Fig. 51.1
Bisphosphonate-induced osteonecrosis of the mandible. Axial (a) and coronal (b) CT images show a mixed sclerotic and lucent lesion within the left mandibular body that has a bone-within-a-bone appearance (arrows)
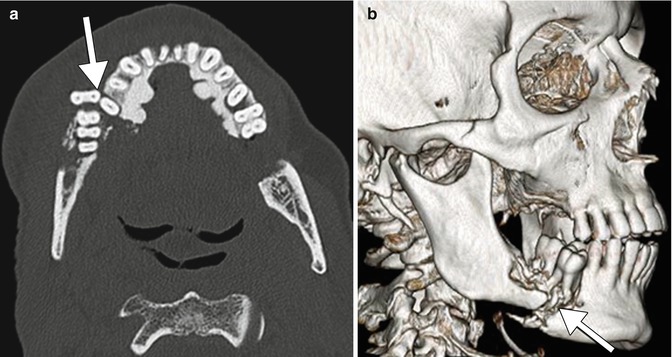
Fig. 51.2
Bisphosphonate-induced osteonecrosis of the mandible with pathological fracture. Axial (a) and 3D surface rendered (b) CT images show a displaced fracture of the right mandibular body (arrows), adjacent to a lucent focus of osteonecrosis. There is also torus mandibularis internis (Courtesy of Christine Glastonbury)
Fig. 51.3
Bisphosphonate-induced osteonecrosis of the maxilla. Coronal CT image shows a defect in the left maxillary sinus wall and alveolus with associated oroantral fistula (arrow) (Courtesy of Christine Glastonbury)
MRI can be used to further delineate involvement of the surrounding soft tissues and neurovascular bundle, lymphadenopathy, as well as bone marrow edema, which may be an early indicator of bone ischemia and necrosis. Therefore, in the early stages of BRONJ, findings classically include decreased bone marrow signal intensity on non-contrast T1-weighted images, accompanied by increased signal intensity of the surrounding soft tissues on contrast-enhanced T1-weighted images. Findings on T2-weighted and short inversion time inversion-recovery (STIR) images are variable and can appear normal in early stages of disease. Areas with low signal intensity on T2-weighted and STIR images correspond to osteonecrosis. Additionally, there is increased T2-weighted signal intensity and enhancement on contrast-enhanced T1-weighted images at the periphery of the necrotic bone, corresponding to formation of a reactive fibrotic margin and surrounding soft tissue inflammation. In clinically advanced cases, development of a sequestrum is recognized by identifying areas with centrally decreased signal intensity on T2-weighted images, which are surrounded by a high T2-weighted signal intensity peripheral rim. Enhancement of the bone marrow corresponds to low signal intensity on T1-weighted images and indicates the degree of fatty marrow replacement, which often spares the central bony sequestrum. It is important to remember that the signal intensity changes on MRI in patients with BRONJ are not isolated to the affected bony cortex, but encompass adjacent areas including the surrounding soft tissues, bone marrow, inferior alveolar canal, and maxillary sinuses. Enhancement of the adjacent soft tissues often involves the mylohyoid ridge, buccinator muscle, orbicularis oris muscle, and masticator space, with focal areas of mass-like muscle thickening. Additionally, reactive cervical lymphadenopathy is frequently present, most commonly in the submental and jugulodigastric areas secondary to infection of the affected bone.
Nuclear medicine studies, such as 99mTc-methylene diphosphonate (99mTc-MDP) planar and single-photon emission computerized tomography (SPECT) bone scintigraphy, hybrid SPECT/CT systems, as well as [18F] sodium fluoride (NaF) or [18F] fluorodeoxyglucose (FDG) positron emission tomography (PET/CT), are highly sensitive for the detection of BRONJ, especially in the early stages of disease. Typically, these modalities demonstrate increased radiotracer uptake in the majority of cases, which is thought to be secondary to surrounding areas of soft tissue inflammation as well as infection at the site of necrosis. Furthermore, 3-phase bone scintigraphy characteristically reveals increased perfusion and increased blood pool, which is caused by areas of hypervascularity in the affected region. The limiting factor of these functional imaging modalities is their poor spatial resolution and low specificity. However, hybrid systems such as SPECT/CT are able to demonstrate the metabolic difference between the necrotic sequestrum (decreased radiotracer uptake) and surrounding areas of reactive osteoblastic hyperactivity, therefore allowing for precise localization of the osteonecrotic core and enabling differentiation from the adjacent viable bone.
51.4 Differential Diagnosis
The differential diagnosis for bisphosphonate-induced osteonecrosis of the jaw includes osteoradionecrosis, neuralgia-inducing cavitational osteonecrosis, osteomyelitis, bone metastases, and primary bone tumors (osteosarcoma).
Get Clinical Tree app for offline access

Osteoradionecrosis: There is always an accompanying clinical history of radiation therapy to the oral cavity. Osteoradionecrosis causes an increase in the marrow space which is filled with necrotic tissue, followed by bony sequestration demonstrating a typical moth-eaten appearance. Furthermore, osteoradionecrosis may present with ill-defined regions of cortical thickening and sclerosis, loss of trabeculation, soft tissue edema, and pathologic fractures (Fig. 51.4).
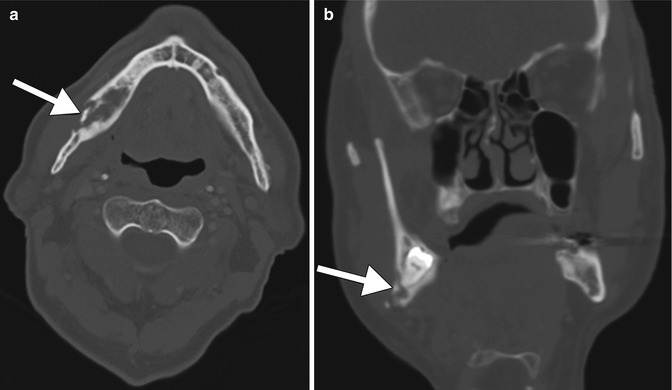
Fig. 51.4
Osteoradionecrosis. Axial (a) and coronal (b) CT images show fragmentation of the lingual cortex of the right mandible body (arrows) associated with surrounding irregular lucency and sclerosis in a patient who received radiation therapy for a right tonsillar squamous cell cancer several years before
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








