34 Atypical Parkinsonian Syndromes
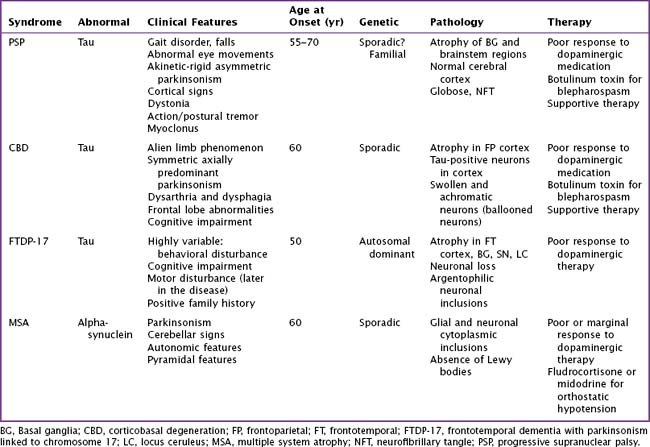
Atypical parkinsonian syndromes previously called Parkinson-plus syndromes, are chronic, progressive neurodegenerative disorders, characterized by rapidly evolving parkinsonism in association with other signs of neurologic dysfunction beyond the spectrum of idiopathic Parkinson disease (PD). These include early postural instability, supranuclear gaze palsy, early autonomic failure, and pyramidal, cerebellar, or cortical signs. The most common disorders (Table 34-1) are progressive supranuclear palsy (PSP), corticobasal degeneration (CBD), and multiple-system atrophy (MSA). Unlike idiopathic PD, these uncommon syndromes have poor or transient responses to dopaminergic therapy and consequently a worse prognosis. These disorders are classified as tauopathies and synucleinopathies based on the accumulation of the abnormal proteins tau or alpha-synuclein within neurons and glial cells having various anatomic distribution within certain brain areas.
Progressive Supranuclear Palsy
Clinical Vignette
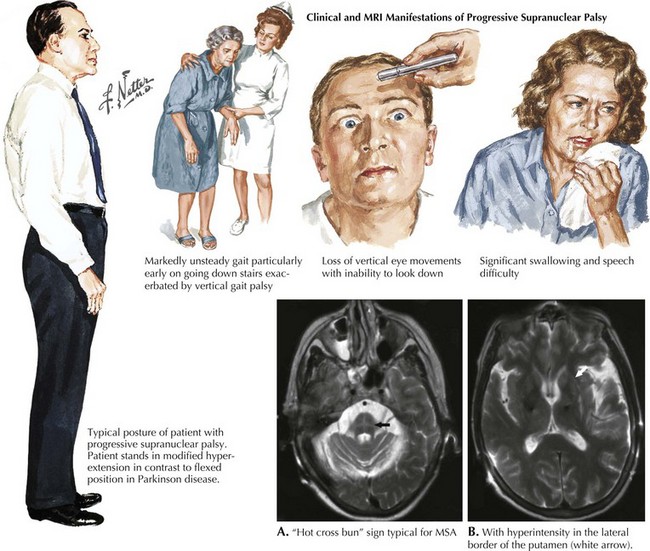
PSP is a sporadic tauopathy that has a progressive clinical course characterized by parkinsonism with supranuclear gaze palsy (Fig. 34-1), early postural instability, falls, bradykinesia, and dysarthria as well illustrated in this vignette. PSP typically does not respond to dopaminergic therapy. Its prognosis is poor, with a median survival of 5–7 years. PSP’s etiology, like that of CBD, is unknown. A genetic susceptibility may be invoked; however, to date, only the H1 MAPT haplotype has been consistently associated with a risk of developing progressive supranuclear palsy
Pathophysiology
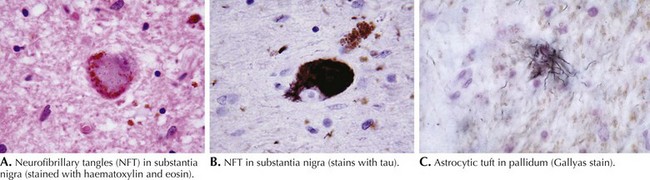
PSP is primarily a subcortical neurodegenerative tauopathy in contrast to both CBD and FTPD-17 having involvement of the cerebral cortex. Macroscopically, depigmentation is observable within the substantia nigra (SN) and locus coeruleus (LC), as well as atrophy of the pons, midbrain, and globus pallidum (Fig. 34-2). Microscopically, the most affected regions are brainstem nuclei III, IV, IX, and X, the red nucleus, LC, SN, globus pallidus, and cerebellar dentate nucleus. Tau protein accumulates within neurons as neurofibrillary tangle (NFT) and in glia as spherical neuropil threads.
Clinical Presentation
Patients usually present with gait instability and tendency to unexpectedly fall backwards; in contrast, neither of these symptoms occurs early on in Parkinson disease. The parkinsonism of PSP is typically axial and symmetric, unlike the asymmetric often single limb presentation of PD. Most patients with PSP carry an erect posture in contrast to the flexed PD stance (see Fig. 34-1). Often they lack the typical PD tremor. Dystonia is a common finding particularly early on affecting limbs, neck dystonia, or even as blepharospasm.
Diagnosis
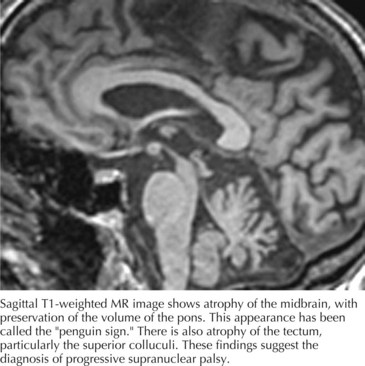
Computed tomography (CT) and magnetic resonance imaging (MRI) (Fig. 34-3) often demonstrate generalized or brainstem (dorsal midbrain) atrophy. The combination of atrophy of the midbrain tegmentum with relative sparing of the basis pontis resembles “a lateral view of a standing penguin (especially, the king penguin), with a small head and big body” on a midsagittal MRI scan. Previously, appearance of the midbrain tegmentum was stated to resemble the head of a hummingbird. Whether the penguin or hummingbird sign will take flight remains to be seen, but the implication of both studies is the same: the midbrain in PSP is atrophic and MRI can be helpful to verify the clinical diagnosis.