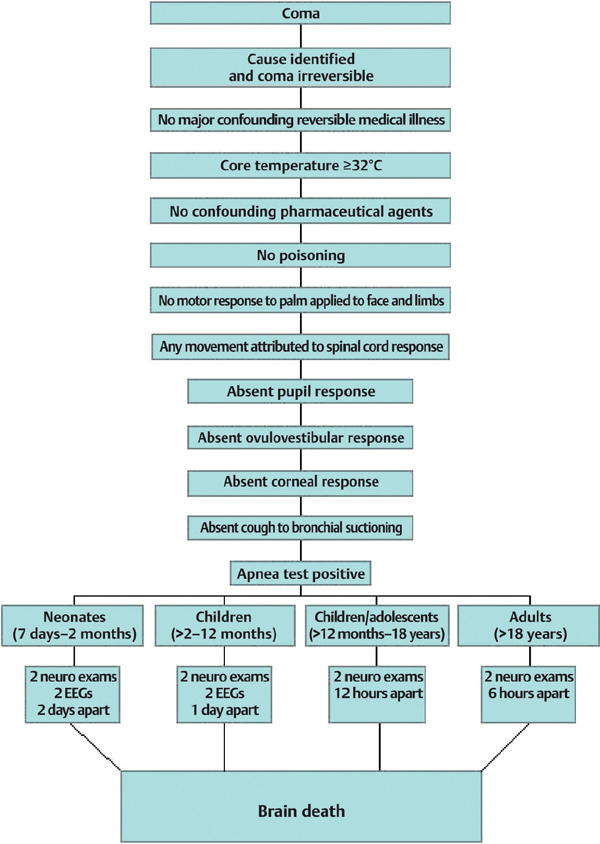
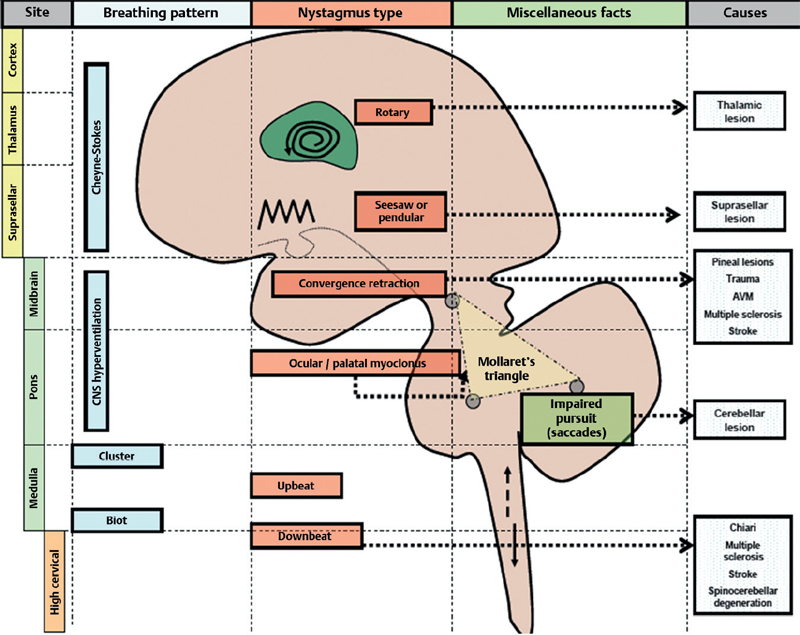
33 What is the definition of brain death? Irreversible cessation of function of the brain, including the brainstem1–4 What are the three most common causes of brain death in adults (in descending order)? 1. Traumatic brain injury (TBI) and subarachnoid hemorrhage (SAH) 2. Hypoxic-ischemic brain damage 3. Fulminant hepatic failure1–4 What are the three most common causes of brain death in children (in descending order)? 1. Abuse 2. Motor vehicle accidents What is a common transitory appearance of the pupil in brain death? An oval shape Fig. 33.1 An algorithm for diagnosing brain death. (Courtesy of Dr. Eelco Wijdicks.) What is the procedure for testing oculovestibular (OV) responses? Cold water calorics, aka the caloric reflex test: irrigate a single ear canal with 50 mL of ice water with the head elevated to 30 degrees. Wait about 1 minute for a response and 5 minutes before testing the opposite ear canal. (Be sure to rule out tympanic membrane perforation before beginning!)1–4 What is the pathologic oculovestibular (OV) response in a comatose patient with an intact brainstem? Tonic conjugate eye deviation toward the irrigated ear without nystagmus What does an inability to adduct the ipsilateral eye during OV testing indicate? An ipsilateral brainstem lesion of the medial longitudinal fasciculus (MLF). Internuclear ophthalmoplegia (INO), seen unilaterally in elderly comatose patients with brainstem infarcts and bilaterally in multiple sclerosis, produces this response with this procedure.1–4 What is the anticipated response of a normal awake patient who receives OV testing? Slow eye deviation toward the side of cold stimulus (usually the irrigated ear), followed by nystagmus beating to the opposite direction. Remember the mnemonic COWS: Cold-Opposite; Warm-Same, describing the normal direction in which the nystagmus will beat. When would one strongly suspect brain death? When all brainstem reflexes are absent in a comatose patient and the cause of coma is known and irreversible. What are the prerequisites for the apnea test? Prerequisites are: 1. Core temperature ≥32.2°C 2. Systolic BP ≥90 mm Hg 3. Normovolemia 4. Normocapnia 5. Normoxemia Describe the apnea test procedure. 1. Connect a pulse oximeter to the patient’s finger. 2. Disconnect the ventilator. 3. Supply 100% oxygen at 6 L/min for approximately 15 minutes. (The oxygen cannula should be near the level of the carina.) 4. Examine patient closely for respiratory movements. Respiration is defined as chest or abdominal excursions that result in adequate tidal volumes. 5. Measure arterial PO2, PCO2, and pH via ABG after about 8 minutes and reconnect the ventilator. 6. If there are no spontaneous respirations and arterial PCO2, is ≥ 60 mm Hg or there is an increase of 20 mm Hg in the PCO2 above baseline after at least 2 minutes, then the apnea test is interpreted as positive (supporting a diagnosis of “brain death”). 7. If spontaneous respirations are observed, the apnea test is interpreted as negative (warranting premature termination of the exam). 8. If hypotension, desaturation, or dysrhythmia occurs, the apnea test is interpreted as an occurrence of cardiovascular or pulmonary instability (requiring a confirmatory test). 9. If there are no spontaneous respirations and the posttest arterial PCO2, is <60 mm Hg without cardiovascular instability, the apnea test is interpreted as inconclusive (warranting repetition with 10 minute. of apnea).1–4 In whom should an apnea test be terminated prematurely? 1. A breathing patient 2. A hypotensive patient 3. A patient with a SpO2 <80% via pulse oximeter 4. A patient experiencing a cardiac dysrhythmia What confirmatory testing exists for the diagnosis of brain death? 1. Conventional cerebral angiography 2. Electroencephalography (EEG) 3. Transcranial Doppler (TCD) 4. Cerebral radionuclide angiogram (CRAG) 5. Somatosensory evoked potentials (SSEPs) What findings of cerebral angiography are consistent with brain death? Absent intracerebral filling at the level of the carotid bifurcation or circle of Willis. External carotid circulation is patent; however, filling of the superior sagittal sinus may be delayed. This method is not routinely used to diagnose brain death. What is the characteristic finding on electroencephalography (EEG) to confirm brain death? Loss of cerebral electrical activity, also known as electrocerebral silence (ECS). However, transient persistence of electrical activity can occur for as long as 170 hours after the clinical diagnosis of brain death has been made. What findings of transcranial Doppler (TCD) are consistent with brain death? (1) Small systolic spikes in early systole, followed by (2) a bidirectional systolic flow pattern with retrograde diastolic flow, and finally (3) an absence of diastolic flow or reverberating flow altogether, indicative of markedly elevated intracranial pressure (ICP) (above MAP) and arrest of cerebral circulation. What is the typical finding in a brain dead patient with cerebral radionuclide angiogram (CRAG)? Lack of uptake of radionuclide in brain parenchyma, called the “hollow skull phenomenon” What finding on somatosensory evoked potentials (SSEPs) is consistent with brain death? Bilateral absence of N20-P22 response with median nerve stimulation What cardinal clinical findings must be documented for the diagnosis of brain death? 1. Presence of coma (complete loss of consciousness, verbalization, and spontaneous motor activity) 2. Absence of brainstem reflexes: a. Light reflex b. Corneal reflex c. Oculovestibular reflex d. Oculocephalic reflex e. Gag and cough reflex 3. No response to deep central pain 4. Presence of apnea 5. Absence of confounding factors that could simulate brain death on exam (such as hypotension, hypothermia, systemic drugs, or pharmacologically induced coma) 1. Severe facial or cervical spine trauma 2. Emergence from barbiturate coma (levels must be ≤10 μm/mL) 3. Pupillary abnormalities (fixed and dilated pupils as with atropine or previous cataract surgery) 4. Hypothermia 5. Hypovolemic shock 6. Anoxia/hypoxia 7. Toxic drug or metabolic levels 8. Sleep apnea or severe pulmonary disease with chronic retention of carbon dioxide (i.e., congestive heart failure [CHF] and chronic obstructive pulmonary disease [COPD]) Confirmatory testing is recommended in the above circumstances. Why should brain death remain a presumptive diagnosis in the ER? The diagnosis should remain presumptive and organ donation should not occur from the ER because adequate time and consideration should be paid to consider confounding causes of coma and to find reversible causes if present. Before a patient is removed from the ventilator, what step is mandatory for procurement in the U.S.? Brain dead patients must be reported to local organ procurement organizations before they can be removed from the ventilator. How long is cardiovascular support required when an individual’s organs have been committed for donation? This will continue either until the organs are safely procured from the deceased individual or immediately following extubation of an individual who is no longer suitable for donation or whose family later withdraws donation. Note to the reader: Some of the information contained in this chapter is a matter of the authors’ opinion and should not be regarded as absolute fact. What is the ethical obligation of the physician in terms of organ donation? To approach the family of an individual who meets the criteria for brain death to discuss the possibility of organ donation; to discuss all suitable organs specified for donation; to facilitate organ procurement in such a way as to avoid disfigurement and honor the family’s wishes to hold an open-casket funeral; and to provide information detailing the ultimate use of the recovered organs What consolation do many families find by participating in organ donation? They may find solace in the fact that, although posthumously, their loved one will give the gift of life to someone who stands to benefit greatly from their generosity. What is the potential conflict of interest that could arise when a full-code patient nearing death has decided on organ donation? A conflict of interest potentially exists between a medical team’s apparent duty to perform “heroic measures” on a patient who is expected to fully succumb to his or her disease, potentially losing organs currently suitable for donation, and the team’s ulterior desire for another patient to obtain desperately needed organs that offer a cure only if promptly donated. What steps can a physician take to appease a family’s natural reservations about organ donation? 1. Avoid heavy involvement by other medical teams (e.g., transplant surgery) when deciding to diagnosis brain death in the patient. 2. When scheduling a family meeting to discuss organ and tissue donation, involve physicians who are both empathetic and experienced with discussing uncomfortable topics and breaking bad news. What is the significance of the Uniform Determination of Brain Death Act? In the U.S., this act acknowledges the principle that death can be diagnosed when neurological criteria for brain death are fulfilled. Fig. 33.2 High-yield graph relating breathing patterns in comatose states and nystagmus depending on location.
Brain Death
33.1 Basic Concepts
33.2 Testing for Brain Death
33.3 Certification of Brain Death
33.4 Organ Donation
33.5 Ethical and Legal Issues in Brain Death
33.6 High-Yield Coma Facts
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






