FIGURE 9.1 Example of a typical week-at-a-glance sleep diary.
1. Adjustment (acute) insomnia. This term has been used to describe insomnia that immediately follows a clearly identifiable stressor and is expected to resolve when the stress ends or the patient adapts. Adjustment insomnia is often associated with anxiety and depression related to the specific stressor.
2. Psychophysiologic insomnia. This is a conditioned insomnia due to learned, sleep-preventing associations. It can represent persistent adjustment insomnia, where an external (or internal) stressor leads to a state of arousal “racing mind” in association with bedtime at home (patients often sleep better in the sleep lab; the “reverse first-night effect”).
3. Paradoxical insomnia. Patients complain of severe insomnia with no objective evidence of disturbed sleep or daytime impairment. PSG studies show that these individuals overestimate their sleep latencies and underestimate their sleep times. Patient concerns are not alleviated when they are presented with these objective findings. High-frequency activity on electroencephalographic power-density measures may alter sleep perception in this patient population.
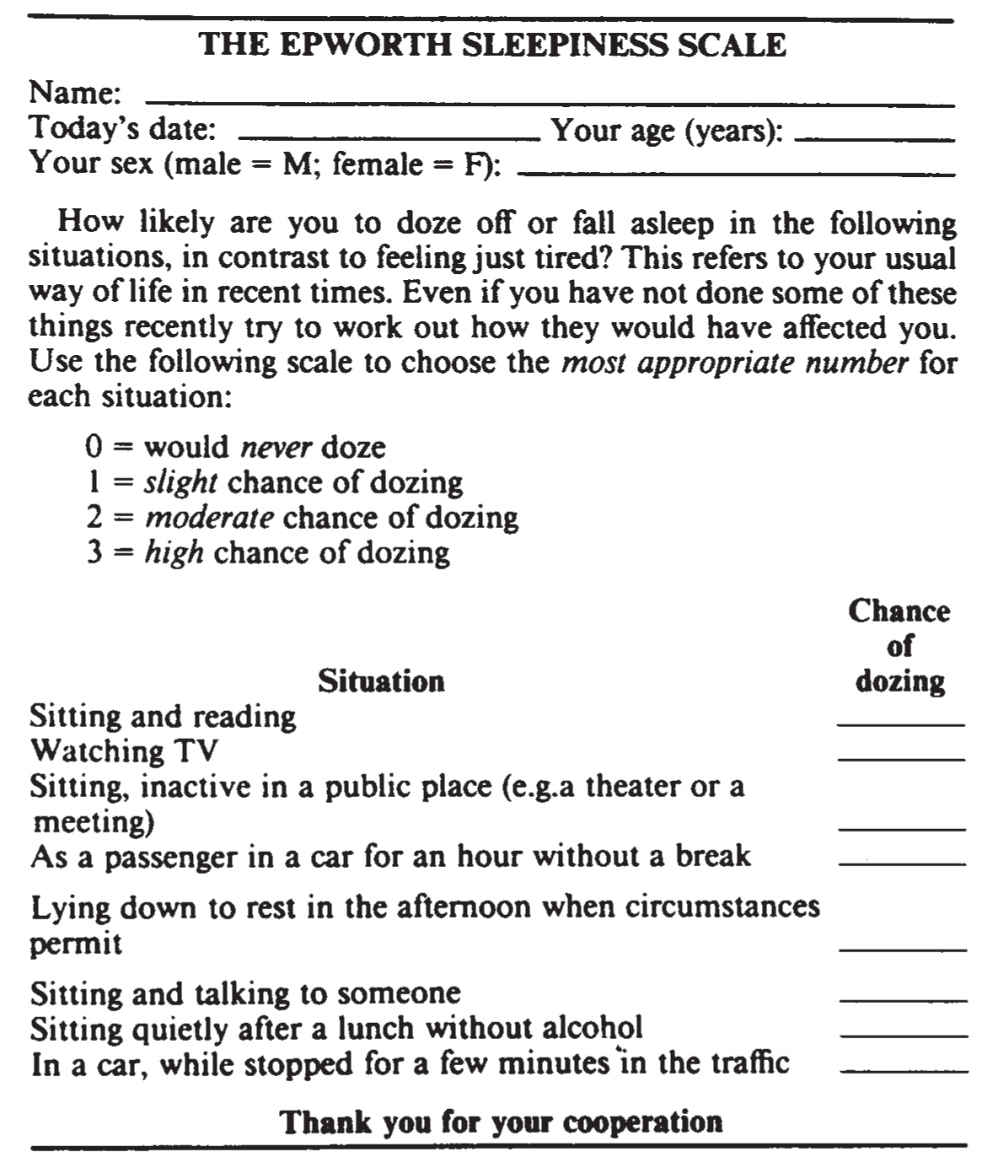
FIGURE 9.2 The Epworth sleepiness scale. A score of 10 or greater suggests EDS. (From Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545, with permission.)
4. Idiopathic insomnia. This lifelong disorder is reported in 1% of young adults, beginning in infancy or early childhood. It has no known precipitators or major psychological concomitants, but may be associated with attention-deficit/hyperactivity disorder (ADHD) and dyslexia. A genetic abnormality in sleep/wake mechanisms is suspected. PSG often shows reduced body movements despite severely disturbed sleep.
5. Insomnia due to (another) mental disorder. In this diagnosis, insomnia is a symptom of a mental disorder, but its severity demands treatment as a distinct problem, which often improves the underlying mental disorder. Major depression is frequently associated with insomnia and reduced rapid eye movement (REM) sleep latency, but PSG is not needed for diagnosis.
6. Inadequate sleep hygiene. This presents as a primary or secondary diagnosis in over 30% of sleep-clinic patients. It involves two categories of habits inconsistent with good sleep: practices that produce increased arousal (e.g., caffeine and nicotine use) and practices that are inconsistent with the principles of sleep organization (variable bedtime and awakening times). Important factors can include engaging in mentally or physically stimulating activities too close to bedtime and failure to maintain a comfortable sleeping environment.
7. Behavioral insomnia of childhood. There are two types seen in up to 30% of children (possibly more frequent in boys) after 6 months of age. Sleep-onset association type occurs with dependency on a specific stimulation, object, or setting for sleep. Sleep-onset associations are extremely prevalent and are only a disorder if highly problematic. Limit-setting type occurs with bedtime stalling, or refusal in toddlers and preschoolers. This problem is often due to poor practices of the caregiver.
8. Insomnia due to drug or substance. This is suppression or disruption of sleep during consumption or exposure to a drug, food, or toxin, or upon its discontinuation. The PSG in chronic alcohol withdrawal can reveal light and fragmented sleep that may persist for years.
9. Insomnia due to a medical condition. Disorders that cause discomfort (comfort is necessary for normal sleep) and neurodegenerative problems (with disruption of normal central sleep/wake mechanisms; poorly formed or absent sleep spindles are common) are representative of many possible etiologies. This diagnosis should only be considered when insomnia causes marked distress and warrants specific attention.
B. Sleep-related breathing disorders (SRBDs). In addition to the wake/sleep history, PSG is required in diagnosing SRBDs. PSG is the combined sleep monitoring of electroencephalography (EEG), electromyography (EMG), electrooculography (EOG), and physiologic measures that include airflow, respiratory effort, and oxygen saturation (Sao2). PSG differentiates four sleep stages—non-REM (NREM) stages N1, N2, and N3, and REM (stage R). An obstructive apnea is a drop in airflow by ≥90%, in association with continued inspiratory effort, for ≥10 seconds in adults, or the duration of two baseline breaths in children. A central apnea is an absence of inspiratory effort for ≥10 seconds in adults, or, in children, for 20 seconds, or the duration of two baseline breaths in association with an arousal, awakening, or a ≥3% Sao2 reduction. A mixed apnea occurs when there is initially absent inspiratory effort, followed by resumption of inspiratory effort in the second part of the event. Hypopneas in adults occur with a ≥10-second period of reduced airflow of ≥30%, with an Sao2 reduction of ≥3% (or an associated arousal). In children, a hypopnea requires a ≥30% fall in airflow for duration of two baseline breaths, in association with an arousal, awakening, or ≥3% Sao2 reduction. Severity of an SRBD is suggested by the apnea–hypopnea index (AHI)—the average number of apneas and hypopneas per hour of sleep.
1. Obstructive sleep apnea disorders. Obstructive sleep apnea (OSA) is associated with repeated episodes of upper airway obstruction. From 30 to 60 years of age, the prevalence ranges from 9% to 24% for men and 4% to 9% for women. Obstructions often result in oxygen desaturation, elevation in Paco2, and arousals, which disrupt sleep continuity and can lead to EDS. This syndrome often occurs among sleepy, middle-aged, overweight men with insomnia who snore. Premenopausal women are less commonly affected. This disorder has also been associated with systemic and pulmonary hypertension, nocturnal cardiac arrhythmia and angina, gastroesophageal reflux, nocturia, and an overall reduction in quality of life. Predisposing factors include familial tendencies, redundant pharyngeal tissue (e.g., adenotonsillar hypertrophy), craniofacial disorders (e.g., micrognathia, retrognathia, nasal obstruction), endocrinopathy (e.g., acromegaly, hypothyroidism with myxedema), and neurologic disease.
a. OSA, adult
(1) History. The patient or bed partner often reports restless, unrefreshing sleep and sleep maintenance insomnia with arousals associated with gasping, choking, or heroic snoring, possibly exacerbated by fatigue, alcohol, weight gain, or the supine sleeping position. Snoring may force the person to sleep alone and persist even when sitting. Although patients may not report daytime sleepiness, problems with fatigue, memory, and concentration are frequent. A family history of similar problems should be carefully sought.
(2) Examination. The blood pressure, body mass index (BMI—weight in kilograms per square meter of height), and neck and waist circumference should be documented, as hypertension and obesity may relate to OSA. Of general concern (following western standards) are a BMI ≥ 30 kg/m2, a neck circumference of >40 cm (15.7 inches), and a waist circumference (often measured at the iliac crest) >102 cm (40.2 inches) in men, and >88 cm (34.6 inches) in women. These are frequent signs in OSA that may predict comorbidities in the metabolic syndrome, heart disease, and stroke. Oral and nasopharyngeal patency and abnormalities of the tonsils, adenoids, tongue, soft and hard palate, uvula, nasal septum, turbinates, and temporomandibular joint as well as fatty infiltration of soft tissues in the upper airways should be documented.
(3) PSG. Recurrent obstructions and respiratory effort-related arousals (RERAs) contribute to EDS. (However, the frequency of events correlates poorly with sleepiness severity.) Events generally appear worse in the supine position and during REM sleep. Tachy–brady cardiac arrhythmias and asystole may be documented. The diagnosis of OSA is considered with an obstructive AHI, or respiratory disturbance index (RDI; the obstructive AHI + the average number of RERAs/hour of sleep) ≥5, and when there is at least one symptom; EDS, insomnia, arousals with shortness of breath or choking, and witnessed loud snoring/apneas, or significant comorbidity; arterial hypertension, coronary artery disease, congestive heart failure (CHF), atrial fibrillation, stroke, mood disorders, or diabetes. The diagnosis is also given whenever the obstructive AHI or RDI is ≥15 (even in the absence of symptoms or comorbidities).
(4) Differential diagnosis. Loud snoring and RERAs, as part of the upper airway resistance syndrome (UARS), can lead to EDS without the standard PSG evidence of OSA (as RERAs are pathophysiologically similar to obstructions). During PSG, defining RERA requires esophageal balloon (or nasal pressure/inductance plethysmography) monitoring that reveals ≥10 second episodes of respectively increasing negative pressure, or flattening of nasal pressure waveforms (that correspond to increased respiratory effort), which terminate with arousal. In addition, isolated snoring, central sleep apnea (CSA), nonobstructive alveolar hypoventilation, narcolepsy, and restless legs syndrome (RLS) may manifest similarly to OSA in regard to disruptive sleep and EDS.
(5) Other tests. In severe cases, an interdisciplinary approach may necessitate electrocardiography, chest radiography, echocardiography, and pulmonary function tests (addressing pulmonary hypertension and right ventricular hypertrophy), cephalometric evaluations of the upper airways, and extensive cerebrovascular assessments.
b. OSA, pediatric. The prevalence of OSA is 2% in the general pediatric population, with girls and boys being affected equally, but with a higher prevalence in African American relative to White children. Some children may have OSA breathing patterns similar to adults; nevertheless, younger children may be prone to obstructive hypoventilation (long periods of persistent partial upper airway obstruction).
(1) History. Snoring and difficulty breathing are common, often with reports of associated neck hyperextension and diaphoresis. Cognitive and behavioral complications (ADHD) are frequent, with EDS being reported especially in older children.
(2) Examination. Although children can have OSA secondary to large tonsils and adenoids, obesity is becoming a more common etiology. Pectus excavatum may result from chronic paradoxical respirations. Patients with craniofacial abnormalities, Down syndrome, neuromuscular diseases, cerebral palsy, gastroesophageal reflux (with upper airway edema), mucopolysaccharidosis, sickle cell disease, or who are post cleft palate repair may be prone to OSA.
(3) PSG. Even relatively short obstructions may lead to severe hypoxemia as children have faster respiratory rates with lower functional residual capacities than adults. OSA in children is defined by an obstructive AHI ≥1.
(4) Differential diagnosis. In children, UARS, isolated snoring, CSA, nonobstructive alveolar hypoventilation, narcolepsy, and RLS may manifest similar to OSA in regard to disruptive sleep and EDS. In the pediatric PSG, RERAs are defined by a sequence of ≥2 breaths, characterized by increasing respiratory effort, flattening of the inspiratory portion of the nasal pressure waveform, snoring, or an elevation in the end-tidal Pco2 leading to an arousal from sleep.
2. CSA syndromes
a. CSA with Cheyne–Stokes breathing (CSB). PSG defines CSB as at least three consecutive cycles of a crescendo/decrescendo breathing with a central AHI of ≥5, and/or a cyclic crescendo/decrescendo pattern that lasts ≥10 consecutive minutes. CSB is most prominent in NREM sleep (usually absent or attenuated in REM). It occurs predominately in men >60 years of age, with a prevalence up to 45% in CHF, and in 10% of strokes. CHF (a poor prognostic sign), stroke, and possibly renal failure are the most important precipitating factors.
b. CSA due to a medical disorder without CSB. A majority of the medical conditions with CSA are associated with brainstem lesions and cardiac or renal disorders.
c. CSA due to high-altitude periodic breathing. The only known predisposing factor to this disorder is when an individual has an increased hypoxic ventilatory responsiveness. This leads to hyperventilation on rapid ascent to altitudes >4,000 m and a hypocapnic alkalosis that, during sleep, inhibits ventilation (usually the first night), leading to central apneas in NREM sleep that alternate with hyperpneas in cycles of 12 to 34 seconds (often leading to shortness of breath, frequent arousals, and EDS). This is considered a normal, and transient, adaptive phase to higher altitudes.
d. CSA due to medication or substance. Regular use (>2 months) of long-acting opioids (methadone and time-release morphine and hydrocodone) can lead to CSA (often in association with obstruction, hypoventilation, and periodic breathing). The presumed etiology is from an effect on µ-receptors on the ventral surface of the medulla.
e. Primary CSA. This idiopathic disorder is more frequent in middle-aged to elderly males, associated with a low-normal waking Paco2 (<40 mm Hg), and high chemoresponsiveness (evidenced as central apneas) to the normal rise in PaCO2 that occurs in sleep. Significant primary CSA with an AHI >5 can lead to arousals with shortness of breath, insomnia, and EDS.
f. Primary CSA of infancy (apnea of prematurity <37 weeks conceptual age, apnea of infancy ≥37 weeks, ≤1 year conceptual age). Central, mixed, obstructive apneas or hypopneas (most notably in active/REM sleep) associate with signs of physiologic compromise (hypoxemia, bradycardia, the need for resuscitative measures), but progressively decrease as the patient matures during the early weeks of life. The prevalence varies inversely with conceptual age (in 84% of infants <1,000 g, and <0.5% of full-term newborns), as it is related to developmental immaturity of brainstem respiratory centers. This has not been established as an independent risk factor for sudden infant death syndrome.
3. Sleep-related hypoventilation disorders. These syndromes often coexist with elements of OSA and CSA.
a. PSG. In adults, hypoventilation during sleep can be scored in either of the following situations: if there is an increase in the arterial Pco2 (or surrogate; transcutaneous or end-tidal Pco2) to a value >55 mm Hg for ≥10 minutes, or there is ≥10 mm Hg increase in arterial Pco2 (or surrogate) during sleep (in comparison with an awake supine value) to a value exceeding 50 mm Hg for ≥10 minutes. In children, hypoventilation during sleep can be scored when >25% of the total sleep time as measured by either the arterial Pco2 (or surrogate) is spent with a value >50 mm Hg.
(1) Obesity hypoventilation syndrome. These patients must hypoventilate (as defined by an arterial PaCO2 [or surrogate] >45 mm Hg) while awake, and the hypoventilation must be primarily related to mass loading from obesity (as defined by a BMI >30 kg/m2; >95th percentile for age and sex for children). Prolonged periods of decreased tidal volume and sustained arterial oxygen desaturation (for several minutes) are usually seen, but not required for diagnosis. OSA is diagnosed as a separate entity in 80% to 90% of these patients. The serum bicarbonate level is routinely elevated secondary to renal compensation for the respiratory acidosis that follows chronic hypercapnia.
(2) Congenital central alveolar hypoventilation syndrome (CCHS). CCHS can lead to polycythemia, pulmonary hypertension, heart failure, and death. It is a rare congenital genetic disease (most cases due to de novo mutations in the PHOX2B gene) associated with failure of automatic central control of breathing, usually evident at birth, and requiring intubation. Most patients have a polyalanine point mutation and severity relates to a greater number of polyalanine repeats. Patients may progress to adequate waking breathing with normal daytime PaCO2 levels, although some continue to show daytime hypoventilation, and others may need continuous ventilatory support. All will continue to require ventilatory support during sleep. Rarely individuals can present in adulthood, especially when stressed with general anesthesia or respiratory illness. Although central apneas may occur, the PSG primarily shows hypoxemia and hypercapnia that associate with decreased tidal volume and respiratory rate, with hypoventilation generally appearing worse during slow wave (stage N3) sleep. CCHS is often associated with Hirschsprung’s disease (approximately 16%), autonomic dysfunction, neural tumors, and dysphagia.
(3) Sleep-related hypoventilation due to a medical disorder. This section includes a variety of disorders.
(a) Lower airway obstruction occurs in disorders with obstruction or increased airflow resistance below the larynx, such as chronic obstructive pulmonary disease (COPD); chronic bronchitis and emphysema; bronchiectasis; cystic fibrosis; and α1 antitrypsin deficiency. The greatest risk factor for COPD (the third leading cause of death in the United States) is cigarette smoking. Patients with COPD and significant sleep hypoxemia have increased pulmonary hypertension and mortality. Lower airway obstructive disease is evidenced by a forced expiratory volume exhaled in one second/forced vital capacity ratio <70% of predicted values.
(b) Pulmonary parenchymal or vascular pathology can be documented using pulmonary function tests, radiography, echocardiography, pulmonary artery catheter measurements, and hemoglobin studies. Associated diseases include interstitial lung diseases, pulmonary hypertension, sickle cell anemia, and cystic fibrosis. Worse pulmonary function and a lower waking SaO2 increases the risk for sleep hypoventilation/hypoxemia, and subsequent polycythemia and cardiac dysrhythmias. PSG findings are generally worse in REM sleep.
(c) Neuromuscular and chest wall disorders can cause hypoventilation secondary to reduced contractility of the ventilatory musculature (intercostals, accessory muscles, and diaphragm), or due to anatomic distortion of the chest wall (which causes inefficient breathing). This often affects patients with obesity, amyotrophic lateral sclerosis, myasthenia gravis, muscular dystrophies, kyphoscoliosis, postpolio syndrome, and spinal cord injuries with diaphragmatic paralysis. The course of the breathing disturbance approximates the severity of the underlying condition, and can put the patient at risk for pulmonary hypertension, cor pulmonale, and cognitive dysfunction. Spirometry in patients with neuromuscular and chest wall disorders generally reveals a restrictive ventilatory dysfunction, with a forced vital capacity that is frequently <50% of predicted.
C. Central disorders of hypersomnolence. These disorders involve dysfunction of the normal central wake/sleep centers. The ascending reticular activating system (ARAS) of the brainstem promotes wakefulness through two pathways, leading to diffuse cortical projections. A ventral hypothalamic system excites the lateral nucleus (LN) and tuberomammillary nucleus of the hypothalamus, which relays to cholinergic basal forebrain cells, while a dorsal thalamic route stimulates nonspecific midline and intralaminar nuclei, while inhibiting the reticular nucleus of the thalamus. The central sleep-onset system has a hypothalamic “sleep switch” in the preoptic area of the hypothalamus (the ventrolateral and median preoptic nuclei). These nuclei have reciprocal inhibitory relays with multiple waking centers.
1. Narcolepsy (types 1 and 2). Classically begins during puberty or young adulthood with EDS. Sleep attacks can occur while driving, engaged in active conversation, or eating. Once sleepiness stabilizes, it generally does not progress, but the other symptoms associated with narcolepsy may come and go. Cataplexy, often precipitated by strong positive emotion (usually mirth), involves attacks that range from brief sensations of weakness to essential paralysis. The spells are transient and do not produce cognitive impairment. Thirty-three percent to eighty percent of narcoleptics have the ancillary symptoms of hallucinations and sleep paralysis. Hypnagogic (at sleep onset) and hypnopompic (on awakening) hallucinations are generally frightening visual, auditory, or movement perceptions that essentially represent dreaming while awake. Sleep paralysis occurs during the transition from sleep to waking (or waking to sleep). The patient may experience brief paralysis (seconds to minutes) with the inability to speak. Other symptoms of narcolepsy can include insomnia, poor memory, depression, and automatic behaviors. Narcolepsy is associated with pathologic REM sleep mechanisms, clinically evidenced as EDS, cataplexy, sleep paralysis, and hypnagogic/hypnopompic hallucinations. In narcolepsy type 1 these symptoms are due to a deficiency of wake-promoting neuropeptides (orexins/hypocretins) in the LN of the hypothalamus, as defined by cerebrospinal fluid (CSF) hypocretin (Hcrt)-1 concentration, measured by immunoreactivity, as either ≤110 pg/mL or <1/3 of mean values obtained in normal subjects with the same standardized assay. Narcoleptics with cataplexy, and approximately 24% of narcoleptics without cataplexy, have low CSF Hcrt-1 concentrations and are given the formal diagnosis of narcolepsy type 1. Narcoleptics without cataplexy and with CSF Hcrt-1 levels >110 pg/mL or >1/3 of mean values obtained in normal subjects with the same standardized assay are given the formal diagnosis of narcolepsy type 2. Another clinical and pathophysiologic subtype is narcolepsy type 1 due to a medical condition, primarily central nervous system (CNS) disorders with lesions of the hypothalamus resulting from head trauma, tumors, or autoimmune and paraneoplastic disorders associated with anti-Ma2 or anti-aquaporin-4 antibodies.
a. PSG and the multiple sleep latency test (MSLT). The diagnosis of narcolepsy requires objective measurements, and includes documenting abnormalities of REM sleep utilizing PSG/MSLT. These evaluations should be preceded by at least 1 week of actigraphic recording with a sleep log to help rule out insufficient sleep, shift work, or another circadian sleep disorder that could appear similarly on PSG/MSLT. The patient must also discontinue any drug that affects their sleep for a minimum of 14 days (or five times the half-life of the drug and its metabolites) prior to the PSG/MSLT. This should be confirmed with a urine drug screen. REM sleep is defined on PSG and MSLT as a “relatively low voltage, mixed frequency EEG” of alpha and theta waveforms, associated with “saw-tooth” waves, which occurs with an EOG that shows REMs and an EMG that documents atonia. In diagnosing narcolepsy, the MSLT should be performed approximately 2 hours after the patient awakens from the overnight PSG (which assures adequate sleep, with the goal of at least 7 hours of sleep, and a paucity of other sleep disorders, including SRBDs). The MSLT is a series of five 20-minute attempts at napping (during the patient’s normal waking hours), which are separated by approximately 2-hour intervals. A mean sleep latency (the average time it takes the patient to fall asleep after the beginning of each individual nap period) ≤8 minutes and two or more naps during which REM sleep appears (a sleep-onset rapid eye movement period [SOREMP]) are classically associated with narcolepsy. A SOREMP (within 15 minutes of sleep onset) on the preceding PSG may replace one of the SOREMPs required for diagnosis on the MSLT.
b. Split-screen, video-PSG studies. As patients are infrequently examined during a cataplexy attack, the suspicion of cataplexy is usually based on the clinical history. Nevertheless, split-screen, video-PSG studies in individuals with frequent spells, performed during actual cataplectic events precipitated by emotional provocation, have shown REM sleep patterns during periods when patients were able to give appropriate responses to detailed questioning. Similar results have been documented during episodes of sleep paralysis and hypnagogic hallucinations.
c. Genetics. The risk of narcolepsy type 1 in first-degree relatives of affected patients is 1% to 2% (a 10-fold to 40-fold risk increase). Relatives of individuals with narcolepsy type 1 may be prone to partial narcolepsy symptoms suggesting narcolepsy type 2. The major histocompatibility complex of chromosome 6 contains genetic markers for narcolepsy. For nearly all patients with narcolepsy type 1 the mapping of specific human leukocyte class II antigens (DQ1 and DR2) reveals a subtype human leukocyte antigen allele DQB1*0602. The presence of the DQB1*0602 allele in approximately 45% of patients narcolepsy type 2 (and in 12% to 38% of controls) indicates that genetic testing alone is not sufficient for the diagnosis of narcolepsy.
d. Orexins/hypocretins. Narcolepsy type 1 is caused by a deficiency of LN hypothalamic hypocretin (orexin) wake-promoting neuropeptide signaling, and approximately 24% of narcoleptics without cataplexy have low CSF Hcrt-1 levels (8% have intermediate levels; >110 pg/mL, ≤200 pg mL).
2. Idiopathic hypersomnia. This is generally a lifelong disorder (remission rate of 14%) of EDS, which routinely begins in adolescence (mean age of onset 16.6 to 21.2 years), and is associated with self-reported routine total sleep times ≥10 hours in at least 30% of patients. The use of 24-hour PSG monitoring has documented 24-hour sleep times (major sleep episode plus naps) ≥660 minutes. About 36% to 66% report sleep inertia (sleep drunkenness), defined as prolonged difficulty waking with automatic behaviors and confusion. About 46% to 78% of patients report long (often >1 hour) unrefreshing naps. There are no reports of cataplexy and no more than 1 SOREMP on PSG/MSLT studies, while the mean sleep latency averages 7.8 to 8.3 minutes. The autonomic concomitants implied by the frequency of associated headaches, orthostasis, perception of temperature dysregulation, and Raynaud’s-type phenomena suggest hypothalamic dysfunction; nevertheless, relatively recent CSF studies have shown normal orexin/hypocretin and histamine levels.
3. Kleine–Levin Syndrome (KLS). The KLS is rare (prevalence of 1 to 2 cases per million; 500 cases reported) and begins during the second decade in 81%, with a male–female ratio of 2:1. It is characterized by baseline normalcy interrupted by relapsing-remitting episodes of hypersomnolence associated with cognitive, psychiatric, and behavioral disturbances. The first episode is often associated with an infection or alcohol use, and recurs every 1 to 12 months (median 3 months), typically resolving after a median of 14 years. During episodes the patient may sleep as long as 20 hours, are generally amnestic for waking confusion, hyperphagia (66%), hypersexuality (53% primarily men), infantile/depressed behaviors (53%; primarily women), and hallucinations/delusions (30%). Birth and developmental problems and Jewish heritage are risk factors for KLS. In addition, the frequency of HLA DQB1*02 was increased in one retrospective, multicenter study of 30 KLS patients. Brain MRI is normal, but functional brain imaging during episodes is frequently abnormal, variably showing hypometabolism in the thalamus, hypothalamus, mesial temporal lobe, and frontal lobe, with half of the patients showing persistent abnormalities when asymptomatic. Postmortem examinations have been performed in four cases with inconsistent findings that include perivascular lymphocytic infiltrations in the hypothalamus, thalamus, amygdala, grey matter of the temporal lobes, diencephalon, and mesencephalon, raising on occasion the suspicion of localized encephalitis. An autoimmune etiology is suggested by the combined clinical onset during adolescence that is often associated with infection and the HLA DQB1*02. Finally, menstrual-related KLS is a very rare clinical and pathophysiologic subtype (18 reported cases), where episodes occur exclusively just before or during menses. Response to estrogen and progesterone has suggested a reproductive disturbance in these cases.
4. Hypersomnia due to a medical condition. The conditions that can cause hypersomnia through direct effects on wake/sleep mechanisms include neurodegenerative disorders, brain trauma and tumors, encephalitis, genetic disease, and stroke. The diagnosis of narcolepsy type 1 due to medical condition is given when these conditions lead to cataplexy.
a. Hypersomnia secondary to Parkinson’s disease. In Parkinson’s disease (PD), hypersomnia may result from degeneration of dopaminergic cells in the substantia nigra and cholinergic neurons in the basal forebrain.
b. Posttraumatic hypersomnia. Hypersomnolence has been reported with a frequency of 28% in traumatic brain injury. This type of hypersomnia has been reported even in mild head injury (without loss of consciousness), and also during recovery from posttraumatic coma (where early PSG return of sleep spindles and normal sleep–wake cycling is a positive prognostic sign). In some cases this hypersomnolence may result from injury to the hypothalamic hypocretin/orexin neurons or other wake-promoting centers in the brain.
c. Genetic disorders associated with primary CNS somnolence. Specific genetic disorders associated with hypersomnia include Norrie’s disease, Niemann–Pick type C disease, myotonic dystrophy, Prader–Willi syndrome, fragile X syndrome, and Moebius syndrome. In Niemann–Pick disease type C, accumulation of unesterified cholesterol and sphingolipids in the hypothalamus, with a subsequent reduction in orexin/hypocretin, may be a cause of sleepiness. In myotonic dystrophy, hypothalamic (orexin/hypocretin) dysfunction, and loss of serotonin in the dorsal raphe nucleus, may account for hypersomnolence. Smith–Magenis syndrome is associated with reversal in the normal pattern of melatonin secretion (serum levels are high during the day, rather than at night).
d. Hypersomnias secondary to brain tumors, infections, or other CNS lesions. Tumors, infections, strokes, sarcoidosis, or neurodegenerative lesions especially in the hypothalamus or rostral midbrain can produce EDS.
e. Hypersomnia secondary to endocrine disorders. Hypersomnia secondary to endocrine disorder is typified by hypothyroidism. A significant reduction in slow wave activity can be induced by hypothyroidism.
f. Hypersomnia secondary to metabolic encephalopathy. This includes encephalopathies related to hepatic, renal, adrenal, and pancreatic failure, toxin exposures, and some inherited childhood metabolic disorders.
g. Residual hypersomnia in patients with adequately treated OSA. Residual sleepiness in this population may be caused by hypoxic injury to central monoamine waking systems.
5. Hypersomnia due to a medication or substance. This includes use, abuse, and cessation of stimulants, and sedative-hypnotic drugs.
6. Hypersomnia associated with a psychiatric disorder. These are related to psychiatric conditions that include adjustment, personality, schizoaffective, mood, and seasonal affective disorders. Subtypes include hypersomnia associated with a major depressive episode (atypical depression and bipolar type II disorder), and conversion disorder (or as an undifferentiated somatoform disorder).
7. Insufficient sleep syndrome. This is due to voluntary, but unintentional, chronic sleep deprivation. Patients are preoccupied with etiologies they presume are responsible for their sleepiness (causes other than a reduced total sleep time), and their symptoms, which may include irritability, malaise, and reduced concentration.
D. Circadian rhythm sleep–wake disorders. A circadian rhythm sleep–wake disorder (CRSWD) occurs when there are incongruities between the sleep–wake schedule demanded by society and the intrinsic sleep–wake pattern of the patient (determined in large part by the circadian pacemaker—the suprachiasmatic nuclei of the anterior hypothalamus). When not extrinsic or self-imposed (“jet lag” or shift work), these problems are believed to result from abnormal intrinsic physiologic responses to environmental time cues (Zeitgebers) such as sunlight (which exerts its effects through retinal–hypothalamic pathways). The patient’s state of sleepiness or arousal subsequently is out of synchrony with that of the general population. The result is alternating sleepiness and insomnia when the patient tries to follow a normal schedule.
1. History. In many cases, a sleep log can be diagnostic. The accurate, 1- to 2-month documentation of all bedtimes, final awakening times, and nap times can help differentiate a circadian rhythm disorder from poor sleep hygiene. The log should be filled out during a vacation or “free” time so as to avoid societal constraints that prevent the patient from following their intrinsic sleep–wake pattern.
2. Other tests. Actigraphy is a method for recording limb movement using a device (usually placed on the wrist) that records movement. Digitized data are downloaded to a computer, and computer algorithms are used to approximate wake and sleep periods over prolonged periods of time. The American Academy of Sleep Medicine (AASM) indicates actigraphy is reliable and valid for detecting sleep in healthy populations, and useful in the routine evaluation of CRSWDs, insomnia, and EDS. In addition, some sleep disorder centers can monitor hormonal rhythms [such as dim-light melatonin onset], and 24-hour body temperature fluctuations, which can lose normal circadian fluctuations and amplitudes in CRSWDs.
a. Delayed sleep–wake phase disorder. This occurs with a prevalence rate up to 16%, and is primarily noted in adolescents and young adults, and individuals with evening-type personalities (as defined by the Horne–Ostberg questionnaire). There is an association with polymorphisms in the circadian clock gene hPer3, with a positive family history in 40%. Patients report chronically late bedtimes with late final awakening times (delayed over 2 hours relative to societal norms), which can be confirmed with a sleep logs and actigraphy (over at least 7 days). These individuals do not report sleepiness unless they attempt to follow the normal societal sleep–wake schedule.
b. Advanced sleep–wake phase disorder. Persons with this syndrome go to sleep very early in relation to the setting of the sun, arise very early in relation to sunrise, and do not report excessive sleepiness during their “normal” waking hours. This tendency increases with age, and has a prevalence of 1% in middle-aged and older adults. Almost all patients are considered morning-type personalities. In younger patients genetic factors may be involved, possibly with an autosomal-dominant inheritance pattern, in association with a mutation in the circadian clock gene hPer2. This CRSWD is generally addressed only if it impairs the quality of the patient’s work, social, or family life.
c. Irregular sleep–wake rhythm disorder. In this disorder there is no definitive sleep–wake rhythm. Patients subsequently have intermittent nocturnal insomnia and variable periods of daytime sleepiness, which generally result in three or more irregularly timed naps during a 24-hour period. The total sleep time during a 24-hour is normal, but the timing of sleep is not predictable. This disorder can be seen in the institutionalized elderly, in association with dementia, and in children with intellectual disabilities.
d. Non-24-hour sleep–wake rhythm disorder. Also known as hypernychthemeral syndrome, these patients have an inability to synchronize (entrain) the physiologic desire for a sleep–wake schedule that is greater than 24 hours with a normal 24-hour day. Subsequently these patients continually “phase delay” and on a day-to-day basis show a progressive 1- to 2-hour delay of bedtime and final awakening times. When they attempt to keep regular sleep–wake schedules (fixed bedtime and final awakening times), they experience recurrent periods without sleep problems (when their intrinsic schedules match society’s), which are then followed by the gradual onset of periods associated with sleep-onset insomnia, difficulty waking in the morning, and daytime sleepiness (when their intrinsic schedules are out of synchrony with society’s). These patients are often blind and the disorder has been reported with intellectual disability, schizophrenia, and rarely in the otherwise normal population. Upon diagnosis, imaging studies of the brain can be considered, as this disorder has been associated with suprasellar lesions.
e. Shift work disorder. In this disorder insomnia and EDS result when the patient works during the normal physiologic sleep period. The prevalence of shift work in industrialized countries is 20% and the estimated prevalence of insomnia/EDS because of shift work is 2% to 5%. This disorder may complicate gastrointestinal and cardiovascular disorders, cause social difficulties, or lead to drug dependency in attempts to improve sleep, and presents work-related safety concerns.
f. Circadian sleep–wake disorder not otherwise specified. Degenerative diseases (including Parkinson’s and Alzheimer’s disease), blindness, and hepatic encephalopathy can alter the function of the biologic clock and lead to insomnia and EDS. Sleep-related problems can then influence the severity of the underlying condition (e.g., “sun downing” and nocturnal wandering in dementia).
E. Parasomnias. These are undesired sleep-related physical events, associated with semipurposeful behaviors and elevated autonomic activity. Of the parasomnias, only the REM sleep behavior disorder (RBD) requires PSG for diagnosis.
1. NREM-related parasomnias. Confusional arousals, sleepwalking, and sleep terrors are closely related parasomnias formally referred to as disorders of arousal (from NREM sleep). They can occur in a familial pattern, are primarily noted in children, and generally begin in slow-wave (stage N3) sleep during the first third of the night. The spells are associated with general lack of environmental responsiveness, automatic actions, confusion, disorientation, and occasional injuries. After these events, from which the patient is generally unarousable, there is usually amnesia without dream recall.
a. Confusional arousals. These are prevalent in children (17.3% in children 3 to 13 years of age) and adults <35 years of age (2.9% to 4.2% in adults >15 years of age), with a lifetime prevalence of 18.5%. The childhood form usually appears around 2 years of age and diminishes in occurrence after 5 years age. Young children may sleepwalk when they become adolescents. Adolescents and adults can have the variants: severe morning sleep inertia and sleep-related abnormal sexual behaviors. Severe morning sleep inertia is a persistent problem that can lead to sleep-related injury (risk of motor vehicle accidents), violent behavior, poor work performance, and social problems. Sleep-related abnormal sexual behaviors can lead to assaultive behaviors followed by morning amnesia.
b. Sleepwalking. This occurs with a lifetime prevalence up to 18.3% (peaking by 8 to 12 years of age), and in up to 4% of adults (with associated violent behaviors occurring more frequently in men). The rate of familial sleepwalking is 60% when both parents are affected. Childhood sleepwalking can lead to injury, but usually resolves by puberty.
c. Sleep terrors. These occur with a prevalence rate up to 6.5% in children, and in 2.2% of adults. Adults may have associated bipolar, depressive, or anxiety disorders. The onset is usually between 4 and 12 years with resolution often during puberty. During the spell, the patient often appears frightened, with tachycardia, tachypnea, diaphoresis, and inconsolable screaming and crying that can last from a few seconds to 20 minutes.
2. REM-related parasomnias.
a. RBD. This disorder is associated with violent behavior during sleep that reflects dream enactment. Events begin during REM (“dreaming” or “paralyzed”) sleep and are followed, after arousal, by reports of dream imagery compatible with the actions observed during the spell. This disorder generally appears after the age of 50 years, in elderly men, with a prevalence of 0.38% to 0.5% in the elderly and the general population. It is often associated with synucleinopathies (neurodegenerative disorders like PD and dementia with Lewy bodies (DLB), where there are neuronal lesions from aggregates of insoluble α-synuclein protein). A conversion rate (often after a delay of more than a decade) up 82% has been reported from idiopathic RBD to parkinsonism/dementia. RBD is reported in 46% of individuals with PD, 50% with DLB, and in >90% multiple system atrophy. The patients have histories of potentially harmful sleep-related body movements associated with dreaming. Patients frequently report sleep-related injuries, which include bruises, lacerations, dislocations, fractures, and subdural hemorrhage. The pathophysiology may be degeneration of REM-atonia pathways. The PSG shows that during REM sleep, muscle tone is generally elevated (REM without atonia). Periodic limb movements during sleep (PLMS) are seen in 75% of patients during NREM sleep. Behaviors appearing as dream enactment may be appreciated during REM sleep.
(1) Clinical or pathophysiologic subtypes. The parasomnia overlap disorder occurs when RBD occurs with a disorder of arousal, sleep-related eating disorder, sexsomnia, or rhythmic movement disorder (RMD). Status dissociatus is diagnosed when the PSG has no discernable sleep stages, but behaviors that resemble sleep and suggest dreaming and RBD. This can be seen in a broad range of underlying neurologic and medical conditions.
F. Sleep-related movement disorders
1. RLS. RLS is clinically diagnosed by symptoms that form the acronym URGE: an Urge to move the limbs (usually the legs), that is worse at Rest, improves with movement (Going), and is most evident in the Evening (often when attempting to go to sleep). In children there may be an association with ADHD. This symptom complex affects up to 10% of the general adult population, 30% of patients with rheumatoid arthritis, and up to 20% of patients with uremia (up to 62% of those on hemodialysis). It is reported almost twice as often in women, possibly related to the 11% to 20% prevalence recognized after the 20th week of pregnancy. There are early- and late-onset types of RLS. The early-onset form begins <45 years of age, is slowly progressive, and highly familial with 40% to 92% reporting affected family members. Linkage analyses have shown that a gene variant of BTBD9 is estimated to confer a population attributable risk of 50% for RLS. The late-onset form typically, rapidly progresses and aggravating factors are common. Etiologic elements may relate to physiologic mechanisms associated with relative central dopamine and iron deficiencies (serum ferritin <18 to 50 µg/L, iron saturation <16% to 20%).
2. Periodic limb movement disorder (PLMD). PLMS are reported in 80% to 90% of patients with RLS, in up to 34% of patients >60 years of age, and in up to 15% of insomniacs. When PLMS are significantly elevated and they have an adverse effect on sleep or daytime functioning, the diagnosis of PLMD is made. Gene variants BTBD9 and MEIS1 (found in genome-wide studies of RLS) appear to influence the expression of PLMS. PLMD can be exacerbated by tricyclic antidepressants, monoamine oxidase inhibitors, and hypnotics, and during withdrawal from benzodiazepines, barbiturates, and antiepileptic drugs. On PSG, the PLMS appear as elevated, predominantly 50 to 150 Hz, EMG activity from the tibialis anterior muscle, which persists for 0.5 to 5.0 seconds and coincides with episodes of repetitive, stereotypic extensions of the large toe with ankle, knee, and hip flexion. Consecutive movements have an intermovement interval ≥5 seconds and ≤90 seconds (generally 20 seconds to 40 seconds), and occur primarily in stage N2 sleep. PLMS are considered significant when the PLM index (the average number of PLMS per hour of sleep) is >5 in children and >15 in adults. New actigraphic monitors with high sampling rates can adequately detect PLMS, and promise to be a powerful research tool to study the known night-to-night variability of PLMS. There is controversy regarding whether autonomic arousals associated with PLMS (characterized by significant heart rate and blood pressure surges) provide a mechanism for possible increased risk for cardiovascular and cerebrovascular disease.
3. Sleep-related RMD. RMD primarily affects children. The movements are sleep related, stereotypical, repetitive movements of the head, neck, or large muscle groups and are often associated with rhythmic vocalization that includes head banging, body rocking, and leg banging (Video![]() 9.1). Rhythmic body movements often begin in normal children between 8 and 18 months of age and rarely lead to injury. These movements generally resolve by 5 years of age, although persistence may be associated with stress, stimulus deprivation, or CNS lesions. Family members are generally concerned about the noise and sometimes violent nature of these behaviors. PSG studies have shown that rhythmic movements tend to arise from stage N1 or N2 sleep and occur with a frequency of 0.5 to 2 Hz. A series of movements generally lasts <15 minutes.
9.1). Rhythmic body movements often begin in normal children between 8 and 18 months of age and rarely lead to injury. These movements generally resolve by 5 years of age, although persistence may be associated with stress, stimulus deprivation, or CNS lesions. Family members are generally concerned about the noise and sometimes violent nature of these behaviors. PSG studies have shown that rhythmic movements tend to arise from stage N1 or N2 sleep and occur with a frequency of 0.5 to 2 Hz. A series of movements generally lasts <15 minutes.
OTHER INVESTIGATIONAL TOOLS AND OPTIONS
A. The maintenance of wakefulness test (MWT). The MWT is a MSLT variant that is performed while the patient attempts to maintain wakefulness in an environment conducive to sleep (a warm, dark room, while lying in a semireclining position). The sleepiness documented utilizing an MWT may more accurately translate to a work situation when compared to the MSLT. The AASM Standards of Practice Committee recommends the MWT begin 2 hours after awakening from overnight sleep. It consists of four, 40-minute naps; each nap separated from the next by a 2-hour interval. A mean sleep latency <8 minutes is abnormal, whereas values between 8 and 40 minutes are of uncertain value. The use of an MWT has been approved in some occupations where sleepiness is hazardous, to justify a change in employment, and to support disability. No sleep is the strongest evidence for the ability to maintain wakefulness, but does not guarantee safety in regard to hypersomnolence.
B. Brain imaging and EEG. In some hypersomnias due to a medical condition, imaging of the brain and routine EEG may be of prognosticating value. In posttraumatic coma with hypersomnolence, radiographic evidence of hydrocephalus predicts poor treatment response. In Alzheimer’s disease, clinical progression, secondary to degeneration of cholinergic neurons in the basal forebrain, often correlates with EEG loss of sleep spindles, slow waves, and REM sleep patterns. The use of extended PSG montages, which have extra channels, can allow more thorough assessment of variables such as the EEG (for nocturnal seizures) and EMG (for sleep-related movement and behavior disorders). Daytime provocative studies can be used to appropriately characterize phenomena such as cataplexy.
C. Others. Routine laboratory studies may be needed to rule out anemia, hypoxemia, infection, and metabolic and endocrinologic abnormalities. A Minnesota Multiphasic Personality Inventory with an interview by a neuropsychologist or psychiatrist familiar with sleep disorders can be helpful in cases in which an affective disorder is suspected. There is promise that for a number of intrinsic sleep disorders, such as narcolepsy, genetic testing may help to confirm the diagnosis.
D. Referral to a sleep disorder center. When sleep problems persist, greatly impair quality of life, or necessitate formal sleep studies for diagnosis or therapy (SRBDs and narcolepsy), referral to a reputable sleep disorder center should be considered.
The general approach to the patient with a sleep disorder should always begin with the sleep history. The many specific questions necessary for diagnosing a variety of unique sleep disorders are neatly summarized in the ICSDs. The use of PSG is essential in diagnosing SRBDs, central disorders of hypersomnolence, and the RBD. The MSLT can delineate the types of pathologic sleepiness specific to narcolepsy and idiopathic hypersomnolence, whereas the MWT has been used to assess treatment efficacy and job suitability. In certain cases, basic metabolic panels, drug screens, genetic testing, and a variety of laboratory studies, including arterial blood gases (ABGs), complete blood counts, renal function tests, and CSF analyses, are of value. Occasionally, brain imaging, to address potential lesions affecting the ARAS and specific wake/sleep CNS centers, is important. An approach that properly combines clinical acumen with the appropriate diagnostic tools generally leads to a solid diagnosis, which allows successful therapeutic interventions.
Key Points
• It is imperative when approaching a patient with a suspected sleep disorder, to begin with a full sleep history for which the many specific questions necessary to diagnose any given disorder are clearly summarized in the ICSDs.
• The ICSDs define many sleep disorders, and only a few require PSG for diagnosis. These include the SRBDs and RBD (and in conjunction with an MSLT, the central disorders of hypersomnolence, as typified by narcolepsy types 1 and 2).
• In certain cases sleep diaries/actigraphy, properly timed urine drug screens, genetic testing, and CSF analyses (narcolepsy type 1), and waking ABGs and PaCO2 monitoring (sleep-related hypoventilation/hypoxemia) can be invaluable.
• An approach combing clinical acumen (based on a solid sleep history) and when indicated, diagnostic tools (which can include sleep diaries/actigraphy, PSG/MSLT, drug screens, ABGs, genetic testing, and CSF analyses) generally lead to solid diagnosis and successful treatment of many sleep disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







