Isolated facial numbness often is descriptive of impairment of sensation of the face as a result of dysfunction of the trigeminal system or central trigeminal pathways.
A. Patients may report unilateral or bilateral facial numbness, paresthesia (a spontaneous abnormal sensation), or dysesthesia (an unpleasant abnormal sensation produced by normal stimuli). There may be associated symptoms of altered sensation of the mucous membranes of the nose, mouth, gums, palate, or teeth. Facial numbness may be a part of a syndrome involving other cranial nerves, in addition to the trigeminal nerve. Trigeminal nerve dysfunction associated with pain is discussed in
Chapter 14.
B. Types. The types of facial numbness discussed in this chapter include conditions that may present with isolated facial numbness, including lesions of the trigeminal nerve branches (e.g., trauma, tumor, and connective tissue diseases), the gasserian ganglion (GG) or root (e.g., infection, tumors, and nontumorous masses), and the central tri geminal pathways (e.g., stroke, tumor, and vascular anomalies). Facial numbness is an uncommon, but not rare, condition. A patient with facial numbness may see a dentist, primary physician, neurologist, or otolaryngologist. The typical clinical scenario is gradual onset of numbness in one or more regions of the face, usually unilaterally. Because the presence of facial numbness can indicate a serious underlying condition, each patient with this symptom needs a thorough evaluation.
C. Facial numbness as a symptom of a life-threatening disorder. Facial numbness can represent not only a serious underlying condition that needs to be evaluated expedi tiously but also, in some rare instances, a medical condition that must to be dealt with as an emergency. In rare instances, facial numbness is the presenting sign of internal carotid artery dissection, carotid aneurysm, intracranial hemorrhage, or intracranial or nasopharyngeal tumor. However, in most instances, associated features point to one of these serious etiologic conditions. If there are features suggestive of carotid artery dis section or intracranial aneurysm, appropriate studies may include emergency CT or MRI of the brain and a vascular imaging study (helical cervical CT angiogra phy, MRI/MRA, or conventional cerebral angiography), depending on the area of concern. MRI of the head with contrast medium is indicated if there is suspicion of an intracranial tumor. Brain CT without contrast material is indicated if intracranial hem orrhage is a concern. An otolaryngology consultation should be obtained if symptoms suggest a nasopharyngeal tumor.
I. ETIOLOGY
A brief review of the trigeminal pathways is necessary for an understanding of the location of dysfunction with facial numbness.
A. Neuroanatomy of the trigeminal nerve.
1. The trigeminal nerve (cranial nerve V) is a mixed sensory and motor nerve.
The sensory portion of the nerve is the largest portion, transmitting sensation from areas of the face, oral cavity, and nasal passages.
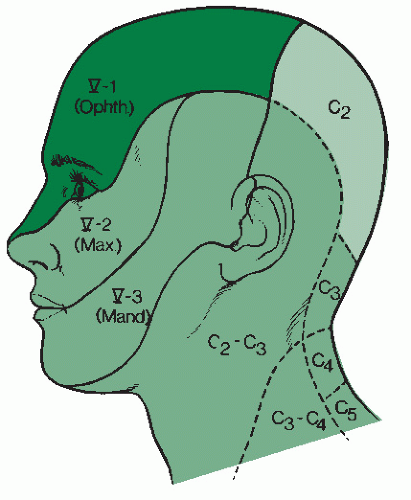
There are three divisions of the
sensory portion of the trigeminal nerve (
Fig. 13.1).
Ophthalmic (VI). The ophthalmic division provides cutaneous supply to the forehead and anterior scalp to approximately the vertex, parts of the nose and the upper eyelid, and the upper half of the cornea. Branches of this division to the facial structures are the nasociliary, infratrochlear, supratrochlear, lacrimal, and supraorbital nerves.
Maxillary (V2). The maxillary division provides cutaneous supply to portions of the nose, upper lip, cheek, lower half of the cornea, upper gums and teeth, palate, and nasal mucosa. Branches of this division are the zygomaticofacial, zygomaticotemporal, and infraorbital nerves.
Mandibular (V3). The mandibular division provides cutaneous supply to the lower lip; chin; portions of the jaw, ear, and mouth; lower gums and teeth; and the anterior two-thirds of the tongue. Branches of this division are the auriculotemporal, buccal, and mental nerves. The combined nerve trunk of the mandibular division and the motor portion gives rise to the inferior alveolar nerves and the lingual nerves.
The motor portion of the trigeminal nerve is a smaller division that travels with V3. It provides motor function to the muscles of mastication and the tensor tympani. This portion is not discussed further. However, it is important to examine the patient for dysfunction of the motor portion of the nerve.
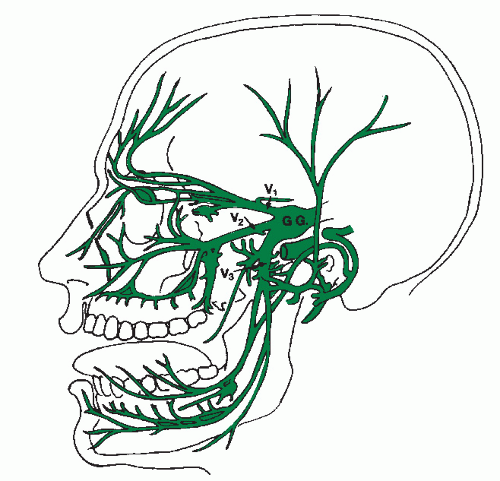
2. The three sensory divisions (V1, V2, and V3) enter the cranial cavity through the superior orbital fissure, foramen rotundum, and foramen ovale, respectively, to unite in the gasserian or semilunar ganglion, which lies at the apex of the petrous bones.
3. Second-order sensory neurons enter the pons at the sensory root.
B. Localization of the lesion with facial numbness
(
Table 13.1). Facial numbness usually is unilateral and can be partial or total. Complex facial numbness is numbness associated with other cranial nerve or brainstem findings. Bilateral numbness can be associated with brainstem involvement, leptomeningeal disease, or systemic diseases, or it can be idiopathic. There are some generalizations that help localize the lesion.
1. Lesions of the divisions of cranial nerve V have distinct areas of sensory loss (
Fig. 13.1).
2. Lesions proximal to the GG cause cutaneous numbness of the entire face and the anterior scalp (
Fig. 13.2).
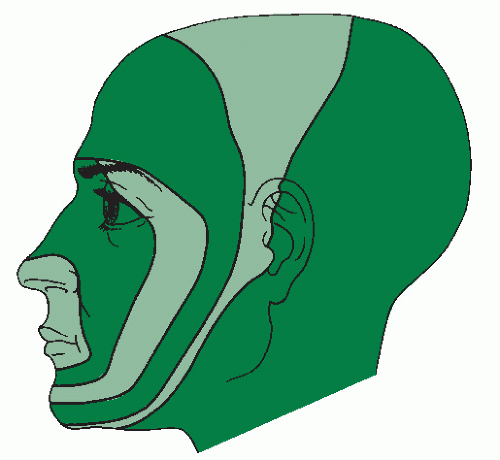
3. Lesions of the brainstem can produce an onionskin distribution of sensory loss (
Fig. 13.3).
4. Lesions of cranial nerve V typically spare the angle of the jaw, which is supplied by C2 and C3 (
Fig. 13.1).