Chapter 26 Treatment of spinal deformities can be operative or nonoperative. Surgical treatment involves direct bony manipulation using instrumentation to eventuate fusion in a corrected position. Nonoperative treatment has less lofty, but equally important, goals. Numerous methods of nonoperative treatment have been used, including traction, electrical stimulation, and stretching, though only bracing and casting have demonstrated clinical efficacy. Bracing and casting rely on indirect manipulation of spinal curvatures, with the primary goal usually being arrest or prevention of deformity. The indications and goals for nonoperative treatment of spinal deformities vary with different diagnoses. For instance, bracing is indicated to treat idiopathic adolescent scoliosis curves between 30 degrees and 45 degrees in a skeletally immature patient. In this instance, cessation of curve progression is a positive result. In conditions such as Scheuermann’s kyphosis, bracing may in fact be effective in maintaining a corrected spine. In contrast, bracing patients with spondylolisthesis is usually for symptomatic relief of back pain, although it may aid healing of the lytic defect in some adolescent cases with minimal or no slip. It is the purpose of this chapter to discuss the available methods, indications, and outcomes of nonoperative treatment. A focus is placed on bracing, a mainstay of nonsurgical management of spinal deformities, with an expanded discussion of its role in idiopathic scoliosis. Prevention of spinal deformity can take many forms. It may be (1) prenatal or preconception, as is the case for myelomeningocele; (2) centered around early diagnosis, such as school screening for idiopathic scoliosis or regular radiographic follow-up after a thoracolumbar burst or compression fracture; (3) intraoperative, such as the decision to fuse after sacrifice of more than 50% of the facet joints and pars interarticularis during posterior decompression. Genetic counseling may alert prospective parents of a propensity toward specific congenital deformities with proposed hereditary patterns.1 Preemptively, maternal folate intake prior to conception decreases the chance of congenital neural tube defects (myelomeningocele).2 After conception, prenatal screening, including -fetoprotein levels and ultra-sound, are useful in the early detection of neural tube defects. In the fetus or neonate, congenital spinal defects should be suspected when other anomalies are present. Genitourinary and cardiac malformations are present in 20% and 12% of children, respectively, with congenital spinal disorders. In the preteen stage, school screening can help detect mild idiopathic scoliotic curves early on when they may be amenable to nonoperative measures. Regular inspection by a pediatrician can aid early diagnosis of kyphotic disorders such as Scheuermann’s disease, which may be correctable with brace treatment in its early stages. Congenital curves are highly progressive and usually necessitate surgical intervention at initial presentation.3 However, early detection may help lessen the amount and complexity of surgery required. There are several avoidable iatrogenic causes of spinal deformity. Postirradiation kyphosis can be prevented by excluding the spine from the radiation field, if possible, with nonspinal tumors.4 Late-onset kyphosis is a common sequelae associated with laminectomy without fusion in the thoracic spine. Postlaminectomy kyphosis can be prevented or minimized by maintaining at least 50% of the facet joint integrity or fusing when this criterion cannot be met.5 In children, postlaminectomy kyphosis can develop as late as 6 years after surgery, necessitating long-term radiographic follow-up.6 Iatrogenic postoperative deformities may also occur secondary to either a failed arthrodesis or incorrect selection of fusion levels.7,8 Bracing has been largely ineffective in the management of postlaminectomy and postirradiation kyphosis.4 Kyphosis is a common radiographic sequelae after nonoperative treatment of thoracolumbar burst fractures. Although the clinical significance of these deformities remains to be defined, early treatment in a hyperextension brace is often employed to prevent collapse at the fracture site.9 Patients can be treated with a Jewett extension brace or custom-molded thoracolumbar sacral orthosis (TLSO). Interestingly, the efficacy of brace or cast treatment to prevent local kyphosis after compression fractures or so-called stable burst fractures has yet to be demonstrated in a prospective clinical trial. Spinal bracing attempts to position the vertebral column in a corrected or overcorrected position. This is achieved indirectly through externally applied forces. Forces are applied to the skin and transmitted to subcutaneous skeletal structures that are confluent with the vertebrae. Posteriorly, the spinous processes are largely subcutaneous and accessible for brace contact. Anteriorly, thoracic and abdominal viscera cover the spine. This creates a deficiency of direct contact points. Pelvic structures, such as the iliac crest, can be used to influence the position of the lower lumbar spine. The subcutaneous path of the ribs and sternum make them a viable site for deformity-correcting contact areas. Though no longer popular because of the development of dental deformities in young patients as well as poor compliance,10 the mandible has also been used as a site of brace contact to enable better control of the upper thoracic spinal column. Brace correction of a deformity requires a 3-point bending moment applied to a flexible spine. For coronal deformities, a lateral force is applied at the apex of the convexity while contralateral forces above and below the apex are simultaneously applied. With scoliosis, coronal force vectors are produced at the lateral rib cage or iliac wing. In vivo studies have correlated the amount of force exerted through the brace to the percentage of curve correction.11 The axilla is the upper limit of coronal contact areas, making control of levels above T4 difficult with underarm bracing.11 Control of upper thoracic scoliosis can include use of mandibular pads (Milwaukee brace). Rotational deformity is not directly corrected by bracing maneuvers but is rather indirectly influenced by coupled lateral flexion-rotational motion. Hyperextension bracing or casting can be useful for kyphotic curves. Correction vectors are applied to the sternum, anterior iliac spines, and spinous processes. Broad sternal pads (Jewett-type brace) can deliver a posterior force to the upper thoracic spine while strong anterior forces are delivered to the kyphotic apex through the spinous processes.12 Braces are limited by several factors. The forces applied must be compatible with tissue survival, as skin breakdown and pressure necrosis are known complications. Contact pads with large surface areas dissipate corrective forces over broader surfaces and relieve concentrated points of pressure. This, and frequent clinical monitoring of the integument, can help prevent these complications. Braces are also limited in that corrective forces are broadly applied and cannot be precisely directed toward one specific vertebra. In addition, these vectors are applied at a significant distance from the spinal column and thus much of the corrective forces are dissipated within extravertebral tissues. The Charleston brace is a custom-made, underarm TLSO (Fig. 26–1). It relies on achieving overcorrection of the scoliotic curve, which is achieved by tightening the straps. It is worn only part-time, usually at night. The Wilmington brace was developed in an attempt to improve the cosmetic appeal of the brace and, in turn, the wear compliance. It is custom-molded from a single-piece of plastic (Fig. 26–2). Figure 26–1 The Charleston brace is a custom-made underarm thoracolumbar sacral orthosis (TLSO). Figure 26–2 The Wilmington brace was developed in an attempt to improve the cosmetic appeal and wear compliance of the brace. It is custom-molded from a single piece of plastic. The Milwaukee brace was the first device designed to treat idiopathic scoliosis. It includes a form-fitting apron that rests upon subcutaneous pelvic bony protuberances, notably the iliac crests, anterior and posterior superior iliac spines, and ischial tuberosities. Longitudinal uprights span the abdomen and thorax to support occipital and mandibular pads (Fig. 26–3). An adjustable side pad is used to deliver curve correcting force. It is a full-time brace. The Boston brace was the first underarm brace introduced to treat scoliosis (Fig. 26–4). Lateral correcting forces are delivered above the apex through the underarm bar and below the apex through the apron portion of the brace. This enables a large window cut-out on the concave side of the curve. It is intended to be worn full-time. The Jewett hyperextension brace is an example of an adjustable, non-custom-molded, “off the shelf” device that can be used to correct hyperkyphosis. In comparison with a form-fitting TLSO, it offers little rotational control. It is most often used to treat Scheuermann’s kyphosis and some traumatic thoracic or lumbar fractures. The antilordotic brace was designed to hold the lower lumbar spine in a flexed position. It is thought that this posture can relieve the shear stresses on the pars interarticularis and encourage healing in patients with spondylolytic lesions. Nonoperative decision-making for idiopathic scoliosis is influenced by the degree and progressivity of the curve. Scoliotic curves measuring between 10 degrees and 20 degrees warrant close observation. Radiographs should be obtained every 6 to 12 months until skeletal maturity to detect progression of the deformity. For those with curves between 20 degrees and 30 degrees, observation should include radiographs every 4 to 6 months until skeletal maturity. Figure 26–3 The Milwaukee brace includes a form-fitting apron that rests upon subcutaneous pelvic bony protuberances and longitudinal uprights that support occipital and mandibular pads. Figure 26–4 The Boston brace was the first underarm brace introduced to treat scoliosis. The indications for brace treatment have varied over the past decade. Recently, the indications for surgery have become more stringent, increasing the number of patients who are “braceable.” Brace treatment may be indicated for skeletally immature patients with curves that measure between 30 degrees and 45 degrees. Progressivity can warrant bracing curves that would otherwise be treated by observation alone. Specifically, 5 degrees of radiographically documented progression in a patient with a 25-degree curve may be an indication. Bracing may have a more limited role in boys than in girls, with recent data suggesting that results are inferior in adolescent male patients, most likely because of poor wear compliance. There is currently minimal to no role for electrical stimulation in the treatment of idiopathic scoliosis because of lack of supporting evidence.
Bracing and Nonoperative Treatment of Spinal Deformity
♦ Prevention and Early Detection of Spinal Deformity
♦ Biomechanical Principles of Spinal Bracing
General Principles
Coronal Deformity
Sagittal Deformity
Biomechanical Limitations
♦ Brace Types
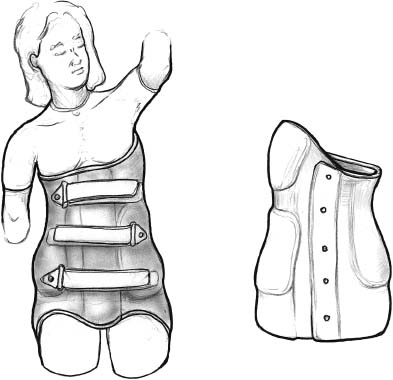
Charleston Brace
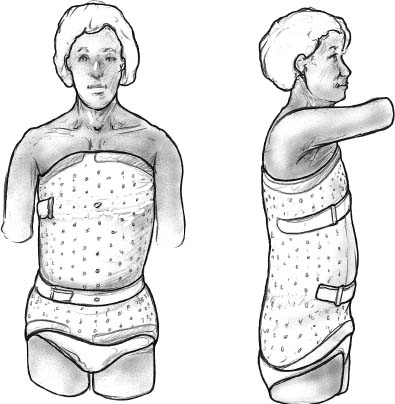
Wilmington Brace
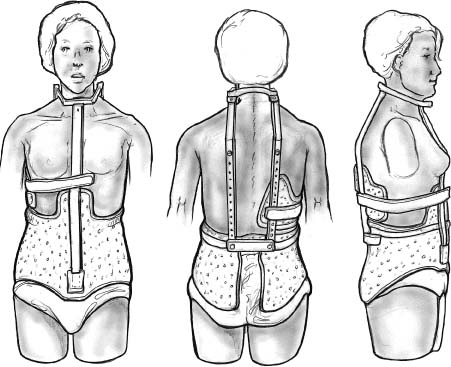
Milwaukee Brace
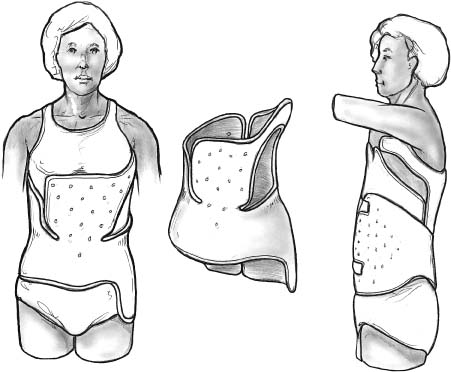
Boston Brace
Jewett Hyperextension Brace
Antilordotic Lumbosacral Brace
♦ Bracing and Nonoperative Treatment for Specific Spinal Conditions
Adolescent Idiopathic Scoliosis
Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree