later extension to the sacrum.12,38 Similarly, King I or Lenke 5C (and most 6C) curves in which the thoracic minor curve demonstrates poor flexibility (<50%) or moderate to large magnitude (>35 to 50 degrees) may best be approached posteriorly as these curves may need to be included in the fusion.12,39 Likewise, rigid fractional lumbosacral curves (“oblique spinal take-off”) inferior to the planned fusion level are best treated via a posterior approach, allowing extension of the fusion to L4 or caudally as needed. Lumbosacral fractional curves that do not correct to <15 degrees from the horizontal on supine side-bending films have an increased risk of postoperative coronal imbalance. Finally, anterior instrumentation should not be routinely placed at L4 level or below, as the hardware poses a risk to the nearby iliac vessels and increases the incidence of injury to the superior hypogastric plexus. Patients with very large (>70 to 90 degrees) or rigid curves, or obese patients (>15% over ideal body weight) may require a combined anterior and posterior spinal fusion, where the anterior approach (release) provides increased curve flexibility while the posterior approach provides supplemental internal stability.40,41 However, advancements in spinal instrumentation techniques have decreased the need for such combined anterior and posterior fusions. The proper selection of fusion levels is simply a balance of the competing goals of improved curve correction versus preservation of spinal mobility, with the ultimate goal of achieving a balanced spine centered over the sacrum in both the coronal and sagittal plane while fusing as few motion segments as possible. Much research has been dedicated toward this end; however, rigid guidelines are not possible. For anterior thoracolumbar or lumbar spinal fusion, the most common recommendation is to include the superior and inferior end vertebrae in the fusion (Fig. 18–2). Puno et al. found that anterior fusions that were stopped short of the inferior end vertebra resulted in increased overall curve progression compared with fusions stopped at the inferior end vertebra.42 Similarly, Luk et al. noted an “adding on” phenomenon with Dwyer and Zielke instrumentation when thoracolumbar or lumbar curves were fused to one level short of the inferior end vertebra.43 Kaneda et al. and Puno et al. both demonstrated better correction of the lower compensatory lumbosacral curve when the primary curve was fused from end vertebra to end vertebra using the Zielke system.42,44 In addition, when instrumentation is extended cephalad to the superior end vertebra, there was an increased likelihood of worsening of the compensatory thoracic curve (29% versus 7% of those fused from end vertebra to end vertebra).42,44 Kaneda et al. reported saving a distal motion segment in 64% of patients in which the vertebra above the inferior end vertebra was neutral, within the Harrington stable zone and horizontalized on side bending.44 For the superior end vertebra, they included this level in the fusion if the compensatory thoracic curve demonstrated >50 to 60% flexibility on supine side-bending. If the compensatory thoracic curve was rigid, then they fused to one vertebral body caudad to the superior end vertebra to prevent decompensation of the thoracic curve. Using these criteria, mean trunk shift improved 84%. When the compensatory curve is large (>35 to 50 degrees) or rigid (<50% flexibility), decompensation can occur after selective fusion, thus necessitating a subsequent PSF.39 For these more problematic curves, primary long posterior or anterior/posterior fusion is preferential. Figure 18–2 Anterior/posterior (AP) radiograph of a 46-degree Lenke 5C thoracolumbar-lumbar curve with mild coronal decompensation to the left. For this case, proper fusion levels should most likely be from T10 to L3 (end vertebra to end vertebra).
Anterior Surgery for Adolescent Thoracolumbar and Lumbar Scoliosis
♦ History of Instrumented Anterior Spinal Fusion
♦ Clinical and Radiographic Evaluation in Adolescent Idiopathic Scoliosis
♦ Indications for Anterior Spinal Fusion
♦ Selecting Fusion Levels
Class | Prevalence Rate (%) |
|
1 | 51 | Main thoracic (MT) |
2 | 20 | “Double thoracic,” MT + proximal thoracic (PT) |
3 | 11 | “Double major,” MT ≥ thoracolumbar/lumbar (TL/L) |
4 | 3 | “Triple major,” PT + MT + TL/L |
5 | 12 | “Thoracolumbar/lumbar,” TL/L |
6 | 3 | Thoracolumbar/lumbar–main thoracic,” TL/L > MT |
Sources: Adapted from Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 2001;83-A (8):1169–1181. Prevalence rates from Lenke LG, Betz RR, Clements D, et al. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: does classification correlate with treatment? Spine 2002;27(6):604–611.
We currently advocate ASF from superior to inferior end vertebra (Cobb angle) for Lenke 5C curves (Table 18–2) and some Lenke 6C thoracolumbar/lumbar curves that meet the listed criteria (Table 18–3). However, if the vertebra above the inferior end vertebra horizontalizes (tilt angle 10 degrees) completely on reverse (concave) side-bending films without causing more than 15 degrees of wedging in the subjacent disk, this distal motion segment may be spared. Likewise, if the lower end vertebra does not horizontalize sufficiently, then we caution ending the fusion at this level.45
Selective Thoracolumbar/Lumbar Curve (Lenke 5C, 6C) Criteria |
Cobb, AVT, AVR ratio of TL/L:MT > 1.25 Flexible thoracic compensatory curve (bends to ≤20 to 25 degrees) No TL/L junctional kyphosis (T10-L2 < + 20 degrees) TL/L > MT trunk shift – decompensation to the side of the TL/L curve Thoracic rib prominence is acceptable to patient, family, and surgeon Closed triradiate cartilage Normal or hypokyphosis (T2-T12 < 40 degrees) LIV corrects to 10 degrees from horizontal |
AVT, apical vertebral translation from the center sacral line; AVR, apical vertebral rotation (Nash-Moe grade); TL/L, thoracolumbar/lumbar curve; MT, main thoracic curve; LIV, lowest instrumented vertebra.
Sources: Adapted from Lenke LG, Edwards CC 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine 2003;28(20):S199–207; Sanders AE, Baumann R, Brown H, Johnston CE 2nd, Lenke LG, Sink E. Selective anterior fusion of thoracolumbar/lumbar curves in adolescents: when can the associated thoracic curve be left unfused? Spine 2003;28(7):706–713; discussion 714; Lowe TG, Betz R, Lenke L, et al. Anterior single-rod instrumentation of the thoracic and lumbar spine: saving levels. Spine 2003;28(20):S208–216.
♦ Surgical Treatment
The anterior thoracolumbar retroperitoneal approach provides excellent exposure for disk removal, interbody grafting and/or placing of structural grafts, instrumentation, and deformity correction across the thoracolumbar junction. It has been the standard anterior surgical approach for deformity correction since it was introduced by Hodgson.46,47 The following sequence of steps is our adaptation of this standard approach for adolescent thoracolumbar or lumbar curves. We currently recommend a dual solid-rod system to provide increased construct rigidity and a decreased pseudarthrosis rate.
Preoperative Preparation
Somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) are used for all deformity correction surgeries to provide early warning of neurological compromise. For anterior spinal surgery, segmental vertebral artery ligation may result in a critical decrement in the blood supply to the corresponding spinal cord level, as approximately two-thirds of the blood supply to the spinal cord comes from the anterior spinal artery, which is supplied by these segmental arteries.48 The largest and most important segmental artery is the arteria radicularis magna, or the artery of Adamkiewicz, which is most commonly found to the left of midline between T8 and L2 in 80% of individuals.49 Preoperative spinal angiography, magnetic resonance angiography, and intravascular contrast-enhanced CT have been used to identify and avoid the artery of Adamkiewicz in an effort to protect the anterior circulation to the spinal cord.49 Alternatively, segmental arteries can be clipped or occluded prior to ligation to evaluate the effect on SSEP and MEP signals. This technique may be more efficacious in congenital scoliosis where the spinal cord may be at an increased risk of ischemia.48 We do not image for the artery of Adamkiewicz preoperatively and consider segmental artery ligation to be extremely safe. Additionally, the Stagnara wake-up test is used as an adjunct to neuromonitoring.50 It is considered the “gold standard” for assessing intraoperative spinal cord integrity.48,50 However, we do routinely practice the Stagnara wake-up test with all patients at a preoperative clinic visit to familiarize the patients with this exam, should it be necessary at the time of operation.
A peripheral arterial line and a central venous line are routinely placed prior to positioning. These permit continuous blood pressure and fluid monitoring by the anesthesia team. A Foley catheter is also placed. If fusion above T10 is planned, a double lumen endotracheal tube may be required, but for routine anterior thoracolumbar or lumbar curves, this is usually not necessary. In most cases, curves up to and including T12 can be treated without taking down the diaphragm.
Surgical Approach
The thoracoabdominal approach is less bloody than the posterior approach.51,52 It traverses well-defined, avascular anatomic planes and does not result in paraspinal muscle denervation as compared with the posterior midline approach.51,53 The approach is almost always on the curve convexity, which is typically the left side, because all anterior instrumentation systems place screws on the convex, lateral side of the instrumented vertebrae. Additionally, the descending aorta is on the left side. The vessel wall is thicker and more durable than the inferior vena cava, which is more easily injured.
The patient is placed on an inflatable beanbag in the lateral decubitus position on a Jackson table (OSI, Union City, CA, USA). An axillary roll is placed approximately one fist-width inferior to the axilla on the dependent side to take pressure off the brachial plexus. The nondependent arm (left arm for a left thoracoabdominal approach) is placed across the body onto a well-arm holder. The hips and knees are flexed to relax the psoas muscle, and the peroneal nerve is padded for protection. A pillow is placed between the knees. The shoulders and hips are then taped in place to immobilize the patient.
The skin incision is made directly over and follows the contour of the rib selected for resection, usually T1052 (Fig. 18–3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree