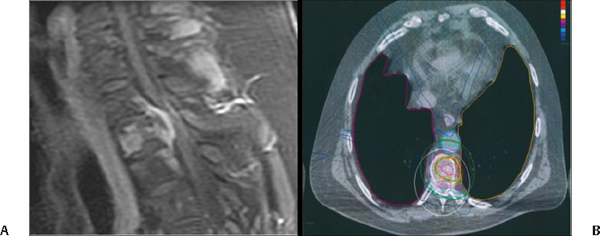
38 What is stereotactic radiosurgery (SRS)? Single-session (or hypofractionated, i.e., two to five sessions), focused beam radiation delivery used to treat brain or spine abnormalities1 When was SRS first developed? In 1951 by the Swedish neurosurgeon Lars Leksell as an alternative to the highly invasive surgical procedures of the era for movement and pain disorders1 What is a localizer? A small device attached to the frame (that is attached to a fixed point on the patient) that has neuroimaging-compatible fiducial markers in the major cardinal planes. What does the localizer achieve? It links the stereotactic coordinate with the imaging coordinates. What is a positioner? A small device attached to the frame that aligns the stereotactic and room coordinate systems. What is a dose gradient? The change in radiation dose as a function of distance. It is also called “radiation fall-off.” What are multileaf collimators? A collimator is a device made up of “leaves” of a high atomic numbered material that can be positioned along the path of a particle beam to block it. Multileaf collimators allow computer-assisted or manual beam shaping for contouring the radiation field to the tumor shape.2 What are microleaf collimators? Microleaf collimators are multileaf collimators that can achieve decreased leaf width for lower beam width. What do computer-controlled microleaf collimators achieve? Dynamic field adjustment during irradiation, which allows for intensity-modulated radiotherapy (IMRT)3 What are FSR and SRT? Fractionated stereotactic radiotherapy and stereotactic radiotherapy, which describe fractionated therapy Which patients are candidates for SRS? • Patients with skull base tumors (e.g., acoustic neuroma, pituitary adenoma, meningioma) • Patients with limited numbers of brain metastasis • Patients with compact arteriovenous malformations • Patients with medically refractory trigeminal neuralgia • Those with focal, recurrent, or residual lesions • Patients with a favorable performance status (e.g., KPS) • Certain patients with spinal cord or spinal column tumors (either primary or metastatic) not amenable to surgical resection or that have recurred or present as a residual after surgical resection (primarily treated with robotic radiosurgery) What is the optimal target for SRS? Solid, well-defined tumors ≤3 cm What are other applications for SRS? Movement disorders (seldom done except for essential tremor) and well-defined focal pain syndromes (e.g., trigeminal neuralgia) Is SRS primary or adjuvant therapy? It’s considered primary therapy for unresectable tumors or AVMs, but it serves as adjunctive therapy in the treatment of resectable tumors. How does radiosurgery exert its effects? 1. Direct cytotoxic damage (malignant tumor model) 2. Indirect vascular effects (benign tumor model) 3. Neuromodulation How do the mechanisms of brachytherapy and radiosurgery differ? Brachytherapy exploits cell susceptibility in the cell cycle over time, whereas radiosurgery arrests cell-division at all points in mitosis. How is brachytherapy delivered? “Seeds” of highly active iodine-125 are implanted stereotaxically, allowing for delivery of a focal radiation dose over 4 to 6 days.4 How do SRS and stereotactic radiotherapy (SRT) differ? According to the AANS/CNS Stereotactic Radiosurgery Task Force, the two techniques are part of a continuum, but broadly speaking, SRS is delivered in one to five sessions, whereas SRT, which is typically fractionated, may occur over as many as 30 sessions.1 What is fractionated stereotactic radiotherapy? Multiple treatments given daily or multiple times per day, over weeks (concept: healthy tissue regenerated between minor dose overlap) What is the goal of fractionation? To allow for the 4 R’s of radiation therapy: reoxygenation, reassortment, repopulation, and repair1 What is the primary accepted mechanism of radiotherapy? Free radicals causing single- and double-stranded DNA breaks of tumor cell DNA How long does it take for SRS to be effective? 1. Weeks to months for malignant or metastatic tumors (i.e., early-responding tissue) 2. One year or more for benign tumors or AVMs (i.e., late-responding tissue)5 What is the most common side effect of SRS? Cerebral edema (may be treated with steroids) Can SRS be used on a patient who has already had other radiotherapy? Yes6 What is the probability of developing a SRS-induced tumor? Although one series argues less than 1 in 1000,7 the landmark study by Rowe et al have found no significant increase in neoplasm after treatment, with the important caveat that mean follow-up was only 6.1 years.8 Several cases of SRS-induced neoplasms have been reported in the literature,9–11 but it is considered customary to tell patients that the odds are between 1 in 1000 to 20,000.12 What are the three basic forms of SRS? Proton, photon, and linear accelerator (LINAC) What is proton SRS? Particle beam radiation used for treatment of brain tumors What is Gamma Knife™ SRS? Gamma Knife was originally developed by Leksell and colleagues in 1967. • Gamma Knife™ SRS (GKS) (Elekta™ AB) is a photon-based device that contains 201 fixed cobalt-60 sources. • Cobalt-60 emits gamma ray photons that travel as high-energy beams and are delivered at a predetermined rate. • GKS enables precise delivery of radiation to a target by delivering 201 separate beams of radiation, which converge onto a predetermined central target. What is LINAC? LINAC is an acronym for “linear accelerator.” LINAC produces ionizing beams (photons) used in single session or multisession therapies. These can be used on brain and body tumors or other lesions such as AVMs. There are multiple brands of LINAC systems. What is CyberKnife™ (Accuray)? • CyberKnife™ is a brand of LINAC equipped with stereotactic capability. • It is essentially a frameless robotic radiosurgery system with two main elements: • A small linear particle accelerator that produces the radiation • A robotic arm that enables the energy to be directed at any part of the body from any direction Fig. 38.1 (A) Midsagittal T1 MRI with contrast of the thoracic spine demonstrating a lesion at the T3 vertebral body level consistent with a vertebral body and epidural metastasis in a 60-year-old patient with lung carcinoma. (B) Cyberknife™ planning axial CT showing target lesion of interest highlighted in red as well as critical anatomy also delineated including the spinal cord, aorta, and lungs. The colored lines surrounding the target represented the isodose lines of the treatment.
Basic Concepts
38.1 Important Terminology and Concepts
38.2 Patient Selection
38.3 Radiation Delivery Options (Whole Brain, Fractionated Radiosurgery, Stereotactic Radiosurgery)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






