Chapter 59 Black Disc
Diagnosis and Treatment of Discogenic Back Pain
The fact that intractable axial back pain may be associated with degenerative changes in the lumbar discs has been recognized for over half a century. Discography was introduced by Lindblom in 19481 to evaluate the disc anatomy for disc herniations. Four years later, Hirsh and Schazowicz2 described the provocation and localization of axial back pain with discography despite a normal myelographic study. Since that time, in spite of a general understanding of the condition, a consensus definition of discogenic back pain has not been achieved.
The lack of consistent terminology to describe symptomatic disc degeneration has added to the controversy. In 1970, Crock3 used the term internal disc disruption as an alternative to describe this process. More recently, the term symptomatic anular tear has been used because of subtle findings on high-resolution MRI and lumbar discography. For consistency in this chapter, we will use the terms discogenic back pain, anular tear, and anular degeneration in reference to symptomatic disc degeneration. Less specific terms such as black disc disease, dark disc disease, postlaminectomy syndrome, and failed back syndrome should be avoided in favor of more specific terminology.
Because of inconsistent terminology and nonstandardized definitions for low back pain, the various causes of back pain have been difficult to differentiate in clinical studies.4 Furthermore, although axial back pain occurs independently of radicular pain in many cases, clinical studies have not routinely distinguished between the causes and treatments of axial back pain as compared with radicular leg pain. Consequently, accurate or reasonable epidemiologic estimates for the incidence, prevalence, or natural history of discogenic back pain as compared with radiculopathy with or without axial back pain are not available.
Causes of Discogenic Pain
Although the most common source of midline axial back pain remains muscular or ligamentous strain, chronic pain associated with specific postural changes can be attributed to either facet joints or intervertebral discs. More specifically, discogenic pain is classically associated with sitting intolerance and flexion of the spine, as compared with pain with spinal extension in cases of facet syndrome. As the body’s largest avascular structure, the intervertebral disc is prone to decreased nutritional uptake and subsequent degeneration. Repetitive motions in the spine from activities of daily life can create shear forces, resulting in microtrauma to the disc. Breakdown of proteoglycans and hydrophilic proteins in the nucleus pulposus leads to disc desiccation, which in turn initiates a cascade of disc height loss, progressive disc collapse, and immobility of the functional spinal unit. This decreased motion may actually lead to mechanical stability through the formation of osteophytes across the affected disc space and gradual resolution of pain, despite continued or progressive degeneration. The natural history and time course of symptoms can vary widely, and a small number of patients remain chronically symptomatic. The dilemma in diagnosis and treatment lies in our lack of understanding of why intervertebral discs with nearly identical morphology can behave differently, some causing patients chronic pain while others remain asymptomatic.5
Progress has been made, however, in understanding the pathophysiology of the lumbar disc as a cause of discogenic pain. The lumbar disc is supplied by a network of pain fibers from the sympathetic chain arising from the sinuvertebral nerve,6 which innervates the outer six layers of the anulus fibrosus.7 With progressive disc collapse, the anulus bulges and tears. Activation of anular nociceptive C-fibers then occurs from direct mechanical stimulation from disc material extending into the outer region of the disc. In addition to causing direct pain, anular tears decrease disc integrity and can cause pathologic loading of the facet joints and end plates, with resultant inflammation. Sprouting of pain fibers into the site of anular injury has also been observed and may be a factor in causing symptoms.8
Pressure changes within the disc provide yet another mechanical mechanism that causes discogenic pain. Intradiscal pressures have been shown to be greatest in the sitting position9,10 and correlate with the symptomatic pattern of discogenic pain, which worsens with sitting and resolves with recumbency. Clinically, a lumbar disc herniation can present with an initial history of acute back pain prior to the development of radicular leg pain. Some patients report the resolution of this initial back pain with simultaneous acute new onset of radicular leg pain. Although cause and effect are difficult to prove, it has been postulated that the initial pain from a symptomatic anular tear resolves as internal pressure on the anular pain fibers decreases with herniation of nuclear material into the spinal canal.
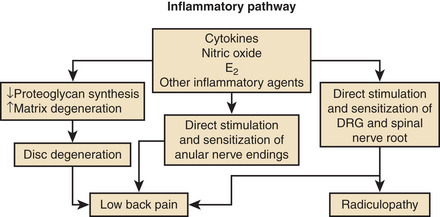
In addition to mechanical sources of pain, a wide variety of putative inflammatory agents, such as phospholipase A2, metallomatrix proteinases, and prostaglandins, have been reported to occur in the nucleus pulposus as part of the degenerative process (Fig. 59-1).11–13 Leakage of these substances into the outer anulus may be another mechanism of pain generation in degenerative disc disease. Exposure of the dorsal root ganglion to these same noxious agents has also been shown to result in histologic damage to the myelin sheaths and ganglion.14,15 This inflammatory process may be the basis of neuropathic pain, which may accompany discogenic pain.
Clinical Presentation
Despite the description of significant pain, the physical examination is usually normal; by definition, the diagnosis of discogenic back pain excludes findings associated with nerve compression. On close observation, the patient may exhibit a tendency for frequent position changes, a relative intolerance to sitting, and pain on forward flexion. The absence of physical findings may prompt the diagnosis of malingering or psychogenic pain. Formal psychometric testing should be used liberally to rule out potential psychosocial issues and to quantify the effect of long-standing pain on coping mechanisms.16,17 Abnormal psychological factors, in addition to the presence of active litigation, tobacco use, and disability, are predictive of a poor outcome with surgical treatment.18 Close observation of the patient at the time of discography can be helpful in further substantiating the presence or absence of psychological risk factors, and some institutions use video recordings for accurate recording of the patient’s response at the time of testing.
In addition to pain of discogenic origin, there are alternative sources of activity-related back pain. Myofascial and ligamentous pain tend to be more superficial, diffuse, and sharp; often have significant local tenderness; and are less associated with sitting intolerance. Facet pain from facet arthropathy typically occurs with extension maneuvers of the spine and improves with flexion. Tumors may present with vague back pain symptoms but are rarely missed with current MRI capabilities. Osteoporotic or pathologic fractures frequently present with isolated back pain but are easily recognized with standard radiographs and CT and with MRI scans in the acute setting. Isthmic spondylolisthesis can result in chronic back pain or be asymptomatic and may present with acute back pain in adolescent patients, while older patients more often present with radiculopathy. An incomplete transitional vertebra syndrome with unilateral or bilateral pseudojoint formation between the enlarged L5 transverse process and sacral ala can also be a potential source of pain and can be easily missed without an angled anteroposterior (Ferguson’s) plain radiograph of the lumbosacral junction.
Diagnostic Imaging
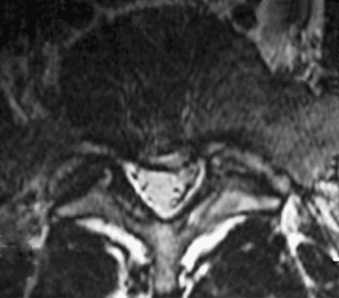
Without specialized testing, discogenic back pain secondary to lumbar degenerative disc disease is not adequately assessed by conventional radiography, CT, and MRI scans. Typical radiographic findings include loss of disc space height, end-plate sclerosis, osteophyte formation, and disc bulge, consistent with spondylosis, which may also be found in asymptomatic patients.19,20 Standard spine radiographs are warranted to rule out spinal instability but are otherwise unhelpful in the diagnosis of symptomatic anular tear. With the advent of MRI, the entire spine can be screened for degenerative processes. While the so-called black disc features nonspecific imaging changes that are consistent with loss of water content (and the disc therefore appears hypointense on T2-weighted imaging), a unique finding referred to as a high-intensity zone (HIZ) in the dorsal anulus has been described on MRI consisting of a discrete hyperintensity within the dorsal anulus.21 The HIZ lesion has been thought to represent either disc material visualized within an anular tear or edema fluid located within the dorsal anulus (Figs. 59-2 and 59-3). While this finding may be suggestive and helpful in localizing the site of pain, it may also be asymptomatic.22–24
Additional MRI findings have been characterized by Modic et al.,25 who described signal changes in the vertebral bodies adjacent to the affected disc space that may have clinical implications correlating with discogenic disease. Modic type I changes are hypointense on T1 and hyperintense on T2 sequences and signify bone marrow edema. These findings are indicative of acute changes in the vertebral body, have a high specificity for discogenic back pain, and may warrant further workup for the possibility of treatment.26,27 Modic type II changes indicate marrow replacement by fat, are bright on both T1 and T2 sequences, and signify chronic degenerative changes involving the vertebral body and intervertebral disc that are less likely to be associated with discogenic pain.27 Modic type III changes are dark on both T1 and T2 sequences, indicating sclerotic vertebral end plates that are clinically insignificant.
While these MRI findings may be helpful for localization of a potential pain generator, the diagnosis should be confirmed with provocative testing of the disc space via discography.28 With the advent of water-soluble contrast agents and MRI, discography has been used primarily for the evaluation of chronic axial discogenic back pain. Patients with a consistent clinical history who have greater than 50% low back pain compared with lower-extremity pain warrant further investigation with discography.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree