Chapter 159 Biomechanics of Motion Preservation Techniques
For many years, cervical and lumbar arthrodesis has been the gold standard of treatment for a wide range of degenerative, traumatic, deformational, and oncologic spinal disorders. Although spinal arthrodesis has been used with great success, from a biomechanical perspective, it significantly alters the regional and global balance of physical forces and moments. As a consequence, several studies have demonstrated accelerated degenerative changes at levels directly adjacent to rigid spinal fusions.1–3 This is commonly termed adjacent-segment degeneration (ASD). Specifically, it is thought that the stiffness imposed by a rigid fusion on an adjacent vertebral functional spinal unit (FSU) alters stress transfer between the vertebral segments and predisposes adjacent segments to accelerated degeneration. As a result of this, motion-sparing technologies have emerged in an attempt to preserve the native motion of the spinal unit, predominantly at the disc interspace. Theoretically, if a motion-sparing implant closely simulates the biomechanical properties of the intact FSU, the incidence of ASD would be expected to decrease.
The earliest and most traditional form of motion preservation surgery came in the form of laminectomy, laminoplasty, and laminoforaminotomy. These techniques were designed to treat underlying spinal pathology while preserving as much of the natural motion of the spine as possible. They involve a small amount of bone removal and preservation of the facets and many of the supporting ligaments, and do not violate the disc. In particular, the laminoforaminotomy has been shown to induce the least disruption in normal spinal mobility and stiffness compared with traditional laminectomy.4 There is, however, a limited range of pathologic processes for which these techniques are indicated (and effective).
Biomechanics of the Functional Spinal Unit
Physical Principles
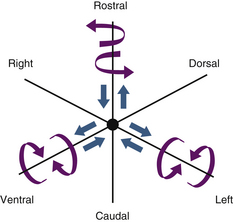
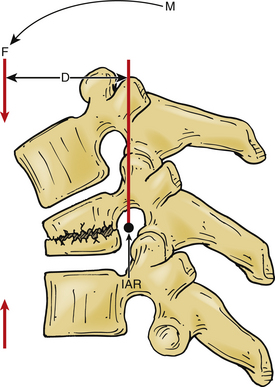
A vector is a force oriented in a fixed direction in three-dimensional space. All forces acting on the spine can be described in terms of their component vectors. A vector may act on a lever (moment arm), resulting in a bending moment. A bending moment applied to a point in space causes rotation (or a tendency to rotate) about an axis, called the instantaneous axis of rotation (IAR). Movement about the IAR can be described in terms of the cartesian coordinate system (Fig. 159-1). The IAR is the point or location in three-dimensional space about which each vertebral segment rotates at any given instant. The location of the IAR is not fixed, but rather is variable (mobile) depending on the intrinsic curvature of the spine and any other intrinsic or extrinsic forces that may act on the spine5 (Fig. 159-2).
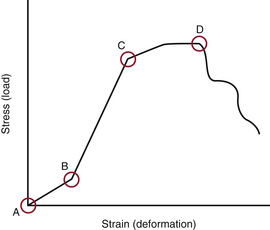
When several forces act on a solid with a resultant net force of zero, the solid is deformed. A stress-strain curve describes this relationship (Fig. 159-3). Stress is defined as the force applied to an object (load). Strain is defined as the response of the object to the force (deformation). The neutral zone or zone of nonengagement describes the reaction of a solid to stress before deformation of that solid is realized. When the neutral zone is exceeded and stress continues, the solid enters into the elastic zone. The elastic zone describes applied stress (usually of lower magnitude) that results in strain that is completely recoverable after removal of stress. As the applied force increases, the elastic limit is reached and the plastic zone is entered. At this point, increased stress results in permanent deformation of the solid up to the point of failure, when the solid yields.
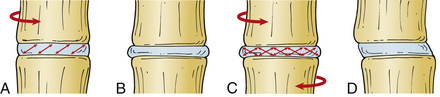
Intervertebral Disc
The intervertebral discs contain a peripherally located anulus fibrosus and a centrally located nucleus pulposus. The cartilaginous end plates form the rostral and caudal limits of the intervertebral discs. The fibers of the anulus are arranged radially in opposite directions about the vertebral body interspace between the end plates, whereas the nucleus pulposus is contained within the anulus. The anulus contains two types of laminated (mostly collagenous) fibers: radial fibers that attach to the cartilaginous end plates (called inner fibers) and to the cortical bone on the edge of the vertebral bodies (called Sharpey fibers). These fibers are oriented roughly 30 degrees with respect to the end plate and opposite to each other, which gives the disc the ability to resist rotational forces (Fig. 159-4). The nucleus pulposus is a gel-like remnant of the embryonal notochord. It is composed of reticular bands surrounded by a thick mucoid ground substance.
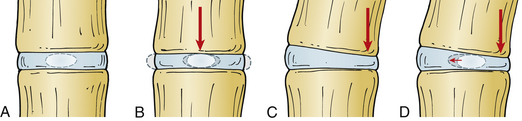
The intervertebral disc can resist significant axial forces; however, this ability decreases with age. A pure (i.e., central) axial load causes symmetrical deformation of the disc because the intradiscal pressures are distributed symmetrically. In the presence of flexion, extension, or lateral bending (i.e., eccentric) forces, the intradiscal pressures are distributed asymmetrically and the normal disc will deform in a relatively predictable manner. The anulus bulges on the side of the deformation and stretches on the side opposite to the load, whereas the nucleus pulposus tends to move away from the area of applied force (in the opposite direction from the anular bulge)5 (Fig. 159-5).
Studies of the nucleus pulposus in vitro demonstrate its importance in intervertebral disc biomechanics. Mechanical denucleation of intervertebral discs in cadaver lumbar spine segments results in increased range of motion and neutral zone compared with intact discs. Removal of the nucleus also results in decreased disc height and segment stiffness. Interestingly, the nucleus is most effective at lower loads, before the anulus has a chance to be engaged in a more effective tensile load-bearing state.6
Biomechanics of Intervertebral Disc Degeneration
Several in vitro and finite element analysis (FEA) studies have been conducted to examine the complex forces at play in the FSU and on the intervertebral disc. A complex state of loading exists in the physiologic scenario, and studies must strive to duplicate this. For example, the intervertebral disc rarely undergoes isolated axial loading but rather experiences a dynamic range of forces, usually in combination and varying from moment to moment. Many FEA studies have therefore measured a variety of combinations of forces applied to a given intervertebral disc and measured resultant intradiscal pressures and shear strains on the discs.
An FEA study of the L4-5 FSU demonstrated that the anulus fibrosus is strained maximally in the dorsolateral regions of the intervertebral disc.7 This may explain why a disc prolapse occurs most commonly in this region. The shear and fiber strains on the anulus were greatest during combined movements such as rotation plus lateral bending or flexion and combined flexion or extension and lateral bending. These strains were also high in the dorsolateral regions of the disc. An in vitro study of human lumbar spine segments also supports these data.8
As the disc degenerates, a cascade of events ensues that eventually may result in symptomatic degenerative disc disease. In the early stages of disc degeneration, the disc gradually desiccates, losing water content and height in the process. Intradiscal pressures elevate as a result of this because the disc is no longer able to efficiently resist the forces placed on it. The disc interspace narrows, resulting in distortion and bulging of the anulus. The fibers of the anulus gradually break free of their bony attachments, and osteophytes form at these points because of subperiosteal bone formation. The patient may begin to experience pain of spinal origin. At this point, the FSU may become a dysfunctional motion segment, and its motion mechanically unstable. A dysfunctional motion segment is defined as a type of instability related to disc interspace or vertebral body abnormality that results in the potential for pain of spinal origin.5 The patient may experience deep, agonizing back pain that worsens with activity and is relieved by rest; this symptom suggests the diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree