Chapter 45 Application of Current Radiation Delivery Systems and Radiobiology
• Radiosurgery involves the delivery of a high dose of ionizing radiation to a target in a single or a few fractions.
• Physical properties of high-energy photons or protons used for radiosurgery determine their biological effects.
• The biological consequences of high-dose radiation used for radiosurgery are poorly understood, and may differ from those of conventionally fractionated radiation therapy.
• A number of delivery systems are available for modern radiosurgery, with either photons or protons, each of which has unique characteristics for the patient and the physician.
• In retrospective and prospective studies, there are no data that demonstrate a consistent clinical advantage for one type of radiosurgery device over another.
Radiation therapy has been used for the treatment of benign and malignant central nervous system (CNS) diseases for over 50 years. Ionizing radiation, either from machines known as linear accelerators (linacs) or from radioactive sources such as cobalt-60, can be used for either conventional fractionated radiotherapy or single-dose, stereotactic radiosurgery (SRS). Radiosurgery, as defined by both the American Society for Radiation Oncology (ASTRO) and the American Association of Neurologic Surgeons (AANS) is “a distinct discipline that utilizes externally generated ionizing radiation in certain cases to inactivate or eradicate a defined target(s) in the head or spine without the need to make an incision.”1 The definition specifies that radiosurgery is usually delivered in one to five sessions, and uses a stereotactic image guidance system. This definition is in contrast to fractionated stereotactic radiotherapy (fSRT), which uses stereotactic localization and immobilization, but delivers a series of fractions of lower daily dose. This chapter explains the basic physics and biology of radiation therapy, and describes the most common delivery systems used for radiosurgery.
Physics of Radiotherapy
Photon Radiation
The most common form of ionizing radiation used in radiotherapy is the photon, which is a particle that has no mass, travels at the speed of light, and carries the energy present in microwaves, visible light, ultraviolet light, and x-rays. The nature of the interaction of a photon with matter depends upon the energy of the photon. In the kiloelectron volt (keV) range, which is used in most diagnostic x-ray units, photons interact with matter via the photoelectric effect.2 A photon interacts with a tightly bound electron, which absorbs most of the energy and is ejected from the atom and is then free to interact with other atoms in the vicinity. This interaction is highly dependent on the atomic number of the material being irradiated. Diagnostic x-ray studies take advantage of this phenomenon, as bone, which is high in calcium, is much more likely to interact with these photons than soft tissue, which is mostly carbon, hydrogen, and oxygen. This differential interaction is the basis of diagnostic x-ray imaging.
At higher energies, which is the energy of most therapeutic radiation, the Compton effect predominates.2 A high-energy photon in the megaelectron volt (MeV) range interacts with a loosely held orbital electron, which results in ejection of the electron, and scattering of the photon (with a change in energy of the scattered photon). This interaction is independent of the atomic number of the material being irradiated, but it is dependent on electron density. Thus, images generated from therapeutic energy x-rays are less useful for imaging than diagnostic x-rays, as there is little contrast between bone and soft tissue. However, this energy range is useful in radiation therapy, as it is highly penetrating, and is able to interact equally with all tissues.
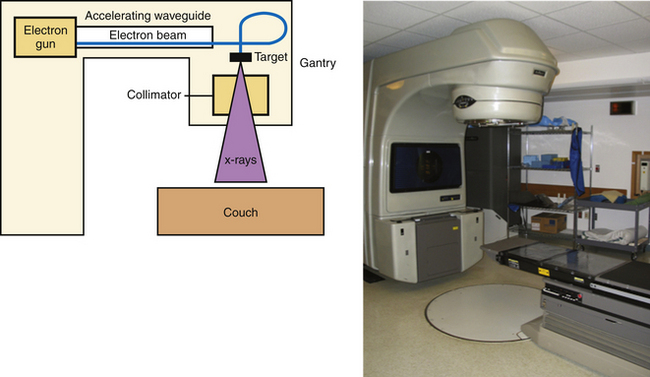
The other main source of high-energy photons is a linac, which uses microwaves to accelerate electrons to a high energy. These electrons are directed to collide with a high-molecular-weight target, and the resulting interactions between nuclei and electrons result in the production of high-energy photons (X-rays) via a process known as bremsstrahlung, or “braking” radiation. The difference between X-rays and γ-rays is simply the site of origin: X-rays are produced by electron interactions but γ-rays are produced by nuclear decay. Unlike the γ-rays produced by 60Co, the energy of the X-rays generated in a linac is based on the characteristics of the machine, and most commercial units offer multiple energy options. These X-rays are produced in the head of the unit (known as the gantry), and can be shaped by a system of controllable leaves, known as a multileaf collimator (MLC), placed between the source of the X-rays and the patient (Fig. 45.1).
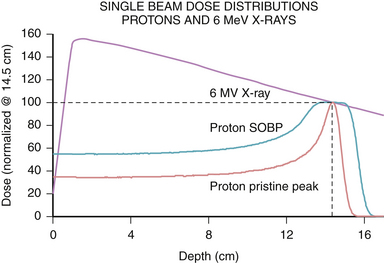
The physical characteristics of photons determine their biological effects. Photons deposit dose in a characteristic pattern, in which there is an initial buildup of energy after entry into the patient, followed by a steady loss of energy as they pass through the tissue according to the law of exponential decay. The energy of the photon is lost in inverse proportion to the square of the distance traveled. Thus, photons spare the skin to some degree, but deposit the majority of their dose upon entrance into tissue, and continue to deposit decreasing amounts of energy as they exit the body (Fig. 45.2). The shape of this depth-dose curve is dependent on the energy of the photon involved. Higher energy photons exhibit greater skin-sparing effect, but have a slower rate of attenuation as they pass through tissue. In general, photons in the 1- to 6-MeV range are used for SRS, as the desired target depth in the cranium is relatively shallow, and higher energies result in unnecessary increased dose delivered beyond the target point.
Proton Radiation
Another form of ionizing radiation used in SRS involves charged particles, most commonly protons. Proton production starts by stripping the electron from molecular hydrogen gas, and the resulting protons are then accelerated to a therapeutic energy level using alternating magnetic fields in a cyclotron or synchrotron. The physical properties of protons result in a different dose distribution from that of photon radiation. Protons have a defined distance of travel, known as the range, which is dependent on their energy. Protons release their energy primarily at the end of their range, which is known as the Bragg peak, after William Henry Bragg, the Nobel Prize–winning physicist. The consequence of the Bragg peak is that protons deposit relatively lower doses of radiation prior to the end of their range compared to photons, and have no exit dose, that is, no dose delivered past their range (see Fig. 45.2). By modulating the energy of protons, a spread-out Bragg peak (SOBP) can be generated to cover wider areas, with the tradeoff of increased entrance dose. Because of their sharp range and lack of exit dose, protons provide a favorable dose profile for use in SRS. The disadvantage of protons is that their availability is limited to a few centers due to the cost and complexity of maintaining such facilities for clinical use.
Biology of Radiation Therapy
The primary target of ionizing radiation is generally thought to be damage to the DNA of target cells. As described previously, ionizing radiation results in the ejection of electrons from the atoms in the tissue being irradiated. Because most of the cell is water, the photon or proton is most likely to interact with a molecule of water, resulting in the production of superoxide, hydroxyl radicals, and other reactive oxygen species, which damage the DNA and result in replicative failure. Thus, radiotherapy is believed to be more effective in the presence of oxygen,3 and it is thought that hypoxic areas of tumors may be less sensitive to the effects of ionizing radiation.4
Although many different types of DNA damage can be produced by ionizing radiation, the most critical form of damage in the use of therapeutic radiation is the double strand break. Double strand breaks are more difficult for cells to repair, and the repair process can generate aberrant chromosomes that result in mitotic catastrophe, or mutations that result in reduced replicative fitness.5 The critical nature of the double strand break is evidenced by the fact that patients with mutations in the ataxia-telangiectasia mutated (ATM) gene, one of the key sensors of DNA double strand breaks,6 and an integral part of double strand break repair, are extremely sensitive to ionizing radiation damage.7
The production of double strand breaks is related to the efficiency of the particle in transferring its energy to the surrounding matter. This concept is quantified as the linear energy transfer (LET) of differing radiation modalities, and results in differences in the relative biological effectiveness (RBE) of different types of radiation beams. Photons produced by 60Co are considered to have a low LET and are defined to have an RBE of 1. However, the LET varies with both energy and with the type of particle used in irradiation. For example, neutrons, which are large, noncharged particles, have a very high LET, and produce more double strand breaks for a given dose of radiation, resulting in a higher RBE.8 Protons at therapeutic energies, although of similar mass to neutrons, do not exhibit a particularly high LET, presumably because their positive charge leads to repulsive forces with atomic nuclei. Protons used in radiotherapy have been calculated to have an RBE of 1.1 compared to photons produced by 60Co.9 This means that for a given absorbed dose, protons will have a 10% greater biological effect. To avoid confusion, proton therapy doses are typically reported as gray (relative biological effectiveness) (Gy[RBE]), taking this correction factor into account.
Although DNA damage is known to be the primary mechanism of action of radiation, the cellular target of radiotherapy is more controversial. For malignant tumors, which are highly proliferative, and often have impaired DNA repair,10 the target is thought to be the cancer cells themselves, as they are unable to repair the DNA damage inflicted by ionizing radiation. Furthermore, their rapid progression through the cell cycle results in more potential checkpoints that can trigger cell death. Thus, cancer cells are more sensitive than normal cells to radiation. This effect is seen clinically, as radiation of malignant tissues often causes clinical or radiographic regression of the lesion.
In contrast, for benign disease, the cells are not as proliferative, and may be in resistant phases of the cell cycle. These observations have led some to speculate that benign tumors are relatively radioresistant.11 However, in clinical practice, radiation appears to induce a quiescent state, which corresponds to radiographic and clinical stability,12,13 suggesting that benign tumors respond to radiotherapy in some way. It is possible that these tumors undergo DNA damage that limits their replication, but the biology of this process is still unclear.
Although tumor cells have been thought to be the primary target of radiotherapy, many have suggested that radiotherapy has an effect on vascular endothelium, which mediates the primary mode of cell death, especially at the higher doses used in SRS.14,15 Irradiation of B16 melanoma cell explants in mice with doses of 15 to 20 Gy result in waves of endothelial cell apoptosis 1 to 6 hours after irradiation.15 The endothelial response was critical to tumor control, as endothelial- specific mutation of Bax, a critical regulator of apoptosis, rendered these explants insensitive to doses of 15 Gy. Thus, endothelial cell death may lead to direct hypoxic necrosis of the tumor, or may secrete signaling molecules that may cause tumor death. However, other studies have shown that at even higher radiation doses (>20 Gy), the mode of death in an irradiated gastrointestinal tract appears to become independent of endothelial cell apoptosis,16 suggesting that the dose response relationship is complex, and may be differentially regulated in different tissues. These differences are the subject of much investigation and may become more important as combination chemotherapy or targeted therapy is considered.
These observations correlate with data from radiosurgical experiments exposing normal rat brain or tumor explants to radiosurgical doses of ionizing radiation. Examination of human acoustic schwannoma xenografts after irradiation with 10 to 40 Gy showed a significant decrease in tumor vascularity, as well as significant intramural vascular hyalinization.17 Furthermore, irradiation of rat brains with 15 to 30 Gy resulted in changes in local blood flow, leukocyte/endothelial interaction, formation of aneurysmal structures, and thrombus formation.18 These data suggest that vascular damage by radiosurgery may be an important component of its clinical effect.
Fractionation versus Radiosurgery
Conventional radiotherapy is typically fractionated into daily doses, which is thought to result in reduced effects of radiation on normal tissue. Fractionation allows for DNA repair to occur, which is predicted to favor normal cells that retain the full complement of DNA repair proteins.19 Furthermore, fractionation allows for reoxygenation of hypoxic areas, resulting in increased sensitivity of malignant cells that were previously hypoxic.20 Additionally, fractionated therapy allows for reassortment of cells in the cell cycle, as cells are most sensitive to radiation during the G2/M phase of the cell cycle and resistant during the late S phase and G1. Thus, giving radiation in daily fractions allows those cells that are in resistant phases of the cell cycle to move to more sensitive phases of the cell cycle during subsequent fractions.21 The downside of fractionation is that it allows for repopulation of tumor cells during the therapy. Reoxygenation, reassortment, repair, along with repopulation, are known as the “four Rs” of radiobiology, and explain the radiobiological basis for daily fractionated therapy.
The value of fractionation is more apparent for certain tissues, which typically have high rates of proliferation and show relatively less capability to repair sublethal DNA damage. This concept is quantified as the α/β ratio, which is a radiobiological concept, based on a model of radiation response, that attempts to explain the differential sensitivity of tissues to fractionation.22 Tissues with a high α/β ratio respond quickly to radiotherapy, and are sensitive to smaller fraction sizes. Examples of these so-called “early” responding tissues include the gastrointestinal tract, lymphocytes, and skin. Tissues with a low α/β ratio respond more slowly to radiation, are typically less proliferative, and show a high capacity for DNA repair. Examples of late responding tissues include neural tissue and the lung.
The α/β ratio can be used to calculate a biologically equivalent dose (BED), which attempts to equalize total doses that are given in different fraction sizes. The equation is BED = (number of fractions ∗ fractional dose) ∗ (1 + (fractional dose/α/β ratio)).22 Although there is debate over the validity of this model at the high doses used in radiosurgery, it allows one to approximate the effect of doses delivered in fractionated sessions and those given in radiosurgery. For example, if one assumes a tumor to have a high α/β ratio of 10, a dose of 20 Gy in a single fraction is biologically equivalent to a dose of 40 Gy in 8 fractions, or 50 Gy in 25 fractions. However, for normal brain tissue, which has an α/β ratio closer to 3, the schedule 20 Gy × 1 has a BED of 153.3, while 5 Gy × 8 has a BED of 106.7, and 2 Gy × 25 has a BED of 83.3. Thus, the preceding regimens have the same BED for a tissue with a high α/β ratio, but the larger fraction sizes have a much higher BED for tissues with a low α/β ratio. What this means is that although the tumor control would be predicted to be equivalent for 20 Gy in 1 fraction and 50 Gy in 25 fractions, the radiosurgical dose would produce a more profound effect on normal brain tissue. Although the BED is merely an approximation of biological effect and not a real quantity, it can be useful when considering the dose of radiation to be used when the target is close to critical normal structures such as cranial nerves.
Another potential explanation for the excellent clinical effect of radiosurgical doses in malignant disease lies in the possibility that high radiation doses are required to kill radiation-resistant cells. Emerging data suggest that clonogenic cells within tumors may have an intrinsically higher radioresistance due to increased expression of antioxidant genes.23 It may be that very high radiation doses are able to overcome this effect, resulting in death of those clonogenic cells, and leading to tumor control.
The radiobiological concerns outlined here suggest some situations when it may be advantageous to choose fractionated treatment over single-fraction radiosurgery. Given that normal neural tissue, including cranial nerves, are late-responding, with an α/β ratio of approximately 3, they will be more sensitive to large radiation doses compared to small ones. If the target to be treated is in close proximity to one of these structures (e.g., optic nerve sheath meningioma24 or a pituitary tumor very close to the optic chiasm25), it may be more prudent to fractionate treatment to reduce the risk of injury to the cranial nerves. Conversely, for hormone-secreting tumors, there is biological evidence that high-dose radiosurgery is associated with more rapid normalization of hormone levels.26 Thus, the choice between radiosurgery and fractionated treatment must weigh a number of radiobiological and clinical parameters.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree