62 Lumbar Radiculopathy
Clinical Presentation
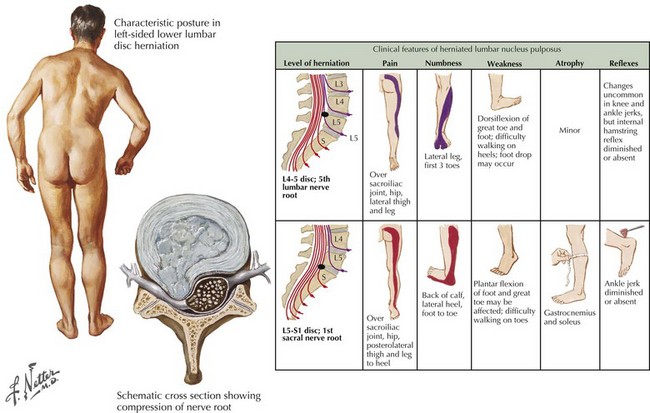
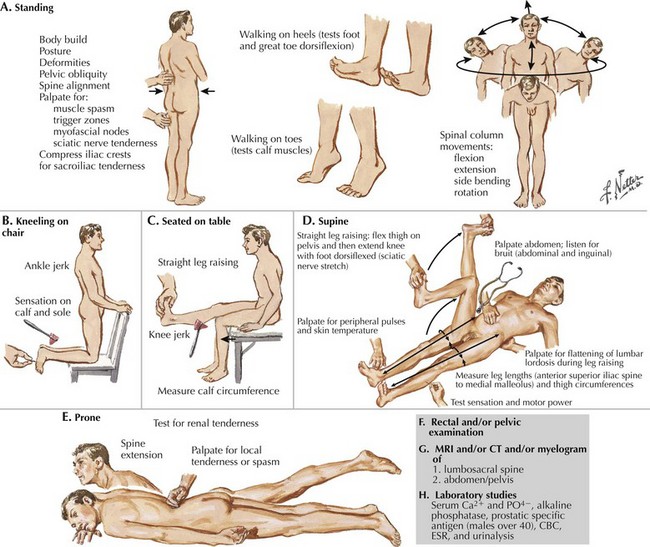
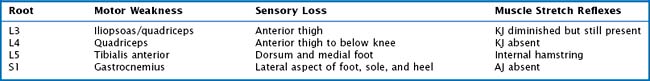
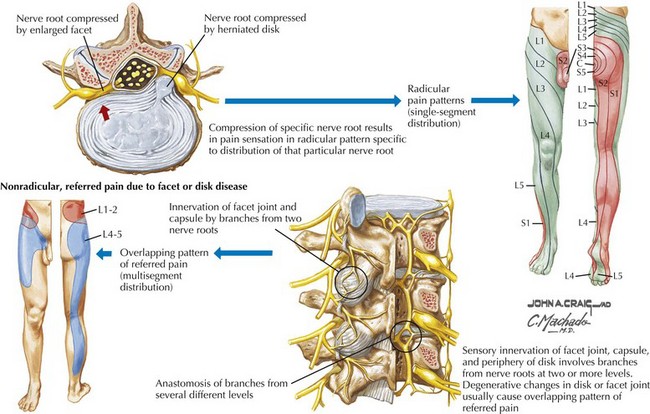
Sciatic pain may occur acutely or evolve more gradually; when the onset is sudden, it may be spontaneous or related to a specific incident, sometimes a seemingly trivial event, such as bending over to make a bed. The symptoms may be minor and clinically inconsequential or significant requiring urgent evaluation and treatment (Fig. 62-1). Depending on the specific nerve root involved, the pain may be classic sciatica with radiation down the posterior aspect of the leg into the foot, as is seen with compression of the L5 or S1 roots (Figs. 62-2 and 62-3). At higher levels, with L3 or L4 root compression, the pain may radiate to the anterior thigh. The clinical signs of lumbar radiculopathy are due to the specific level of involvement (Table 62-1), and the most common levels of nerve root irritation are L5 and S1 roots, followed less commonly by L4 and L3 roots. It is rare to have involvement of the higher roots (L1 and L2).
Etiology
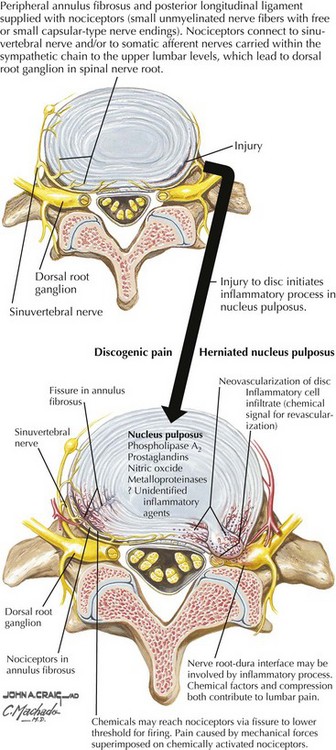
The most frequent cause of lumbar radiculopathy is a herniated lumbar disc, due to herniation of the nucleus pulposus, usually occurring with an equal frequency at the lowest two levels, L4–5 and L5–S1 (Figs. 62-4 and 62-5; see Fig. 62-1). Only ~5% of lumbar disc herniations occur at higher levels. Herniation is the last manifestation of disc degeneration that is an ongoing process in all humans. Hence, disc herniation is uncommon in youth, although occasionally teenagers and rarely toddlers have symptomatic herniations. Disc herniation occasionally occurs with spinal stenosis and may be the cause of rapid deterioration. Most lumbar radiculopathies are unilateral; bilateral sciatica has an ominous significance, suggesting compression of the cauda equina; these patients are at risk for loss of sphincter functions as well as sexual function in males. Early recognition is essential, as even after expeditious decompression, sphincter control and potency may not always return. Rarely spondylosis with foraminal encroachment resulting from disc degeneration may cause radiculopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree