Brain Edema, Increased Intracranial Pressure, and Herniations
Juan C. Troncoso
Brain edema and herniations are common findings in forensic neuropathology autopsies. In most cases they are due to trauma, but they may also be due to hypoxic-ischemic encephalopathy, infarcts, and occasionally tumors.
The brain is contained in the skull, a container that becomes inextensible after the closure of the sutures in early infancy. Therefore, when the brain becomes swollen or displaced by a mass lesion of any sort, such as a hematoma or tumor, it has limited space to accommodate such changes before herniating through natural or surgical openings. Also, the brain parenchyma shares the intracranial space with two other compartments: the cerebrospinal fluid (CSF) within the ventricular system and subarachnoid space (approximately 150 mL) and the vascular compartment, which includes the blood in capillaries, arteries, and veins (approximately 150 mL, 50 mL in the brain parenchyma and 100 mL in subarachnoid vessels and dural sinuses). The normal intracranial pressure is less than 150 mm of water, a value that fluctuates during the day.1 The normal opening pressure of CSF by lumbar tap has been traditionally accepted as between 180 to 200 mm of water, but a recent study expands that range to 100 to 250 mm of water.2 As the intracranial pressure increases, the volume of CSF and vascular compartments can be reduced, offering transient and limited compensation. Once this compensatory mechanism is overcome, the brain parenchyma herniates through the tentorial notch or the foramen magnum, under the falx cerebri, or through a craniotomy. These herniations, ominous in their own right, lead to further distortions of brain structures, hemorrhages, and infarcts. These secondary changes must be distinguished from primary traumatic and vascular events.
INTRACRANIAL COMPARTMENTS
The intracranial volume in the adult is approximately 1, 700 mL, of which 1, 400 mL is brain, 150 mL is blood, and 150 mL is CSF. The blood volume is divided into 50 mL in the brain parenchyma and 100 mL in vessels in the subarachnoid space and dural sinuses. The regulation of the intracranial volume of blood is complex, and within certain limits its net result is the preservation of a constant cerebral blood flow (CBF) without a net increase in intracranial blood volume (i.e., shift of blood volume from pial vessels to the parenchyma). Under pathologic circumstances, however, this autoregulation will stop working.3
HYDROCEPHALUS
The term hydrocephalus indicates dilation of the ventricular system. Hydrocephalus can be caused by the obstruction of CSF circulation, for example, by a narrow aqueduct of Sylvius or by a tumor of the fourth ventricle. This is known as obstructive hydrocephalus (Fig. 8.1). If the outflow of CSF from the ventricular system into the subarachnoid space is normal, but the circulation within the subarachnoid space is impaired or the reabsorption of CSF into the venous system is blocked, then the hydrocephalus is called communicating. This is a common delayed complication of subarachnoid hemorrhages. Finally, a third type of ventricular enlargement is caused by atrophy of the brain; this is called hydrocephalus ex vacuo, and it is common in degenerative diseases and postanoxic encephalopathies (Fig. 8.2).
BRAIN EDEMA AND BRAIN SWELLING
Brain edema is defined as increased water content of the brain parenchyma, leading to increased tissue volume.4 The term “brain swelling” is less specific, as it encompasses also an increase in brain volume caused by expansion of the intravascular or ventricular compartments
of the brain. Among several mechanisms that can cause brain edema, the most relevant to forensic neuropathology are the cytotoxic and vasogenic types of edema, first described by Klatzo.5 In cytotoxic edema, increased water content within neurons and astrocytes occurs, whereas in vasogenic edema, increased extracellular water is present secondary to disruption of the blood-brain barrier (BBB) or cellular injury.6 Other types of brain edema include the interstitial type7 and osmotic type, associated with necrotic brain lesions.8
of the brain. Among several mechanisms that can cause brain edema, the most relevant to forensic neuropathology are the cytotoxic and vasogenic types of edema, first described by Klatzo.5 In cytotoxic edema, increased water content within neurons and astrocytes occurs, whereas in vasogenic edema, increased extracellular water is present secondary to disruption of the blood-brain barrier (BBB) or cellular injury.6 Other types of brain edema include the interstitial type7 and osmotic type, associated with necrotic brain lesions.8
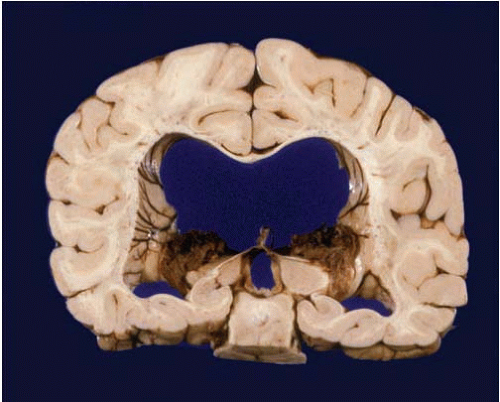 FIG. 8.1. Obstructive hydrocephalus. Massive enlargement of the ventricular system secondary to chronic obstruction of the aqueduct. |
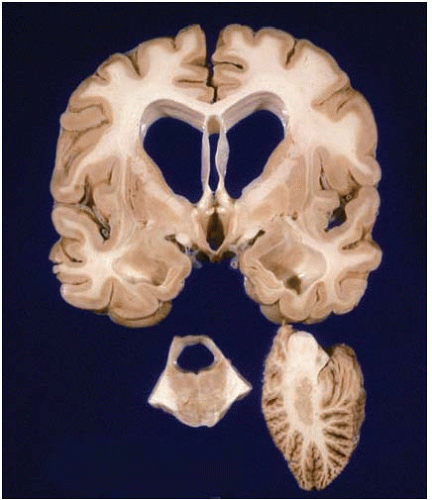 FIG. 8.2. Hydrocephalus ex vacuo. This subject suffered a cardiac arrest and anoxic encephalopathy several years before death. There is marked atrophy of the cerebrum, brainstem, and cerebellum. |
Cytotoxic Brain Edema
Cytotoxic brain edema is characterized by cell swelling as water accumulates within neurons and astrocytes. As astrocytes outnumber neurons 20:1 in the human brain and can swell to five times their normal size, the swelling of astrocytes is the main factor of cytotoxic brain edema.9 Three mechanisms lead to cytotoxic brain edema: (1) increased permeability of cell membrane to sodium (Na+) and potassium ions (K+), (2) energy depletion and impairment of ion pumps, and (3) uptake of osmotically active solutes (i.e., Na+). The excitatory neurotransmitter glutamate has an important role in the development of cytotoxic brain edema, as activation of glial and neuronal glutamate transporters is associated with the influx into the cells of water-binding ions such as Na+, hydrogen ion, and calcium ions.10 A recent development in the pathophysiology of cytotoxic brain edema is the discovery of Aquaporin4 (AQP4), a transmembrane water channel, in astrocytic end-feet. Under normal conditions, AQP4 transports water from the extracellular compartment into astrocytes, 11 but in pathologic circumstances, this mechanism may contribute to cell swelling. In fact, AQP4 knock-out mice are relatively resistant to brain edema after water intoxication or cerebral ischemia.12
Vasogenic Brain Edema
Vasogenic brain edema is caused by disruption of the BBB, leading to accumulation of water rich in albumin and other plasma proteins in the interstitial space.5, 13 The BBB is critical for the homeostasis of the brain, as well as for maintenance of normal brain volume. The anatomical substrates of the BBB are tight junctions among capillary endothelial cells that prevent the free passage of proteins from the plasma into the brain.14 The BBB can be disrupted in multiple ways, including mechanical trauma, ischemia, inflammation, and tumors.
Brain Edema in Forensic Neuropathology
In forensic autopsies, the most common causes of brain edema are usually trauma or hypoxic-ischemic injury and, frequently, their combined effects. Traumatic brain injuries produce a combination of vasogenic and cytotoxic brain edema. The traditional view, based on experimental studies of cryogenic lesions, was that traumatic brain edema was predominantly vasogenic as a result of opening of the BBB associated with contusions. This view is also supported by observations of vasogenic edema and BBB opening in experimental lesions produced by an impact acceleration model.15, 16 More recent work, however, with use of the “control cortical impact injury” experimental model, has revealed that the edema both at the site of contusion and the surrounding tissues is predominantly cytotoxic.17 In humans with traumatic brain injury, magnetic resonance imaging studies within the first 24 hours after injury have revealed no evidence of BBB leakage, but signs of cellular edema in the periphery of contusions18 as well as diffusely19 have been noted. In concert, experimental and clinical studies provide evidence that the edema of traumatic brain injuries has both vasogenic and cytotoxic components.
In ischemic brain lesions, brain edema is initially cytotoxic and subsequently vasogenic. When CBF decreases to less than 10 mL/100 g/min, ion exchange pumps begin to fail and cytotoxic edema develops. Subsequently, and particularly if CBF is further reduced, the BBB breaks down, allowing the extravasation of water and plasma proteins from the capillaries into the interstitial brain space. In experimental paradigms with complete ischemia, water accumulates in cells within a few minutes, but the BBB remains intact for 3 to 6 hours. An important factor in the development of BBB damage is the restoration of CBF and the reperfusion injury.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








