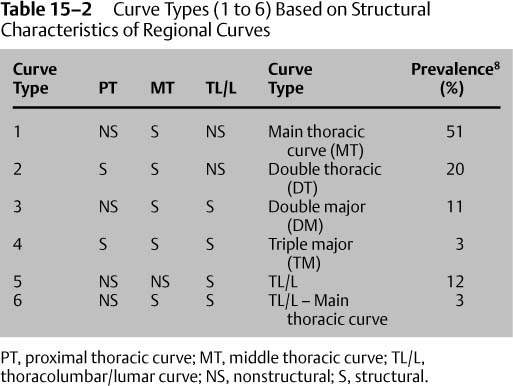
Chapter 15 Anterior surgery has been used for correction of spinal deformity since 1960. Anterior surgery can used for diskectomy, specifically for a release, to improve curve correction after posterior instrumentation; for improving the fusion rate, especially in adults; or for prevention of crankshaft in young adolescents by eliminating the anterior growth plates. In addition, anterior surgery can be the primary means of correction of thoracic scoliosis. The use of anterior instrumentation for correction of thoracic curvatures in idiopathic scoliosis was reported by Dwyer and Schafer in 19741 using theories developed by Dr. Klaus Zielke for lumbar and thoracolumbar curves.2–6 However, anterior instrumentation for correction of thoracic curves did not come into general use until the late 1980s, when Dr. Jürgen Harms began elaborating and refining the technique. In an effort to determine who would be best suited for anterior surgery, the new classification by Lenke et al.7 is best in determining the extent of spinal arthrodesis. The major components of the classification system are as follows: The major curve is always the largest curve and is considered structural. The additional curves are considered minor and can be either structural or nonstructural. The structural characteristics are described in Table 15–1. The residual coronal Cobb angle on side-bending films is 25 degrees for residual structural curves. This is independent of the mechanism of side-bending films, whether supine, erect, or fulcrum. Based on whether the proximal thoracic curve, middle thoracic curve, or the thoracolumbar/lumbar curve is structural or nonstructural, there are basically six curve types: main thoracic, double thoracic, double major, triple major, primary thoracolumbar/lumbar, and thoracolumbar/lumbar with a structural main thoracic curve. The description of these curve types, including whether the curves are structural or non-structural and their prevalence in a series reported by Lenke et al.,8 is shown in Table 15–2.
Anterior Surgery for Thoracic Scoliosis
♦ Classification of Thoracic Scoliosis
Regional Curve | Side-Bend Coronal Cobb Angle | Sagittal Plane Angle |
Proximal thoracic (PT) curve | ≥ 25 degrees | ≥ + 20 degrees (T2-T5) |
Main thoracic (MT) curve | ≥ 25 degrees |
|
Thoracolumbar/lumbar (TL/L) | ≥25 degrees | ≥ +20 degrees (T12-L2) |
Indications for Anterior Surgical Approach for Thoracic Scoliosis
It is generally believed that anterior spinal surgery with instrumentation for the thoracic curve is an option for patients with curve Type 1. The classification system of Lenke et al. further subdivides these curve types into lumbar modifiers A, B, and C. Type C modifier curves behave as false double-major curves, with the lumbar curve crossing the midline. Generally, any of these Type 1 curves with a modifier A, B, or C are candidates for anterior instrumentation. The type C modifier curves are particularly amenable to treatment with anterior instrumentation for preventing lumbar curve decompensation as is seen in 42% of cases after posterior instrumentation.9
Anterior surgery may still play a role in thoracic curve Types 2, 3, and 4 (double thoracic, double major, triple major) where the curves are exceedingly large (greater than 70 degrees) in performing an anterior spinal release for better coronal correction or, on occasion, correction of the thoracic hypokyphosis or thoracic lordosis.
The Lenke et al. classification system further subdivides curves according to the thoracic profile as measured from T5 to T12. Those with sagittal profiles less than 10 degrees are considered hypokyphotic, and in those situations, an anterior release may be considered such that correction of the thoracic kyphosis may be performed consistently. Posterior instrumentation does not consistently correct hypokyphosis with hooks and wires10 nor even with pedicle screws (personal observation). In the authors’ experience, failure to correct the thoracic hypokyphosis significantly leaves the patient vulnerable to development of a proximal thoracic kyphosis.11
Indications for Anterior Instrumentation for Thoracic Adolescent Idiopathic Scoliosis
Despite reports of highly satisfactory results of posterior spinal fusion with multisegmented hook-rod-screw fixation, problems have been reported,9,12–14 including the lumbar curve ending up worse than it was preoperatively, causing unbalancing of the spine9,12,13,15; failure to consistently correct hypokyphosis of the thoracic spine12,14; and the presence of a thoracolumbar kyphosis postoperatively below the level of instrumentation.13,15A The crankshaft phenomenon has been reported after a posterior spinal fusion (PSF) in skeletally immature patients.16 Lumbar pain below the level of posterior instrumented fusion has been reported by Ginsburg and colleagues16A and Cochran and colleagues.17
The published indications for anterior instrumentation for correction of thoracic scoliosis include the potential to save two or more distal fusion levels (Figs. 15–1A to 15–1L) and/or the ability to correct hypokyphosis (less than 20 degrees of kyphosis). In addition, in skeletally immature patients, an anterior release and fusion may be indicated to prevent the crankshaft phenomenon.10 In this situation, insertion of anterior instrumentation potentially involves less surgery than an anterior spinal arthrodesis followed by a posterior arthrodesis with instrumentation.10
The potential number of fusion levels to be saved can be analyzed as follows: The lower instrumented vertebra (LIV) instrumented with anterior thoracic instrumentation is the end vertebral body of the Cobb measurement or, if there are two parallel vertebrae, the more distal vertebra is used. This then can be compared against the predicted posterior LIV either by the stable vertebrae, the Cotrel-Dubousset method,18,19 or Suk’s method.20 In the Cotrel-Dubousset method, the disk below the proposed LIV on a bending radiograph must reverse 5 degrees and the LIV must have less than 20% rotation in the mature patient or have no residual rotation in the immature patient. Dr. Suk’s method uses the neutral vertebra (NV). If the neutral vertebra is the same as the end vertebra (EV) or one level distal, then it is fused to the NV. If the NV is two levels or more distal to the EV, then it is fused to one level proximal to the NV (NV-1).20
Residual hypokyphosis has been reported to occur in up to 60% of cases after posterior multisegmented hook-rod systems,10,12,13 and anterior instrumentation can consistently correct thoracic hypokyphosis and thoracic lordosis.10
Contraindications for Anterior Approach for Thoracic Scoliosis
A double thoracic curve (Lenke et al. Type 2) is one in which the proximal thoracic curve does not bend below 25 degrees. Beware of a proximal kyphosis (T1 to T5) being greater than or equal to 20 degrees and a Lenke Type 2 also.
Patients with preoperative kyphosis (measured from T5 to T12) greater than 40 degrees should have posterior instrumentation. Anterior instrumentation (single rod) cannot correct nor maintain kyphosis.20A
♦ Surgical Treatment
Open Technique
Indications for the Open Technique
Currently, the author only uses an open approach when it is not possible to do the surgery thoracoscopically. Most commonly, this is due to inability to use one-lung ventilation.
Technique
Most commonly, we use a double thoracotomy with a single skin incision.
Results of the Open Technique
The authors, along with other members of the Harms Study Group, conducted a prospective study10 of two cohort groups of patients (one group receiving anterior instrumentation and the other posterior instrumentation) receiving treatment for thoracic idiopathic scoliosis. The objective was to present the 2-year postoperative results of a prospective multicenter study comparing the use of anterior instrumentation with that of posterior multisegmented hook instrumentation for the correction of adolescent thoracic idiopathic scoliosis.
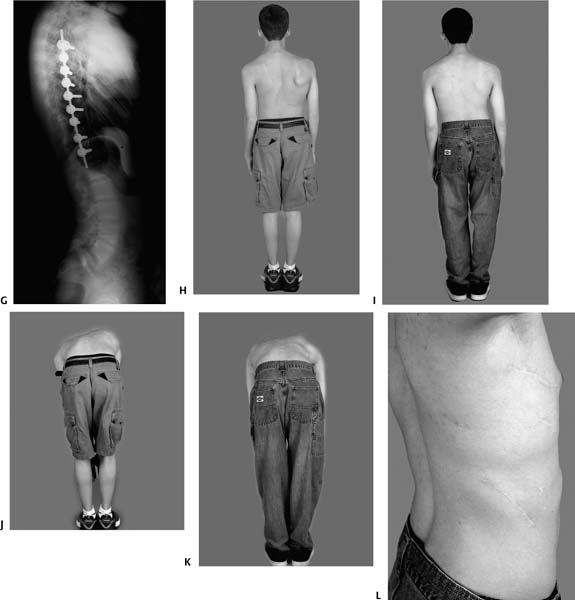
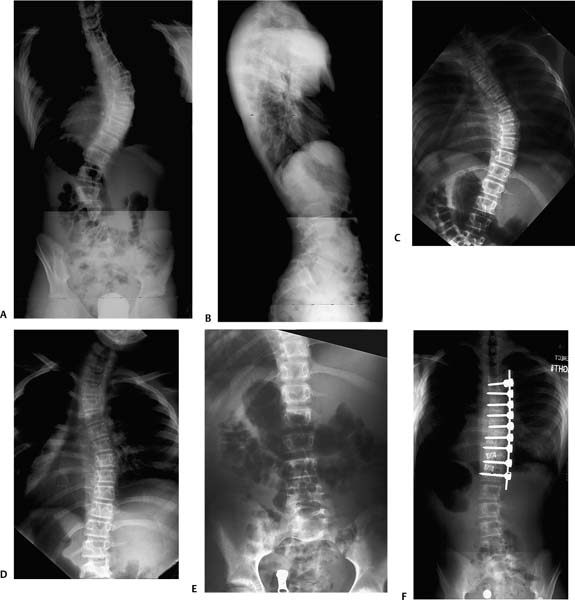
Figure 15–1 Posterior/anterior (PA) (A) and lateral (B) erect of the thoracolumbar spine on a 14″ × 36″ film showing a Type 1CN Lenke curve in this 14-year-old male. The left upper thoracic curve bends down below 25 degrees (C). The main right thoracic curve bends down to 30 degrees (D). The left lumbar bend shows the lumbar curve to be extremely flexible; it bends down to almost 0 degrees (E). This erect postoperative PA (F) and lateral (G) was taken after minimally invasive thoracic anterior instrumentation. Clinical pre (H)– and postoperative (I) photographs. Bending Adams test preoperative (J) versus postoperative (K) showing dramatic improvement in the preoperative thoracic rib prominence just after anterior instrumentation. No thoracoplasty was performed. (L) Close-up of the skin incisions showing the minimally invasive approach with extension of the distal thoracotomy portal into a mini-thoracotomy.
The physician’s traditional criterion for evaluating the outcome of scoliosis surgery has been postoperative radiographic improvement, but there are currently no comprehensive, objective radiographic analyses in the literature. This multicenter study (five institutions) included patients with thoracic idiopathic scoliosis treated surgically with a minimum 2-year follow-up. Ninety-eight patients had anterior instrumentation (anterior group) and 122 had posterior instrumentation (posterior group). The average age at surgery was 14.3 and 14.4 years, respectively, and the preoperative curves averaged 53 and 56 degrees, respectively. The 100-point radiographic scoring system includes both coronal and sagittal measurements. The preoperative radiographic score in the anterior group was 59 ± 8.9 and 57 ± 8.9 degrees in the posterior group, improving to 86 ± 10.3 in the anterior group and 83 ± 7.0 degrees in the posterior group at 2 years. Most of the improvements occurred in the coronal score (38 preoperatively to 64 at 2 years in the anterior group versus 36 to 62 in the posterior group). The sagittal scores changed little in either group. Regarding lumbar spine position in relation to the center sacral vertical line, there was no change in 62% of the anterior versus 66% of the posterior group, improved position in 33% versus 28%, and worsening in 5% versus 6%. In 73 of 98 patients (74%), the fusion stopped at or above L1 in the anterior group versus only 45 of 122 patients (37%) in the posterior group. In conclusion, equal improvement was seen postsurgery in both groups. However, patients with anterior instrumentation were consistently fused shorter than those in the posterior group.
The most significant advantage of anterior instrumentation for thoracic idiopathic scoliosis appears to be the number of distal fusion levels saved (mean 2.5 levels).10 This is in agreement with a study by Hammerberg and Zielke20B, who reported saving an average 2.3 segments distally in a review of 32 patients who underwent ventral derotation scoliosis (VDS) for correction of idiopathic scoliosis.
The saving of any lumbar fusion levels, not just the lower lumbar, appears to be significant regarding prevention of future back pain. Ginsburg et al.16A conducted a review of 113 patients operated between 1946 and 1972 (average 28-year follow-up) and concluded that scoliosis fusions should include as few lumbar segments as possible.
Perioperative Complications
Most research on complications after spine surgery are clouded by the grouping of multiple diagnoses, with few concentrating solely on idiopathic scoliosis. We analyzed the perioperative complications of 673 patients with thoracic adolescent idiopathic scoliosis (AIS) treated with either anterior spinal fusion (ASF) or PSF from the DePuy Spine Harms Study Group Database. “Perioperative” complications (within 3 months of surgery) were defined as “major” (those that caused permanent sequelae, necessitated a second major operation, or required a prolonged hospital stay [≥3 weeks]) or “minor” (those that necessitated a minor operation, caused significant temporary hardship, caused persistent minor problems, or prolonged the hospital stay [<3 weeks]). Because databases tend to under-report minor complications, the charts of those patients from the Philadelphia center were specifically reviewed. Of these 159 patients, 83 patients had ASF and 76 had PSF. The ASF included only open thoracotomies, and none in the PSF group had anterior release, but all had thoracoplasties. The average preoperative curve was 51 degrees in the ASF group and 54 degrees in the PSF group. Average age at surgery was 14 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree