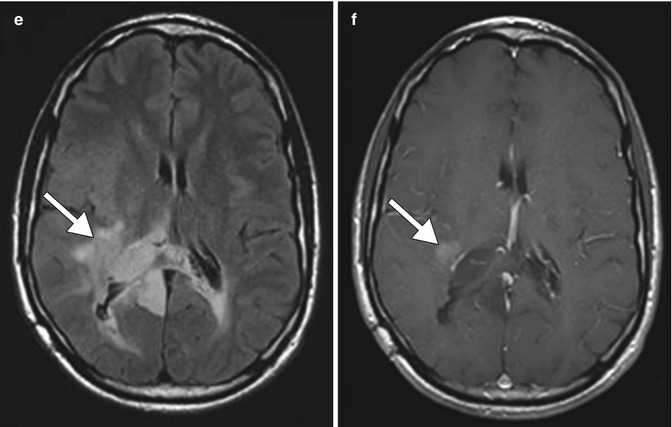
Fig. 16.1
Pseudoresponse. The patient has a history of recurrent glioblastoma in the splenium of the corpus callosum, treated with bevacizumab. Axial FLAIR (a) and T1-weighted post-contrast (b) MR images show a heterogeneous enhancing mass involving the splenium of the corpus callosum. Axial FLAIR (c) and T1-weighted post-contrast (d) MR images show marked interval decrease in the degree of enhancement and edema associated with the tumor shortly after bevacizumab administration. Axial FLAIR (e) and T1-weighted post-contrast (f) MR images show a new area of enhancement and T2 hyperintensity on follow-up imaging obtained 2 months later (arrows)
Stroke-like lesions with diffusion restriction can also result from bevacizumab administration to glioblastoma and metastases (Figs. 16.2 and 16.3). In addition, there is commensurate suppression of abnormal enhancement and normalization of perfusion in the areas of restricted diffusion. These lesions can manifest as early as 4 weeks after initiation of therapy and can persist for at least up to 80 weeks. The histopathology of such lesions consists of atypical necrosis and nuclear hypoxia-inducible factor 1-alpha upregulation, but no tumor recurrence. The cause of these alterations is still uncertain, but may entail atypical necrosis and chronic hypoxia. Other possible neuroimaging findings related to bevacizumab administration include nasal septal perforation and posterior reversible encephalopathy syndrome (Fig. 16.4). Although tumor hemorrhage has been reported with bevacizumab use, bevacizumab may not necessarily carry an increased risk for this complication since many tumors have a propensity to hemorrhage spontaneously.
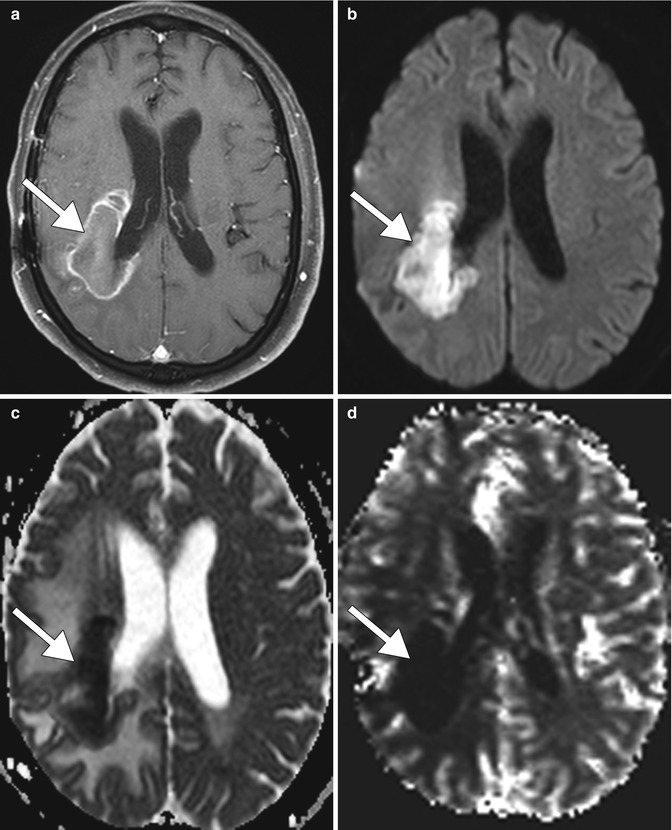
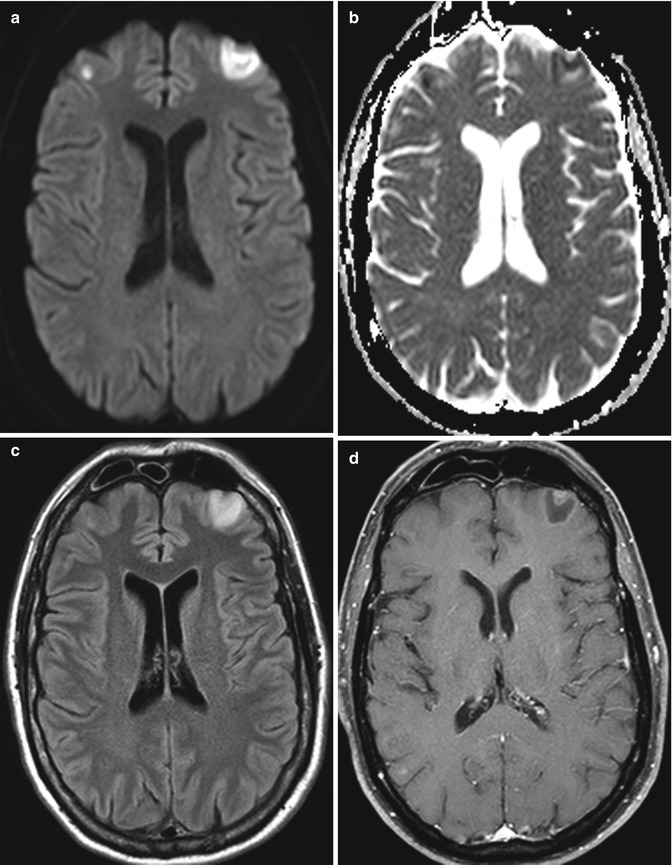
Fig. 16.2
Bevacizumab-induced stroke-like lesions in glioblastoma. The patient has a history of recurrent right frontoparietal glioblastoma treated with bevacizumab monotherapy. Axial post-contrast T1 (a), DWI (b), ADC map (c), and CBV map (d) images show hyperintense DWI signal within the previously contrast-enhancing tumor area and corresponding ADC reduction and hypoperfusion (arrows)
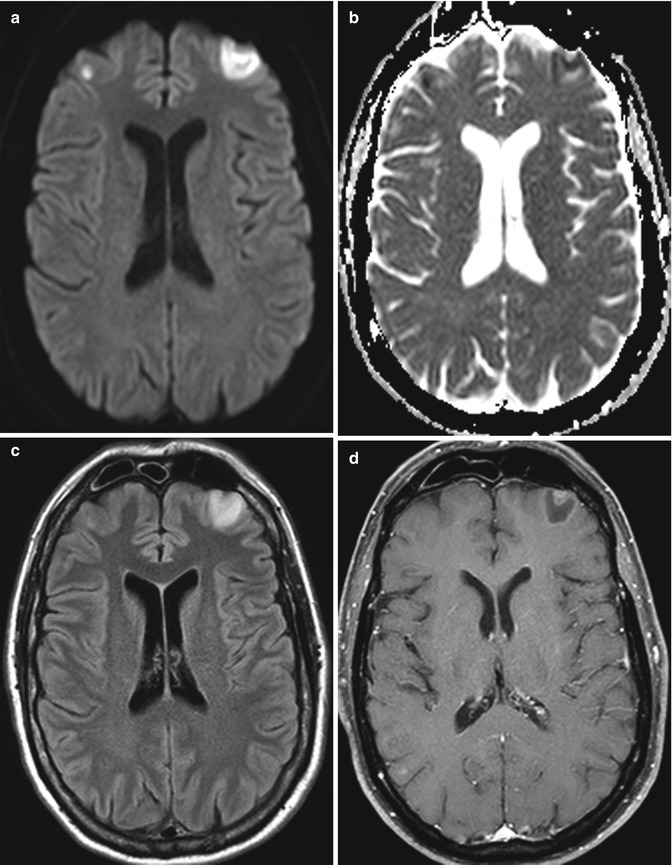
Fig. 16.3




Bevacizumab-induced stroke-like lesions in renal cell carcinoma metastases. Axial DWI (a), ADC map (b), FLAIR (c), and post-contrast T1 (d) show restricted diffusion in the bilateral frontal lobe metastases with negligible associated enhancement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








