Approach to the Patient with Abnormal Pupils
Aki Kawasaki
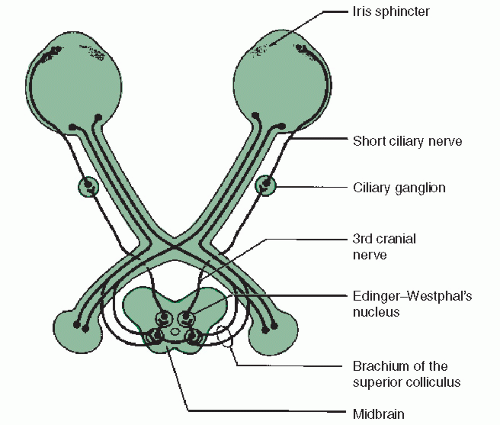
The pupillary light reflex is composed of an afferent limb and an efferent limb (Fig. 11.1). The afferent limb signals pupillomotor information from the retina to the dorsal midbrain. Except at the brachium of the superior colliculus and pretectal olivary nucleus, injury along the afferent limb of the pupil light reflex also results in some form of accompanying visual loss and in unilateral or asymmetric bilateral lesions, a relative afferent pupillary defect (RAPD) will be detected.The efferent limb of the pupil light reflex carries pupilloconstriction signals originating in the Edinger-Westphal subnucleus to the iris. Injury along the efferent limb causes mydriasis of the ipsilateral pupil and poor pupillary constriction to all forms of stimulation—direct light, consensual light, or near effort. (See the section on Unilateral Mydriasis.)
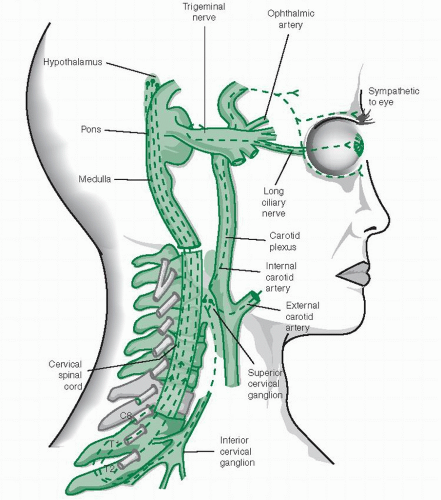
Pupillary dilation is a reflex response to sudden arousal or darkness and is mediated by the sympathetic pathway (Fig. 11.2). The pupil size at any moment is determined by the sum input of sympathetic and parasympathetic activity to two iris muscles, the radial dilator, and the sphincter.
I. PUPILLARY EXAMINATION
A. Hippus.
An awake patient sitting quietly in room light may show small spontaneous oscillations of pupil size, known as hippus. It reflects fluctuations in the modulating signals to the Edinger-Westphal subnuclei.
B. Pupil size.
Resting pupil size is greatest during the teenage years and then gradually decreases with increasing age. Asymmetry of pupil size of 0.4 mm or more is visible to the unaided eye and called anisocoria. When present, anisocoria should be measured in darkness and under bright light.
1. Anisocoria that is greater in magnitude under bright light implies a deficit of constriction, thus, the larger pupil is faulty.
2. Anisocoria that is more apparent in darkness or dim light implies a failure of dilation, thus, the smaller pupil is faulty.
C. Pupillary response to light.
Have the patient fixate on a distant target in a darkened room. Shine a bright focal light (a nonhalogen penlight is not bright enough) directly onto 1 pupil for 3 seconds and record the amplitude and velocity of constriction. Do this for each pupil 2 or 3 times for a mental “average.” Reminder: Simply noting that a pupil is “sluggish” or “responds poorly” to direct light stimulation is not enough information to differentiate an afferent from an efferent pupillary defect. Proceed to the alternating light test to distinguish an afferent pupil defect and check the pupil near response, which should be equally sluggish in the event of an efferent defect.
D. Alternating light test.
This is the standard clinical technique for identifying asymme try of afferent pupillomotor input between the 2 eyes, referred to as the relative afferent pupillary defect (RAPD)The patient usually has subnormal vision in the eye with an RAPD.
1. Technique.
Have the patient fixate a distant target in a dark room. Shine a bright focal light directly onto 1 pupil for 3 seconds, then quickly swing the light onto the other pupil for 3 seconds. Repeat this for 4 or 5 alternations of light stimulation and watch only the illuminated pupil (direct light response). The amplitude and velocity of pupillary constriction as well as the degree of redilation that occurs within the 3 seconds of light stimulation should be symmetric between the 2 eyes.
2. A large RAPD is present if the pupil of the “bad” eye dilates when the light is alternated back onto it after being on the “good” eye. In other words, the bad eye sees so much less light, compared to the good eye that reflex dilation occurs.
3. A small-to-moderate RAPD is sometimes difficult to detect. The bad eye generates enough afferent input to initiate pupillary constriction to direct light but it is a less vigorous response compared with that of the good eye. The pupil of the bad eye also “escapes,” that is, redilates sooner after the initial constriction.
II. RELATIVE AFFERENT PUPILLARY DEFECT
The presence of an RAPD is a sensitive indicator of unilateral or asymmetric injury to the afferent limb of the pupillary light reflex. If an RAPD is found, it needs to be investigated.
A. Ocular and retinal lesions.
1. Large unilateral retinal lesions such as central retinal artery occlusion or trauma produce an obvious RAPD. Visual acuity is generally poor. A dilated funduscopic examination usually provides the diagnosis.
2. Cataracts, corneal opacities, and vitreous lesions do not cause an RAPD, even when the visual loss is severe.
B. Optic nerve lesions.
1.Damage to the optic nerve almost always produces an RAPD and an accompanying visual field defect. Loss of acuity is variable.
2. The extent of damage in bilateral optic nerve disorders is rarely symmetric. Therefore, an RAPD is found on the side with greater damage. Look carefully.
C. Optic chiasm.
Lesions of the optic chiasm that produce bilateral but asymmetric visual dysfunction cause an RAPD in the eye with greater field loss.
D. Optic tract lesions.
Due differences in the retinal sensitivity between the nasal and temporal hemifields, a unilateral optic tract lesion can produce a small RAPD in the contralateral eye. Consider an optic tract lesion in any patient with complete homony mous hemianopsia and an RAPD in the eye with the temporal field loss.
E. Pretectal nucleus.
A unilateral dorsal midbrain lesion such as stroke or tumor that damages the pretectal olivary nucleus on one side can produce a small RAPD in the contralateral eye in the absence of visual loss. This is a rare occurrence.
III. MECHANICAL ANISOCORIA: “OPHTHALMOLOGIC” ANISOCORIA
Two iris muscles modulate pupil size and shape—the sphincter and the dilator. Damage to one or both iris muscles can distort the size, shape, and mobility of the pupil. Ocular pathologies such as trauma, infection, or surgery are common causes of a mechanical anisocoria. It is important to consider and identify ocular causes of anisocoria in order to avoid unnecessary neurologic evaluation.
A. History.
Inquire about any previous infection, inflammation, trauma, or surgery involv ing the eyes, including laser procedures.
B. Examination.
1. Marked irregularity of the pupillary margin, unusual distortion of pupillary shape, and a difference in iris color are structural iris defects that may be appreciated with direct observation.
2. A slit lamp examination of the iris is needed to identify most other causes of mechanical anisocoria such as synechiae (adhesions), small sphincter tears, transillumination defects, and inflammation. A dusting of iris pigment may be observed in a ring on the lens of a patient who has had a blow to the eye.
IV. UNILATERAL MYDRIASIS: NEUROLOGIC OR PHARMACOLOGIC
Once mechanical causes of anisocoria are ruled out, the next obvious step is to check the light reflex of both pupils. If the larger pupil constricts poorly to a bright light compared with the smaller pupil, then the larger pupil is the abnormal pupil. The neural pathway that mediates pupilloconstriction is the oculo-parasympathetic pathway. The preganglionic parasympathetic pupil fibers originate in the Edinger-Westphal subnucleus of the oculomotor and synapse in the ciliary ganglion of the orbit. The postganglionic parasympathetic pupil fibers are carried in the short ciliary nerves to innervate the iris sphincter and ciliary muscle. The neurotransmitter at the iris sphincter is acetylcholine. Three common nonocular conditions causing a large, poorly reactive pupil are oculomotor nerve palsy, a tonic pupil, and a pharmacologically dilated pupil.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree