tips and tricks
“Listen to the patient, son. He’s trying to tell you his diagnosis.”
“Doctors diagnose a patient within the first 18 seconds of speaking with them.”
Jerome Groopman: How Doctors Think.
The first admonition has stayed with me ever since I heard it from a senior physician more than 40 years ago. The second quotation reflects the reality of contemporary medicine. As Groopman points out, physicians make diagnoses based on their experience and the rules of thumb (heuristics) from that experience. Myasthenia gravis (MG), the most common neuromuscular junction (NMJ) disease, is far from common, and the Lambert–Eaton syndrome (LES) is even rarer, thus most physicians have seen too few examples to develop their own sense of how these patients present. The first, and most important, step in diagnosing NMJ disorders is to think of them. However, MG was included in the differential by the first evaluating physician in less than half the patients with MG ultimately referred to the author’s clinic (Table 15.1). The characteristic clinical presentations of MG and LES are described in this chapter. Once these distinctive patterns of weakness are recognized from the history and examination, confirmation by appropriate diagnostic tests is usually straightforward.
Table 15.1. Initial diagnosis in 700 patients with definite acquired myasthenia gravis (MG)
From Sanders DB, Massey JM – unpublished data.
| Initial diagnosis | Number (%) |
| MG | 329 (47) |
| Eye disease | 96 (14) |
| Cerebrovascular accident | 84 (12) |
| Psychological | 20 (3) |
| Myopathy | 15 (2) |
| Bell’s palsy | 13 (2) |
| Thyroid disease | 10 (1.4) |
| Brain lesion | 8 (1.1) |
| Multiple sclerosis | 8 (1.1) |
| Allergy | 8 (1.1) |
| Blepharospasm | 3 (0.4) |
| Other | 106 (15) |
The Clinical Presentation of MG
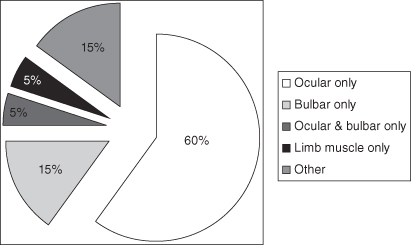
Patients with MG (and LES) seek medical attention because of specific muscle dysfunction. Although they frequently also have excessive fatigue, that is not usually their major complaint. Weakness of ocular or eyelid muscles brings most MG patients to the doctor – in the author’s clinic, 70% of MG patients had eyelid ptosis, diplopia, or blurred vision at onset, and these were the only initial symptoms in 60% (Figure 15.1). Bulbar symptoms – slurred, nasal, or garbled speech, or difficulty chewing or swallowing – are the next most common presenting symptoms. When prompted, patients may recall previous transient episodes of ocular or bulbar muscle weakness – a drooping eyelid or double vision – that resolved spontaneously after several days, frequent changes in spectacles to improve blurred vision, trouble reading or watching TV in the evening, not driving in bright daylight because of double vision, giving up singing because of voice changes, avoiding foods that have become difficult to chew or swallow, coughing after eating because of aspiration, and nasal regurgitation of liquids.
Figure 15.1. Initial symptoms in 919 patients with myasthenia gravis seen at the Duke University myasthenia gravis clinic (Sanders DB and Massey JM, unpublished data). Seventy percent had ocular symptoms (ptosis, diplopia, or blurred vision) at onset, and these were the only initial symptoms in 60%. Twenty-two percent had bulbar symptoms (dysarthria, dysphagia, or facial weakness), and these were the only symptoms in 15%; 5% had ocular and bulbar symptoms, and these were the only initial symptoms in 4%; and 5% had isolated weakness of limb or axial muscles alone. Twelve percent had initial symptoms of generalized weakness or fatigue, with or without other symptoms.
Patients with a recently described subset of MG associated with antibodies to muscle-specific tyrosine kinase (MuSK) frequently have findings atypical for MG. As many do not have ocular muscle weakness and weak muscles may be atrophic, the clinical findings may be more suggestive of motor neuron disease or a myopathy than of MG. Suspect MuSK-MG if there is facial or tongue weakness and atrophy, or weakness that predominates in neck or shoulder muscles.
 caution!
caution!
- Patients with MG associated with MuSK antibodies may have clinical findings suggestive of motor neuron disease or a myopathy, rather than of MG.
- Suspect MuSK-MG if there is facial or tongue weakness and atrophy, or weakness that predominates in neck or shoulder muscles.




