Approach to the Selection of Electrodiagnostic, CSF, and Other Ancillary Testing
Paul W. Brazis
Maria Baldwin
Matthew A. McCoyd
Neurophysiologic electrodiagnostic studies define alterations in the functions of the nervous system that may not be visualized by imaging procedures. The major areas of study include EEG, nerve conduction studies (NCS), EMG, and evoked potentials. The clinical usefulness of these examinations is here discussed, followed by brief descriptions of other ancillary neurologic tests such as polysomnography and the multiple sleep latency test, and finally the indications, contraindications, and utility of performing lumbar puncture (LP) for CSF analysis.
I. ELECTROENCEPHALOGRAM
A. Introduction.
The EEG involves recording of the spontaneous electrical activity of the brain from the scalp and activity elicited by activation procedures, including sleep, hyperventilation, and photic stimulation. This electrical activity is the summation of both excitatory and inhibitory postsynaptic potentials from cortical neurons aligned perpendicular to the surface. Small metal disks containing conductive gel are attached to the scalp and ear lobes according to a system of measurements and are connected by flexible wires to a recording instrument that amplifies the brain activity about a million times. The EEG is sampled on moving paper or on a computer simultaneously from 16 to 21 pairs of electrodes (derivations) in selected combinations (montages).
B. Normal EEG activity.
1. EEG rhythms.
The EEG is a composite of several different types of activity, each with characteristic factors of frequency, amplitude, morphology, reactivity, topography, and quantity. The frequency bands of activity are as follows:
Delta activity (4 Hz)
Theta activity (4 to 8 Hz)
Alpha activity (8 to 13 Hz)
Beta activity (≥13 Hz)
2.
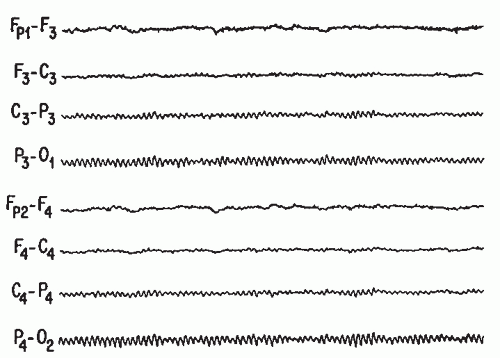
The most characteristic feature of a normal EEG in an adult during relaxed wakefulness is the alpha rhythm, which occurs over the posterior regions of the head while the eyes are closed (Fig. 33.1). Judgments of normality for various EEG activities depend on the age and state of alertness of the subject because complex changes in the EEG patterns occur throughout life and patterns evolve when going from wakefulness through different stages of sleep.
3. Activation procedures
are used to elicit abnormal activities that may not occur spontaneously.
Hyperventilation for 3 minutes is most effective for activating generalized seizure activities such as the spike-wave paroxysms of absence (petit mal) seizures. It may less frequently activate focal abnormalities (e.g., slowing) and focal epileptiform activity. It is contraindicated in a patient with cardiac infarction, recent subarachnoid hemor rhage (SAH), or significant pulmonary disease.
Photic stimulation consists of repetitive brief flashes of light generated by an elec tronic apparatus and delivered at frequencies of 1 to 30 Hz. This procedure evokes responses over the occipitoparietal regions (photic driving). The most frequent abnormal response is diffuse paroxysms of spike-wave complexes (photoparoxysmal or photoconvulsive response) that often indicate a seizure propensity.
C. Abnormal EEG activity.
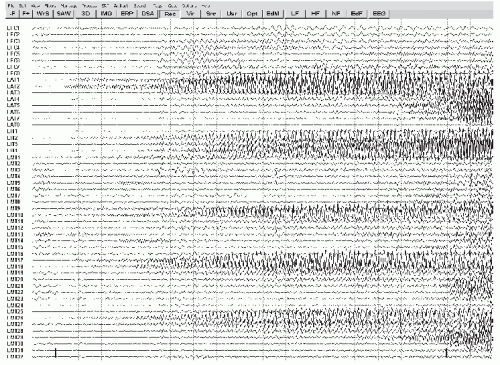
Many EEG changes are nonspecific, but some are highly suggestive of specific entities such as epilepsy, herpes encephalitis, and metabolic encephalopathies. In general, neuronal damage or dysfunction is suggested by the presence of slow waves (activity in the theta or delta range) in a focal or diffuse location, whereas the presence of sharp waves or spikes (epileptiform activity) in a focal or diffuse pattern suggests a seizure tendency. Localized slowing is highly sensitive and significant for local neuronal dysfunction or focal brain damage but is quite nonspecific because it cannot distinguish the pathologic type of lesion. Thus, cerebral infarction, tumor, abscess, and trauma may all cause similar focal EEG changes (Fig. 33.2). Diffuse slowing also indicates organic rather than psychiatric disease but again is nonspecific because such slowing may occur with any significant toxic, metabolic, degenerative, or even multifocal disease process. The EEG is also useful in following the courses of patients with altered states of consciousness and may, in certain circumstances, provide prognostic information. Finally, the EEG is important in the determination of brain death.
1. Epilepsy.
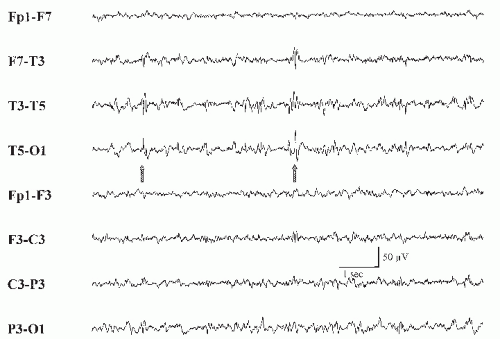
Some types of interictal EEG patterns are termed epileptiform because they have a distinct morphology and occur in a high proportion of EEGs from patients with seizures but rarely in records from asymptomatic patients. Such patterns include sporadic spikes, sharp waves, and spike and slow wave complexes. Not all spike patterns indicate epilepsy; 14- and 6-Hz positive spikes, sporadic sleep spikes, wicket spikes, 6-Hz spike-wave complexes, and the psychomotor variant pattern are all spike patterns that are of no proven clinical significance. Epileptiform discharges are not seizures in themselves. Seizures are electrographically defined as an evolution in frequency, location, or morphology of epileptiform discharges and usually last >10 seconds. An example of an electrographic seizure is demonstrated in Figure 33.3. Interictal findings must always be interpreted with caution because, although certain
patterns of abnormality may be evidence useful in supporting a diagnosis of epilepsy, even epileptiform discharges, with few exceptions, are poorly correlated with the frequency and likelihood of recurrence of epileptic seizures. One must always treat the patient and never “treat” the EEG.
A substantial portion of patients with unquestioned epilepsy have normal EEGs. However, epileptiform activity has a high correlation with clinical epilepsy. Only about 2% of nonepileptic patients exhibit epileptiform EEG activity, in contrast with 50% to 90% of patients with epilepsy, depending on the circumstances of recording and on whether more than one EEG has been obtained. The most conclusive proof of an epileptic basis for a patient’s episodic symptoms is obtained by recording an EEG seizure during a typical behavioral episode.
The EEG helps establish whether the seizure originates from a limited or focal area of the brain (focal or partial seizures) (Fig. 33.4) or involves the brain as a whole from the onset (generalized seizures). This distinction is important because of the different possible causes of these two basic epilepsy types and because the clinical manifestations of both types may be similar.
In general, the epileptiform activity on the EEG may be helpful in classifying the patient’s seizure type.
Generalized seizures of nonfocal origin usually are associated with bilaterally synchronous bursts of spikes and spike-wave discharges.
Consistently the focal epileptiform activity correlates with partial or focal epilepsy.
Anterior temporal spikes correlate with complex partial seizures.
Rolandic spikes correlate with simple motor or sensory seizures.
Occipital spikes correlate with primitive visual hallucinations or diminished visual function.
The EEG analysis may permit further discrimination of several relatively specific electroclinical syndromes.
Hypsarrhythmia refers to a high-voltage, arrhythmic EEG pattern with a chaotic admixture of continuous, multifocal spike-wave and sharp-wave discharges and widespread, high-voltage, arrhythmic slow waves.
This infantile EEG pattern usually occurs in association with infantile spasms, myoclonic jerks, and mental retardation (West’s syndrome) and usually indicates severe diffuse cerebral dysfunction. Infantile spasms consist of tonic flexion or extension of the neck, body, or extremities with the arms flung outward and typically last 3 to 10 seconds. The EEG and clinical findings do not correlate with a specific disease entity but reflect a severe cerebral insult occurring before 1 year of age.
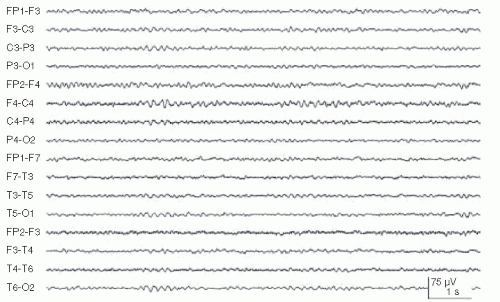
The 3-Hz spike-and-wave activity is associated with typical absence attacks (petit mal epilepsy) (Fig. 33.5). This pattern most often occurs in children between the ages of 3 and 15 years and is enhanced by hyperventilation and hypoglycemia. These bursts are typically accompanied by clinical signs such as staring, brief clonic movements, unresponsiveness, and motor arrest.
Generalized multiple spikes and waves (polyspike-wave pattern) are typically associated with myoclonic epilepsy or other generalized epilepsy syndromes (Fig. 33.6).
Generalized slow spike-and-wave patterns at a frequency of 1 to 2.5 Hz occur in children between the ages of 1 and 6 years who have some underlying diffuse cerebral dysfunction. Most of these children are mentally retarded and have poorly controlled seizures. The clinical triad of mental retardation, severe seizures, and the slow spike-and-wave pattern is called the Lennox-Gastaut’s syndrome.
(5) Central-midtemporal spikes occur in childhood and are associated with benign rolandic epilepsy. These seizures are often nocturnal and consist of focal clonic movements of the face or hand; tingling in the side of the mouth, tongue, cheek, or hand; motor speech arrest; and excessive salivation. The spells are easily controlled with anticonvulsants and disappear by 12 to 14 years of age.
(6) Periodic lateralized epileptiform discharges (PLEDs) are high-voltage, sharply contoured complexes that occur over one cerebral hemisphere with a particular periodicity. These complexes are not necessarily epileptic and usually correlate with acute destructive cerebral lesions, including infarction, rapidly growing tumors, and herpes simplex encephalitis (HSE) (Fig. 33.7). In the past, there was much debate if PLEDs constituted seizure activity. A consensus has now been reached in which PLEDs is not considered an ictal pattern, especially if the discharges occur at slower frequencies of 2 Hz or less.
Focal slowing (delta activity) in the interictal period usually indicates an underly ing structural lesion of the brain as the cause of the seizures. However, such focal slowing may be a transient aftermath of a partial seizure and may not indicate a gross structural lesion. Such slowing may correlate with a clinical transient postictal neurologic deficit (Todd’s phenomenon) and subsides within 3 days after the ictus.
The EEG can make a critical contribution to the diagnosis of a patient who is obtunded when prolonged subclinical seizures with only brief interruptions are recorded, signifying nonconvulsive status epilepticus
Ambulatory EEG monitoring is the recording of an EEG in a freely mobile patient outside of the EEG laboratory, similar to Holter’s monitoring for ECG recording. The main indication is to determine whether a spell is a seizure or some other phenomenon, especially in patients whose spells occur at unusual times or in association with specific events or activities. The yield depends on the type of patient selected, but the absence of EEG seizure activity during a spell does not fully exclude a seizure disorder, because surface electrodes may not record some mesial temporal, basal frontal, or deep midsagittal seizure discharges.
Patients with intractable focal seizures are sometimes candidates for surgical removal of the area of abnormality. Precise identification of the epileptogenic brain area requires special inpatient monitoring facilities for simultaneous closed-circuit television (CCTV) and EEG recording. Prolonged CCTV-EEG monitoring is also often used to document whether a patient’s clinical spells are epileptic or functional (psychogenic).
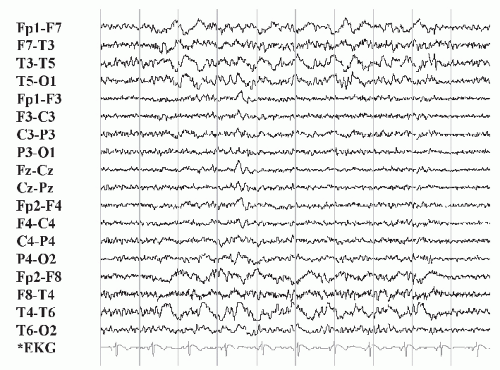 FIGURE 33.2 Left focal fronto-temporal slow wave abnormality in an adult patient with a recent large left fronto-temporal infarction. (Image courtesy of Dr. David Chabolla.) |
2. Altered states of consciousness.
For most causes of acute encephalopathy (e.g., toxic-metabolic disease), the EEG changes are nonspecific, consisting of diffuse slowing. There is, however, a generally good correlation between the degree of EEG abnormality and the clinical state.
An abnormal EEG confirms an organic rather than a psychogenic cause for a patient’s altered state of consciousness. It is also required to document unrecognized epileptic activity as a cause of depressed consciousness (nonconvulsive status epilepticus).
Certain EEG patterns increase the likelihood of specific metabolic disorders.
Prominent generalized fast (beta) activity in the EEG of a comatose or obtunded patient should raise the suspicion of drug intoxication most commonly seen with benzodiazepines.
Broad triphasic waves that are bilaterally symmetric and synchronous and have a frontal predominance may occur during an intermediate stage of hepatic encephalopathy (Fig. 33.8). However, such a pattern may also occur with other metabolic disorders.
Severe generalized voltage depression may suggest hypothyroidism if anoxia and hypothermia can be excluded.
Patients with uremia, uremic patients undergoing hemodialysis, and patients with hyponatremia may exhibit paroxysmal spike-wave discharges and a photoparoxysmal response to photic stimulation in addition to the diffuse slow-wave abnormality.
The focal epileptiform activity is commonly seen in hyperosmolar coma.
Cerebral hypoxia produces diffuse nonspecific slow-wave abnormalities that may be reversible. More severe hypoxia may cause EEG abnormalities that may be par oxysmal and associated with clinical myoclonus. An EEG obtained 6 hours or more after a hypoxic insult may demonstrate patterns of prognostic value in determining the likelihood of neurologic recovery. A poor neurologic outcome is suggested by the presence of the following abnormalities.
Alpha coma refers to the apparent paradoxical appearance of the monorhythmic alpha frequency activity in the EEG of a comatose patient (Fig. 33.9). However, in contrast to normal alpha activity, that observed in alpha coma is generalized, often most prominent frontally, and completely unreactive to external stimuli.
The burst-suppression pattern consists of occasional generalized bursts of medium- to high-voltage, mixed-frequency slow-wave activity, sometimes with intermixed spikes, with intervening periods of severe voltage depression or cerebral inactivity. The bursts may be accompanied by generalized myoclonic jerks.
The periodic pattern consists of generalized spikes or sharp waves that recur at a relatively fixed periodicity of 1 to 2 per second. The periodic pattern is usually accompanied by myoclonic jerks.
Electrocerebral silence. See I.C.3.a.
Infectious disease processes of the CNS produce predominantly diffuse and nonspecific slow-wave activity. However, certain EEG patterns assist in the diagno sis of specific infectious etiologies.
The EEG is extremely important in the initial assessment of HSE, often showing abnormalities before lesions detected by CT or MRI are recognized. A majority
of patients show temporal or frontotemporal slowing that may be unilateral or, if bilateral, asymmetric. Periodic sharp complexes over one or both frontotemporal regions add relative specificity to the EEG findings (Fig. 33.7). These diagnostic features usually appear between the 2nd and 15th days of illness and are sometimes detected only on serial tracings.
Subacute sclerosing panencephalitis (SSPE) has a distinctive EEG pattern of periodic bursts of stereotyped slow-wave and sharp-wave complexes occurring at intervals of 3 to 15 seconds.
Transmissible spongiform encephalopathy is associated with a relatively specific EEG pattern of diffuse high-voltage diphasic and triphasic sharp-wave complexes occurring at a periodicity of approximately 1 per second (Fig. 33.10). This periodic pattern is noted only in the end state of the disease process. Myoclonic jerks are also frequently seen and can correlate with the periodic discharges.
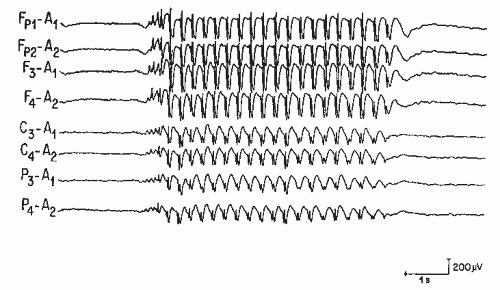 FIGURE 33.5 Burst of generalized 3 per second spike and wave discharges in a child with absence (petit mal) seizures. |
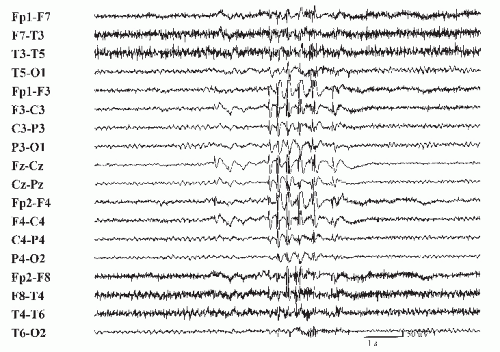 FIGURE 33.6 Burst of generalized multiple spike and wave discharges in a patient with generalized tonic-clonic seizures. |
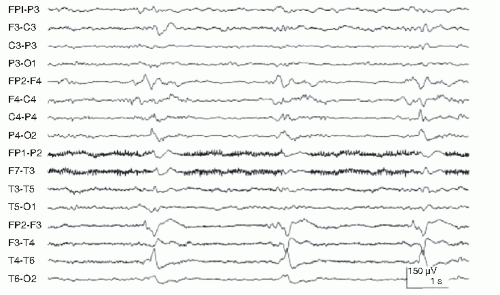 FIGURE 33.7 Right periodic lateralized epileptiform discharges (PLEDs) in a patient with HSE. Compare this figure with that of Figure 33.3 demonstrating a focal seizure. The PLED activity is monotonous and static with little spread and changes in frequency and morphology. In addition, frequency of PLEDs tend to be slower (<2 Hz). |
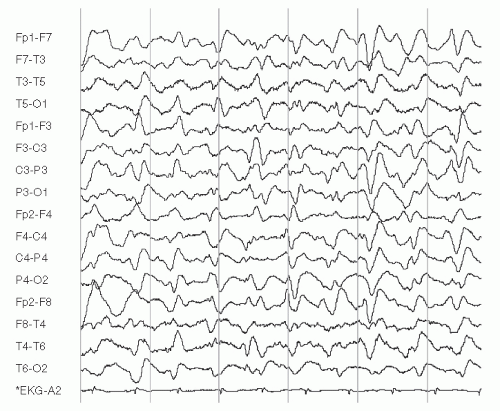 FIGURE 33.8 Frontal predominant triphasic waves and diffuse slow-wave abnormality in a patient with hepatic encephalopathy. (Image courtesy of Dr. David Chabolla.) |