♦ Preoperative
Operative Planning
- Diagnostic imaging
- Computed tomography (CT) scan
- Hydrocephalus should be evaluated, and ventriculostomy performed if ventricles are enlarged
- Calcium or atherosclerotic changes in the aneurysm wall might preclude microsurgical clipping
- Brain asymmetry (temporal lobe encephalomalacia, prior surgery, or sylvian anatomy) might affect side of surgical approach
- Relationship of aneurysm neck relative to the posterior clinoid processes, dorsum sella, and clivus
- Size of frontal sinuses
- Intraluminal thrombus, which might be more apparent on CT angiography
- Hydrocephalus should be evaluated, and ventriculostomy performed if ventricles are enlarged
- Angiogram
- Aneurysm size, neck size, and morphology
- Aneurysm projection (anterior, posterior, superior, or lateral)
- Location of aneurysm neck relative to the posterior clinoid processes, dorsum sella, and clivus
- Laterality
- Anatomy of branches at the aneurysm neck (P1 PCAs, SCAs, and perforators)
- Discrepancy between intraluminal size on angiogram and extraluminal size on CT or magnetic resonance imaging (MRI) suggests intraluminal thrombus
- Posterior communicating (PCOM) artery and P1 PCA are examined for fetal anatomy and anterior to posterior collateral circulation
- Other aneurysms might influence side of surgical approach
- Perforators
- Other angiographic abnormalities, such as early vasospasm, arterial occlusions, associated arteriovenous malformations, moyamoya disease, etc.
- Anatomy of branches at the aneurysm neck (P1 PCAs, SCAs, and perforators)
- Aneurysm size, neck size, and morphology
- MRI
- Not usually done
- Demonstrates intraluminal thrombus and compressive/mass effect
- Not usually done
- Computed tomography (CT) scan
Special Equipment
- Radiolucent head holder, if an intraoperative angiogram will be needed
- Reciprocating saw for orbitozygomatic osteotomies
- Diamond burr (1-mm or 2-mm diameter ball tip) or ultrasonic aspirator with bone curettage tip for removal of posterior clinoid process with low-lying basilar apex aneurysms
- Aneurysm clips, permanent and temporary
- Rhoton dissectors
- Doppler flow probe
- Intraoperative angiography, either with conventional catheter angiography or indocyanine green dye
Operating Room Set-up
- Operating microscope (foot pedal for focus and zoom, mouthpiece for fine adjustments)
- Chair, with arm rests and floor wheels
- Neurophysiological monitoring with somatosensory evoked potentials, motor evoked potentials, and electroencephalography
Anesthetic Issues
- 1 g ceftriaxone, 10 mg dexamethasone, and 1 gm/kg mannitol on skin incision
- Maintain cranial perfusion pressure > 70 mm Hg to prevent ischemia from brain retraction, temporary blood vessel occlusion, or vasospasm
- Severe hypertension should be treated aggressively (propofol, thiopental, vasoactive drugs)
- Allow temperature to drift toward 34° C, start warming after aneurysm clipping
- Relative hypervolemia and above normal blood pressure after aneurysm clipping in patients with vasospasm
♦ Intraoperative
Orbitozygomatic Craniotomy
- As described in Chapter 6, Orbitozygomatic Approach
- A wide splitting of the sylvian fissure is essential, exposing the middle cerebral artery (MCA) trifurcation, M1 segment, and distal M2 MCA branches
- Frontal, self retaining (Greenberg) retractor placed on the frontal lobe at junction of olfactory and optic nerves
- The carotid cisterns are opened to drain cerebrospinal fluid (CSF), and the A1 anterior cerebral is followed out the lamina terminalis for fenestration and additional CSF drainage
- Mobilize the temporal lobe by coagulating and cutting arachnoid adhesions between inferior temporal lobe and middle fossa dura, then coagulating and cutting the temporal pole vein bridging to the sphenoparietal sinus
- Open the arachnoid planes along the tentorial edge, freeing the oculomotor nerve from its connections to the temporal lobe
- Identify PCOM artery and anterior choroidal artery (AChA). PCOM leads to the membrane of Liliequist, which is carefully opened to enter the posterior fossa. AChA leads to the choroidal fissure, and careful dissection of this artery separates the deep adhesions between frontal and temporal lobes to maximize temporal lobe mobilization
- Temporal lobe is then retracted posteriorly and laterally, with the retractor tip placed on the uncus
- In patients with subarachnoid hemorrhage, clot obscures the vascular anatomy and should be removed carefully along normal anatomy as it is uncovered. The PCOM artery serves as the guiding landmark into thick clot, leading the dissection to the P1–P2 PCA junction and preventing inadvertent encounters with the aneurysm dome
- PCOM artery and its perforators can be swept superiorly to open the surgical corridor to more medial structures. Occasionally, PCOM artery may require sacrifice to widen the exposure, but this maneuver should be performed only when PCOM artery is small and the ipsilateral P1 PCA can be preserved with microsurgical clipping. PCOM artery should not be sacrificed when there is fetal anatomy or when clipping might compromise flow in the P1 PCA.
- The undersurface of P1 PCA is followed medially to its intersection with the basilar artery, where SCA is also identified
- Aneurysm dissection is avoided until a segment of the basilar artery is secured below the SCA for proximal control
- Identify the four vessels arising from the apex and decrease the patient’s head rotation as needed to bring the basilar trunk and contralateral vessels into view (Fig. 26.1)
- Identify and exclude posterior P1 perforators by dissecting along back wall of basilar artery proximal to ipsilateral P1 toward base of contralateral P1
- For low-riding lesions, the posterior clinoid and upper portion of the clivus can be drilled off with a diamond burr or ultrasonic aspirator equipped with a bone curettage tip. Bleeding from the posterior-medial cavernous sinus is controlled with bone wax or Nu-knit (Ethicon).
Temporary Clipping
- Temporary clipping should be considered when the aneurysm appears fragile or thin-walled, and mobilization is required to visualize relevant anatomy. Temporary clipping softens the aneurysm to facilitate its manipulation, and reduces the risk of intraoperative rupture.
- An area below the SCAs relatively free of circumflex perforators is identified for temporary clipping
< div class='tao-gold-member'>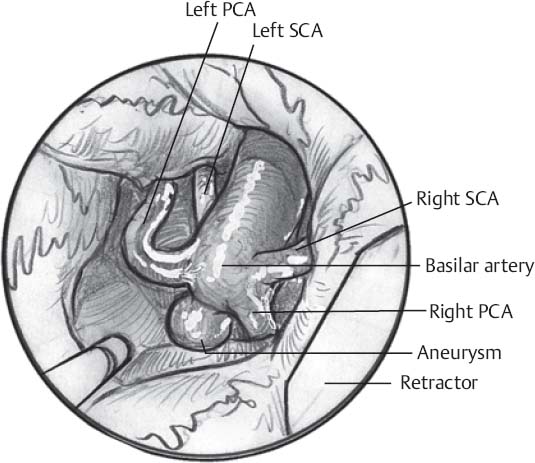 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue








