Approach to the Hypokinetic Patient
Robert L. Rodnitzky
Ergun Y. Uc
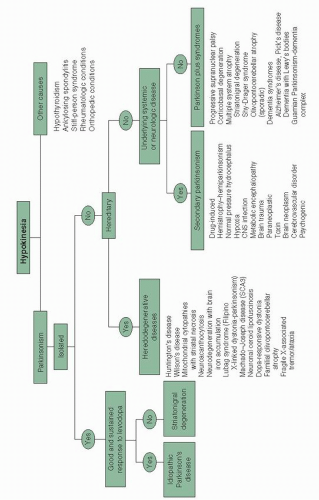
Hypokinesia is defined as a decrease in the amount and amplitude of both volitional and automatic movements and is almost always associated with bradykinesia (slowness of movement). The term akinesia is sometimes used to imply a severe reduction in the amount or amplitude of movement. Parkinsonism refers to a motor syndrome with the following cardinal features: bradykinesia, rigidity, rest tremor, and postural instability. Idiopathic Parkinson’s disease (IPD) is the most common cause of parkinsonism. Other forms of parkinsonism are histologically different and often accompanied by additional neurologic signs and symptoms (Fig. 29.1).
Through careful questioning, clinicians can distinguish a history of neuromuscular weakness from a movement disorder causing parkinsonism such as IPD. It is also essential to determine whether slowness or lack of movement is caused by a psychiatric disorder (catatonia or severe depression), neuromuscular condition producing stiffness (e.g., stiff person syndrome), endocrine disorder such as hypothyroidism with resulting global slowing, or a rheumatologic condition such as ankylosing spondylitis with mechanical restriction of movements.
I. EVALUATION OF PARKINSONISM: HISTORY
A. Direct motoric manifestations of parkinsonism.
What a patient perceives as weakness or poor balance may actually be a manifestation of hypokinesia. Conversely, slowness in performing motor functions such as dressing, walking, feeding, or writing may actually relate to incoordination, weakness, or dementia. Difficulty in rising from a chair, hesitancy in initiating gait, and a change in the legibility and size of handwriting, falls, freezing, hypophonia, and hypomimia are common symptoms of hypokinesia.
Rest tremor, stiffness (rigidity), and postural imbalance in the absence of other neurologic complaints suggest an IPD. On the other hand, the association of hypokinesia/ bradykinesia with neurologic symptoms outside the motor realm usually suggests a condition other than IPD. Such symptoms include seizures, sensory loss, paresthesias, headache, early dementia, visual loss, apraxia, and early or severe autonomic symptoms such as impotence, orthostatic hypotension, or urinary incontinence. Another useful historical fact in differentiating IPD from other forms of parkinsonism is the sequence in which otherwise typical parkinsonian symptoms appear. Although postural imbalance and severe gait disturbance often appear late in the course of IPD, their appearance as presenting symptoms in a hypokinetic patient suggest a different etiology of parkinsonism.
B. Response to medications.
Absence of benefit from adequate dosages of dopaminergic drugs, especially levodopa, casts doubt on the diagnosis of IPD and suggests a diagnosis of secondary causes of parkinsonism or one of the Parkinson’s-plus syndromes. Equally important is determining whether, early in the illness, these medications produced psychiatric side effects such as hallucinations or autonomic symptoms such as severe orthostatic hypotension. The former suggesting the possibility of dementia with Lewy’s bodies (DLB), and the latter indicating possible multiple system atrophy (MSA). In IPD, psychiatric and autonomic side effects from dopaminergic drugs are not uncommon but usually appear when the illness is at least moderately advanced.
C. Cognitive symptoms.
Even early in the course of the disease process, patients with IPD may have mild executive and visuospatial dysfunction. Frank dementia is more common among older patients and usually after the illness is moderately advanced. Mild to moderate cognitive symptoms are present in most of the Parkinson’s-plus
syndromes but are seldom the presenting symptom. Severe, early cognitive abnormalities may indicate a primary dementing disorder such as Alzheimer’s disease (AD) or vascular dementia.
syndromes but are seldom the presenting symptom. Severe, early cognitive abnormalities may indicate a primary dementing disorder such as Alzheimer’s disease (AD) or vascular dementia.
D. Psychiatric symptoms.
Symptoms suggestive of depression or anxiety may precede the onset of IPD. If hallucinosis (typically visual) is present, determine if it began early or late in the course of the illness and whether it appeared in response to the institution or escalation of an antiparkinson drug. Very early appearance of hallucinations in cases of parkinsonism or their presence in an untreated parkinsonian patient raises the probability of DLB.
E. Sleep disorders.
The rapid eye movement behavior may precede the onset of parkinsonism by several years in IPD or DLB. Restless legs syndrome and/or periodic limb movements of sleep may be associated with IPD. Discomfort because of rigidity and inability to turn in bed can cause sleep fragmentation (see Chapters 9 and 55).
F. Dysautonomia.
Constipation, urinary urgency, impotence, and orthostasis may accompany or even precede IPD. When prominent early, these symptoms may suggest MSA.
G. Medication usage.
Patients must be asked if they are currently taking or have recently received antidopaminergic drugs such as neuroleptics, reserpine, or metoclopramide. In addition any history of illicit drug use should be ascertained.
H. Family history.
IPD has a complex and multifactorial etiology. Patients with Mendelian pattern of inheritance constitute a small minority of the overall Parkinson’s disease (PD) population. Heritable disorders that can mimic PD include Wilson’s disease (autosomal recessive), juvenile Huntington’s disease (HD; autosomal dominant), and essential tremor (ET; autosomal dominant with variable penetrance).
I. Toxic exposure.
Exposure to toxins such as manganese or carbon monoxide must be ascertained because both can result in parkinsonism. Less common causes include mercury, carbon disulfide, methanol, and cyanide.
II. PHYSICAL EXAMINATION
A. The clinical findings of parkinsonism.
1. Hypomimia is characterized by diminished facial expression with infrequent eye blinking. A fixed facial expression, often seen in progressive supranuclear palsy (PSP), consists of an unchanging expression such as surprise in which the forehead may be furrowed, the eyelids retracted, and the nasolabial folds deepened. Myerson’s sign, present in IPD and a variety of other basal ganglia disorders, consists of persistent reflex eyelid blinking to repetitive finger taps applied to the glabella, instead of the normal rapid habituation after the fourth or fifth tap.
2. Hypophonia is characterized by diminished amplitude and inflection of speech. Tachyphemia is an excessively rapid speech pattern, which is a common accompaniment of hypophonia, making such speech even more unintelligible.
3. Rigidity may be predominant in axial muscles (e.g., neck or trunk), in the limbs, or equally severe in both. Increased resistance to passive movement of the involved body part is easily appreciated when rigidity is severe. When subtle, rigidity can be reinforced by asking the patient to alternately open and close the fist of the hand on the side opposite of the arm or leg being tested. The presence of tremor in the same limb demonstrating rigidity gives rise to a rachet-like sensation referred to as cogwheel rigidity.
4. Tremor may appear in one or more forms in patients with parkinsonism.
Resting tremor is the hallmark of IPD. Its absence casts some doubt on the diagnosis but certainly does not rule it out. It is also present in some other forms of parkinsonism. The tremor is most commonly seen in the hands and to a slightly lesser extent in the lower extremities and mandible. Rest tremor rarely involves the head and never affects the voice. It appears at a frequency of 4 to 5 Hz and is often at least temporarily extinguished by volitional movement. A subtle tremor can be uncovered by asking the patient to perform difficult mental arithmetic, a mildly stressful task.
Action tremor may also be present in IPD as well as in other parkinsonian syndromes, especially those associated with cerebellar dysfunction. It can be present as a postural tremor while the arms are outstretched in front of the patient or as a kinetic
tremor while the patient is performing a task such as the finger-to-nose test. Postural tremor alone, in the absence of parkinsonian signs, suggests a diagnosis of ET.
Positional tremor. Some tremors are particularly prominent when the involved body part is placed in a specific position. The wing beating tremor of Wilson’s disease is an example of this phenomenon. This tremor is noted when the arms are abducted at the shoulders while flexed at the elbow.
5. Bradykinesia can be documented by simply observing the speed, amplitude, and amount of ordinary movements made by the patient such as gestures or shifting of body position. Repetitive motion tasks such as tapping the index finger against the thumb demonstrate slowness of movement and a progressive loss of amplitude.
6. Impairment of automatic movements is noticeable as a decrease in gesticulation and head movement during conversation, a reduction in the automatic repositioning of limbs while sitting in a chair or reclining in bed, and as a decrease in the amplitude of arm swing while walking. In severe hypokinesia, the affected arm(s) may not swing at all, but rather be held in a semiflexed posture across the trunk.
7. Impairment of repetitive movements such as handwriting or buttoning a shirt is not only performed slowly, but the amplitude of each successive movement typically becomes progressively smaller. This may account for the progressively smaller letters (micrographia) seen when a hypokinetic patient is asked to write a long sentence.
8. Impaired initiation of movement is manifested by difficulty in arising from a chair or hesitancy in taking the first step while attempting to walk. Many patients with IPD have difficulty initiating two motor acts simultaneously such as standing up and shaking hands. Rising from a chair is tested by asking the patient to rise with arms crossed in front of the body to prevent pushing off. The patient may require several attempts to succeed or may be totally unable to arise without using his arms. If the patient is unable to rise without assistance, a judgment must be made as to whether the cause is weakness (which can be tested independently).
9. Gait and posture should be evaluated by having the patient walk a distance of at least 20 feet in an area free from obstacles. Parkinsonian patients often display reduced stride length and arm swing, stooped posture, difficulty in initiating gait, and turns with the body moving as a single unit (en bloc). In more advanced cases, progressively more rapid, small steps as the body leans forward (festination) and “freezing” in mid gait may be observed.
10. Freezing is a sudden involuntary cessation of a motoric act, usually walking, while other functions remain intact. This phenomenon is confined to basal ganglia disorders. It may occur spontaneously or may be provoked by external circumstances such as attempting to turn mid gait or pass through a narrow space such as a doorway. Emotional stimuli including anger or fear can provoke freezing as can the prospect of entering a room filled with people. A variety of sensory or motor tricks such as marching to a cadence are effective in overcoming freezing.
11. Postural reflexes are evaluated by asking the patient to establish a comfortable base, with feet slightly apart and then, while standing behind the patient, applying a brisk backward sternal perturbation. A normal response is to take up to one corrective step backward to prevent falling. When postural reflexes are impaired, more than one step will be needed before balance is reestablished. When postural reflexes are absent, the patient will continue to reel backward and fall if not checked by the examiner.
B. Non-Parkinsonian neurologic signs.
Several neurologic findings are associated with one or more forms of atypical parkinsonism, but most of these signs are uncommon in IPD.
1. Apraxia should be tested independently in both upper extremities. The patient should be asked to perform such tasks as saluting, throwing a kiss, or demonstrating how to use an imaginary tooth brush. Inability to perform these tasks in the face of normal strength and coordination, or the use of a body part such as a finger in place of an imagined implement, suggest apraxia. Apraxia and parkinsonism can be seen in cases of corticobasal degeneration (CBD) and AD.
2. Cortical sensory functions such as graphesthesia, stereognosis, and tactile localization are sometimes abnormal in CBD.
3. The alien limb phenomenon is present when a patient manifests uncontrollable grasping and manipulating of objects or when a hand exhibits interfering involuntary
movement with one of the other limbs (inter manual conflict). This phenomenon may be present in CBD, ischemic strokes, or Creutzfeldt-Jakob’s disease (CJD).
movement with one of the other limbs (inter manual conflict). This phenomenon may be present in CBD, ischemic strokes, or Creutzfeldt-Jakob’s disease (CJD).
4. Ocular motility abnormalities. Inability to generate normal saccadic eye movements, especially downward, with preservation of the same movements when eliciting the oculocephalic reflex indicates a supranuclear gaze palsy. This finding is most characteristic of PSP but can be found in other forms of atypical parkinsonism as well. It is important to remember that limited upgaze is not an uncommon finding in the normal elderly patient, but impaired downgaze is always abnormal. Excessive macro square wave jerks, spontaneous repetitive small horizontal oscillations of the eyes from the midline, are also seen in PSP.
5. Reflex myoclonus, elicited by tapping the arm, leg, or fingertip with the examiner’s own fingertip or with a percussion hammer, may be present in cases of CBD.
6. Blood pressure must be measured in the recumbent and standing positions while recording the concurrent heart rate. Orthostatic hypotension is an early and common manifestation of MSA but occurs later in the course of IPD, especially with the use of dopaminergic or anticholinergic drugs.
7. Mental status evaluation. Evaluation should include functions such as immediate and short-term recall, orientation, constructional praxis, calculation, and comprehension of three-step commands.
8. Other neurologic signs. In order to determine the full extent of involvement of the CNS, a complete neurologic examination should be performed to establish the presence of hyperactive or hypoactive muscle stretch reflexes, sensory loss, cranial nerve dysfunction, cerebellar signs, pathologic reflexes (especially Babinski’s sign), weakness, or muscle atrophy.
III. LABORATORY STUDIES