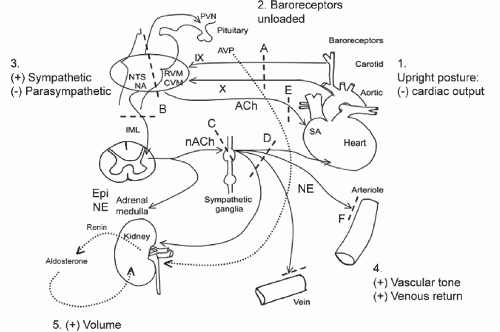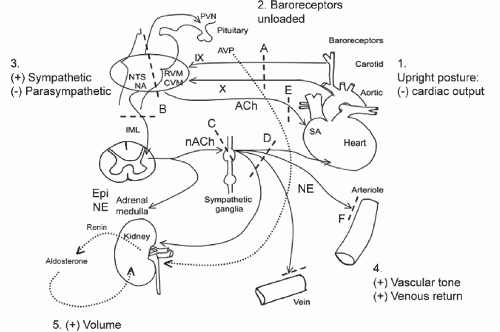
FIGURE 31.1 The baroreflex. 1. Standing produces “pooling” of 600-1,000 mL of blood to the lower body (mainly limb and splanchnic capacitance circulation), reducing venous return and cardiac output (by approximately 30%). 2. This is sensed by specialized stretch receptors (arterial and cardiopulmonary baroreceptors) that in turn activate (unload) baroreflexes. Inputs from carotid and aortic baroreceptors travel with the glossopharyngeal (IX) and vagus (X) nerves to converge on cardiovascular centers in the brainstem and medulla (mainly nucleus of the tractus solitarius) and their projections. 3. The physiologic baroreceptor reflex response to the volume shifts produced by upright posture is a compensatory increase in sympathetic tone with a decrease in parasympathetic outflow. 4. Sympathetic nerve terminals release NE that produces increased vasoconstriction of skeletal and mesenteric muscle vessels, HR, and cardiac contractility. Additional increases in venous return occur through a “pumping” effect of contracting limb and abdominal muscles engaged by the effort of standing (not shown). 5. A longer term response promoting extracellular fluid volume expansion includes baroreflexmediated release of renin, angiotensin, and aldosterone, leading to increased renal Na++ absorption, and release of vasopressin, with an increase in free-water absorption. A: Afferent baroreflex limb dysfunction is present when lesions involve baroreceptors and IX and X cranial nerves (neck surgery, radiotherapy, trauma, neuropathies, and autonomic disorders such as baroreflex failure, Holmes-Adie syndrome, and HSAN III). B: Central lesions involve the ventrolateral medulla (MSA), descending sympathetic pathways (medullary lesions, spinal cord lesions above T5), and IML (MSA, Lewy’s body disorders). C: Sympathetic ganglia lesions involve sympathetic ganglia (autoimmune ganglionopathies associated with nAChR antibodies or paraneoplastic, Lewy’s body disorders). D, E: Postganglionic sympathetic and efferent parasympathetic lesions are present with small fiber neuropathies (diabetes, amyloidosis, Sjögren’s syndrome, HSAN III). F: Efferent sympathetic neuroeffector junction dysfunction occurs with dopamine β–hydroxylase deficiency and α-1 adrenoceptor blocking drugs. nAChR, nicotinic acetylcholine receptor antibodies; AVP, arginine vasopressin; CVM, caudal ventrolateral medulla; Epi, epinephrine; HSAN III, hereditary sensory autonomic neuropathy type III; IML, intermediolateral cell columns of the spinal cord; NA, nucleus ambiguus; NE: morepimephrime NTS, nucleus tractus solitarius; RVM, rostral ventrolateral medulla; SA, sinus node. |