Approach to the Patient with Gait Disturbances and Recurrent Falls
Rodger J. Elble
Jorge C. Kattah
Locomotor disturbances are common in all age groups but are particularly common among older people. Impaired locomotion is a source of disability for approximately 15% of people older than 65 years, rivaling dementia as the leading form of neurologic impairment. The examination of gait and balance provides the clinician with invaluable insight into a patient’s functional status and is arguably the highest yielding component of the motor exam.
I. PATHOPHYSIOLOGY
A. Locomotion
requires the integrated control of posture and movement. Postural control is necessary for static and dynamic stability during stance and locomotion. Somatic, visual, and vestibular sensory information are used in complex feedback (reflex) pathways that enable the nervous system to respond to altered stability. These sensory inputs are also combined with experience to adjust the pattern of stance or locomotion in anticipation of threatened stability. This anticipatory or feedforward control of movement is critically important because reflex responses are too slow and inaccurate for normal locomotion. Feedforward locomotor control utilizes working memory and other cognitive functions that are impaired in many patients with cerebral disease.
B. Anatomy and physiology.
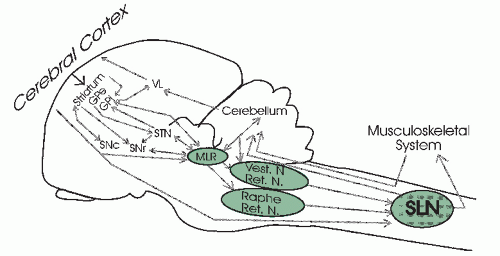
The basic locomotor rhythm emerges from spinal neuronal networks that interact directly with several brainstem nuclei and the cerebellum (Fig. 8.1).
1. Cortical-basal ganglia-thalamocortical circuitsplay an important role in selecting desired postures, movements, and behaviors while suppressing undesired postures, movements, and behaviors. Damage to these circuits impedes adaptation of gait and posture to varying environmental and emotional circumstances.
2.The midbrain locomotor region of the dorsolateral midbrain contains a heterogeneous group of neurons that connect with the basal ganglia and with raphe and reticular nuclei in the caudal pons and rostral medulla. The midbrain locomotor region and its connections play a critical role in the initiation of gait and control of posture.
3.The cerebelluminteracts with pontomedullary reticular nuclei, the red nucleus, and the vestibular nuclei in the coordination of posture and rhythmic limb motion. It receives input from the spinal locomotor network; from peripheral somatosensory, vestibular, and visual pathways; and from cerebral cortex by way of the pontine, olivary, and other brainstem nuclei. These connections enable the cerebellum to play a pivotal role in the feedback and feedforward control of posture and movement.
4. The reticulospinal and vestibulospinal pathways in the ventral spinal cord are necessary for rudimentary control of the spinal networks. The corticospinal pathways are needed for flexible, adaptive control, and this “highest level control” is accomplished through rich cortical connections with the basal ganglia, thalamus, and cerebellum. Thus, the nervous system can modify posture and locomotion as dictated by environmental constraints, body mechanics, and personal desires.
II. ETIOLOGY
A. Gait disturbances.
A disturbance of locomotion can occur at any level of the neuraxis (Fig. 8.1), and neurologic disturbances commonly lead to secondary skeletal deformities and muscle deconditioning that cause additional impairment of locomotion. The causes
of locomotor impairment are myriad. Multiple coexistent etiologic factors are common, particularly in older persons.
of locomotor impairment are myriad. Multiple coexistent etiologic factors are common, particularly in older persons.
1. Gait disturbances are caused by any disease affecting the frontal and parietal lobes, basal ganglia, thalamus, brainstem motor nuclei, cerebellum, spinal cord, peripheral nerves, vision, vestibular function, and the musculoskeletal system.
2. Acute unilateral lesions typically produce focal neurologic signs and postural instability. The postural instability usually resolves or greatly improves with time.
3. Acute or chronic bilateral lesions typically produce a more severe and refractory disturbance of gait and balance.
B. Causes of recurrent falls.
Environmental hazards and errors in judgment are responsible for 35% to 50% of falls in some studies, but most patients with recurrent falls have underlying neurologic disease. Common etiologies of recurrent falls include previous stroke, Parkinson’s disease, severe arthritis, peripheral neuropathy, orthostatic hypotension, dementia (confusion), poor vision, and vestibular disease. Medications are also a common contributing factor or primary cause. Altered sensorium and impaired cognition impede feedforward modifications of posture and movement, resulting in increased risk of falls.
III. CLINICAL MANIFESTATIONS
A. Features of normal walking.
The gait cycle is defined as the time between successive heel-floor contacts with the same foot (Fig. 8.2). One gait cycle consists of two steps (one stride). From right heel-floor contact to left toe-off is a period of double-limb support, which normally lasts approximately 10% of the total gait cycle. This phase of the cycle is followed by the left swing phase, which is simultaneous with and equal to the right single-limb support phase. The time from left heel-floor contact to right toe-off constitutes the second of two double-limb support phases in a gait cycle and is followed by the right swing phase and left single-limb support phase.
1. Stride length (length of two successive steps) and cadence (steps per minute) determine the velocity of walking (stride length × cadence ÷ 2). The magnitudes of arm swing, toe-floor clearance, and hip and knee rotations are proportional to stride
length and velocity, whereas the percentage time in double-limb support increases with reductions in gait velocity. Reduced gait velocity is a nonspecific sign of an underlying medical condition and is associated with reduced long-term survival.
length and velocity, whereas the percentage time in double-limb support increases with reductions in gait velocity. Reduced gait velocity is a nonspecific sign of an underlying medical condition and is associated with reduced long-term survival.
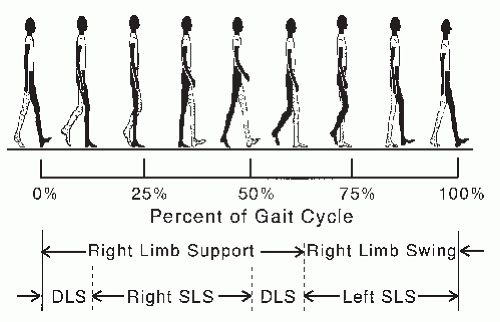 FIGURE 8.2 Phases of the normal gait cycle, expressed as percentage of total stride. DLS, double-limb support; SLS, single-limb support. |
2. The total-body center of mass oscillates vertically at a frequency equal to the cadence and horizontally at one-half the cadence. During a gait cycle, the two maxima in vertical oscillation occur in the middle of right and left single-limb support, and the two minima occur in the middle of the two phases of double-limb support. The left- and right-most horizontal excursions of the center of gravity occur at the times of mid-left and -right single-limb support. These vertical and horizontal excursions of the center of mass are optimized in such a way that the center of mass (body) moves forward with the least amount of expended energy. Consequently, most gait disturbances increase expended energy.
B. Normal development of walking.
Most children walk independently by 15 months, and a fairly mature pattern of lower limb movement is achieved 3 months after walking begins. Maturation of gait and balance probably continues throughout childhood, but most of this maturation is accomplished by 3 or 4 years of age. At this age, most children have lost their lordotic posture and are capable of walking on narrow beams and standing with feet together and eyes closed. Failure to walk by 18 months should be investigated for neuromuscular disease, CNS pathology, visual impairment, and vestibular disease. Independent walking is delayed in blind children, only 50% walking by 24 months.
C. Abnormal patterns of walking.
The characteristics of an abnormal gait are usually a mixture of primary abnormalities (direct effects of the underlying disease), secondary musculoskeletal abnormalities (e.g., joint contractures and musculoskeletal deconditioning), and compensatory changes. All must be considered when deciphering a patient’s gait.
1. Cautious gait is a slow, guarded, or restrained pattern of walking that resembles someone walking on a slippery surface or in a threatening environment. There is slightly stooped posture (lowered center of gravity), reduced arm swing, increased time with both feet on the floor (double-limb support), slightly widened base, and reduced hip and knee rotations, all of which are commensurate with the patient’s reduced stride and gait velocity. This pattern of walking is a nonspecific compensatory response produced by most causes of impaired locomotion, including cortical dementia (Alzheimer’s disease). The features of cautious gait frequently dominate the clinical signs and symptoms of patients with mild neurologic impairment and provide the clinician with little clue to the underlying pathologic process.
2. Dysequilibrium is a disturbance of postural control and balance. Severe dysequilibrium produces a staggering, wide-based gait, particularly when the disturbance is acute. Mild or chronic dysequilibrium often is associated with a predominantly slow, cautious gait. Sudden or rapid movements (e.g., standing, turning, bending, and running) are avoided because they are destabilizing.
Sensory dysequilibrium occurs when there is a loss or conflict among vestibular, somatosensory, and primary visual pathways. Acute disturbances are more likely to produce falls, and disabling dysequilibrium generally does not persist unless at least two sensory modalities are impaired or unless there is concomitant impairment of the CNS. A cautious pattern of walking is typical among patients with isolated chronic peripheral visual, vestibular, or somatosensory deficits.
Vestibular dysequilibrium is associated with vertigo when the condition is acute. Patients with acute vestibular neuritis veer toward the side of the lesion and have horizontal nystagmus away from the lesion.
The head impulse sign is often positive with acute unilateral vestibular lesions. To elicit this sign, the patient is seated upright with the head positioned about 10° to one side. The patient is asked to fixate on the examiner’s nose, and the examiner quickly rotates the patient’s head 20° across the midline to the other side. When the head is rotated toward the side of a peripheral vestibular lesion, the eyes fail to rotate in the contralateral direction, due to the impaired vestibulo-ocular reflex. Consequently, head rotation is followed by a corrective saccade back to the examiner’s nose. Normally, the eyes should remain fixated on the examiner’s nose, resulting in no corrective saccade.
Nystagmus is typically unidirectional, away from the affected vestibular nerve, and is suppressed by visual fixation.
The Hallpike’s maneuver should be performed in all patients with episodic vertigo, particularly if the vertigo occurs with head movement (e.g., lying down, rolling over in bed, looking up, and bending over) (see Chapter 16).
Patients are able to stand and walk without assistance, despite their vertigo.
Somatosensory dysequilibrium is most evident when the eyes are closed (Romberg’s test) or otherwise impeded.
Visual dysequilibrium may occur when vision is acutely distorted with new glasses.
Dysequilibrium due to lesions in the CNS can cause profound loss of balance despite normal sensory feedback. Acute unilateral frontal lobe lesions cause patients to fall away from the side of the lesion. This dysequilibrium usually improves with time. Bilateral frontal lobe damage frequently causes more profound and sustained dysequilibrium due to inappropriate postural synergies. Patients lean the wrong direction in such a way that stability and locomotion are impeded. For example, patients may lean backward when being helped from a chair, or they may lean away from the pivot foot when attempting to turn. The patient’s rescue response to the pull test is absent or greatly reduced, resulting in a backward fall or retropulsion.
To perform the pull test, the patient assumes a normal stance, and the patient is instructed to take a step, if necessary, to prevent falling. The examiner then briskly pulls the patient backward at the shoulders, hard enough to pull the patient off balance. The examiner should stand far enough behind the patient to provide the patient adequate room to regain balance. The test is abnormal if the patient takes more than one or two steps to regain balance. The examiner must catch the patient, if necessary, to prevent a fall. The test should be done with a wall behind the examiner, providing the examiner with support if needed.
The pull test is an examination of the rescue response. It is not a test of balance or static stability. The pull test is not valid unless the patient is pulled off balance, necessitating a rescue response by the patient.
Subcortical dysequilibrium occurs with lesions in the basal ganglia, ventrolateral thalamus, or dorsolateral midbrain (midbrain locomotor region; Fig. 8.1). Acute unilateral lesions cause a tendency to fall backward and laterally away from the lesion. With ischemic lesions, the dysequilibrium is temporary unless the damage is bilateral. Progressive supranuclear palsy produces bilateral destruction of these sites, so early impairment of balance is common in this disorder.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree