Accidents and acts of violence account for the majority of injuries of the spinal cord seen at forensic institutions, hence the majority of spinal cord lesions examined by the forensic neuropathologist are traumatic, whereas vascular, infectious, and neoplastic cord lesions are more common in hospital settings. Several considerations are pertinent in the forensic examination and interpretation of cord injuries. Although the clinical and functional consequences of spinal cord injuries are frequently devastating, advances in the medical management of these patients allow many of them to survive for many years, including those with high cervical injuries. In cases of remote spinal cord injury, it is important and challenging to determine whether the cause of death is a consequence of the spinal cord injury, its complications, or else is due to unrelated causes. If death is deemed to be related to a remote spinal cord injury, the manner of death will depend on the nature and circumstances of the original traumatic event (i.e., accident, suicide, or homicide). In addition to the damage produced at the time of the injury, secondary vascular pathology plays a critical role in the pathogenesis of some long-term complications.
EPIDEMIOLOGY OF SPINAL CORD INJURIES
In the United States, according to statistics provided by the Spinal Cord Injury Information Network,
1 the estimate of the annual incidence of spinal cord injury (excluding people who die at the time of the event) is 40/million population/per year (about 11, 000 new cases per year), and the current prevalence of individuals with spinal injuries exceeds a quarter of a million people. The male-to-female ratio is approximately 4:1, and most subjects are in their second to fourth decades of life when they are injured. Almost half of the injuries (44.5%) result from motor vehicle accidents, followed by falls, inflicted trauma (especially gunshot wounds), and sport and recreational accidents. Of the survivors, the most common diagnosis upon hospital discharge is incomplete tetraplegia (one-third of injured subjects), followed by complete paraplegia (one-fourth of injured subjects), and the remaining have either complete tetraplegia (one-sixth of injured subjects) or incomplete paraplegia (one-sixth of injured subjects). Less than 1% of individuals discharged after spinal cord injuries are functionally fully recovered.
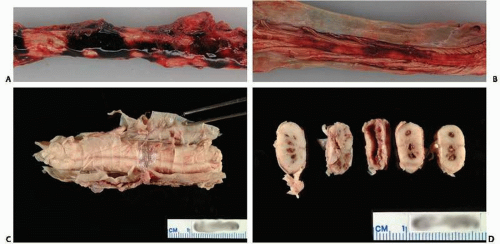
The incidence of spine and spinal cord injuries in people who die at the time of the injury or shortly thereafter is not as well defined, because prospective systematic postmortem studies involving individuals who died immediately or shortly after the traumatic event are lacking. Examination of the spine and spinal cord may require removal, fixation, and sectioning of the spine with the spinal cord inside.
In spite of the relatively high frequency of spinal pathology after trauma, it is difficult to assess the relative incidence of spinal and spinal cord lesions by type of trauma. Reasons for this are discussed below.
First, there are key methodologic differences in the study of nonlethal versus lethal injuries, with differing rates of false-positive and false-negative results. Functional radiology and neurologic exploration (
Table 12.1) are the main methods used for diagnosis in hospitalized patients, and static radiology and/or anatomic exploration are the main methods used in people who died at the scene. Plain radiographs may miss up to 30% of cervical spinal fractures as compared with computed tomography (CT) scans.
2 CT scans miss nonosseous lesions that would be readily detectable by magnetic resonance imaging (MRI), and routine evaluation of the spine at autopsy does not detect some bone lesions or occult trauma in individuals dying after a motor vehicular collision.
3 A comparison of the clinical deficits and the neuropathologic lesions in the same individuals may show significant discrepancy.
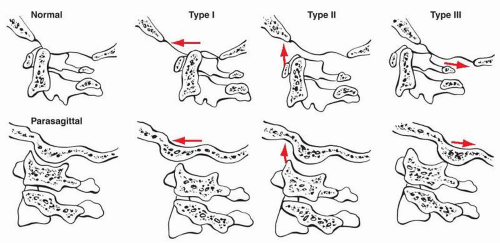
4Second, the postmortem examination and, specifically, the exploration of the spine and spinal cord varies not only among different localities, or different pathologists, but also varies on a case-bycase basis. Postmortem radiologic studies are not performed universally, and vertebral examination in the majority of autopsies is limited to visualization of the anterior vertebral bodies and the atlanto-occipital joint, the spinal cord is not extracted and examined in all cases, and horizontal sectioning and microscopic studies are performed in even fewer cases. Kakulas and Taylor
5 emphasize that parasagittal disc or facet joint lesions, common in whiplash injury, are missed if only radiographs or naked eye examination of the cervical spine are performed.
Third, epidemiologic assessments of cord injury based on hospital discharge or autopsy diagnoses may include a large number of false negatives, because spinal cord lesions may not have been specifically sought and ruled out.
TRAUMATIC LESIONS OF THE SPINE
When linear (compression, distraction, or translation) or angular (flexion, extension, torsion, or lateral flexion) forces to the spine exceed the physiologic range of movement of the area placed in motion, the muscles, ligaments, or bones may fracture, the joints may displace, and the volume of the spinal canal may decrease, with the potential of stretching or compressing the spinal cord. Spinal injury does not necessarily imply spinal cord injury, and alternatively, spinal cord injury may take place in the absence of osteoligamentous lesions, as may occur to young individuals with less brittle, more malleable bones. In addition to primary spinal cord injuries, swelling or vascular damage may aggravate the original lesions by adding an ischemic component to the primary lesion.
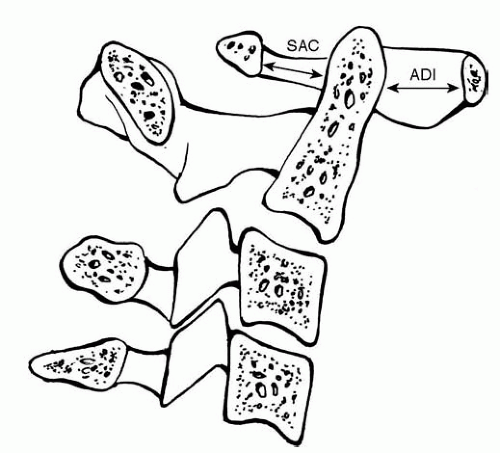
Any temporal or permanent disruption of the spinal canal may produce temporal or permanent damage to the spinal cord. Injuries involving the cervical spinal cord are of importance in forensic neuropathology because they may be the cause of death, whereas thoracolumbar injuries cause significant morbidity and may carry long-term complications, including death. The postmortem determination of spinal injuries is best done, when possible, by both radiologic (CT scan is better than plain radiograph, and MRI is better than CTscan) and direct examination during autopsy. Radiographic studies will detect exaggerated kyphosis or lordosis, misalignments, widening or narrowing of intervertebral spaces, uneven distance between spinous processes, or retropharyngeal swelling better than direct inspection at autopsy. Visual inspection at autopsy may allow detection of some osseous or ligamentous fractures, but at other times, spinal lesions are first suspected when the spine is misaligned, segments of the spine have increased mobility (when the head, neck, or torso is flexed/extended or rotated by the prosector), or when hematoma is visualized in the prevertebral or postvertebral musculature. A number of standardized measurements are routinely used in the radiologic assessment of spinal injuries (
Fig. 12.2), and similar principles can be developed and applied to the anatomic documentation of lesions. Different criteria for classifying spinal lesions exist. Lesions can be categorized by the type of injury, the motion producing the injury, or according to the anatomic location.
Classification of Vertebral Fractures
Compression fracture is the most common type of fracture, usually secondary to hyperflexion. The age of the individual and the degree of osteoporosis determines the amount of force necessary to produce this type of fracture. Compression fractures can result from minor trauma in older subjects, but require considerable force in the young. In the absence of disc displacement, these fractures are not usually accompanied by injury to the cord.
Burst fracture results from axial loading. Fragments of bone “explode” in all directions, including into the spinal canal, resulting in spinal cord injury with complete or incomplete paraplegia, depending on the severity of the spinal cord damage. Burst fractures are most common at the thoracolumbar junction.
Fracture/dislocation results from a complex force with flexion, extension, lateral bending, distraction, or torsion components. Usually the spine is misaligned either in the frontal or sagittal planes, and the spinal cord is injured, with resulting paraplegia.
Functional Classification of Spinal Injuries
Flexion injury produces an anterior collapse of the vertebral body that may be accompanied by displacement (with the risk of spinal cord injury). Depending on the degree of flexion, the posterior muscles and ligaments may distend and break, with the consequent hematoma of the fibers or frank hemarthrosis. Flexion dislocation produces complete transection of the posterior ligamentous complex and anterior subluxation of the vertebrae. It usually produces damage of the cervical spinal cord.
Extension injury results in a wide range of lesions, ranging from tears in the sternocleidomastoid to rupture of the longus colli or fracture of the anterior longitudinal ligament. It may be accompanied by fracture of the inferior articular surface. It usually does not produce neurologic damage except for injury of the spinal artery with the resulting central cord syndrome or when the disc herniates into the spinal canal. Older individuals are at higher risk of spinal cord injury after extension lesions because of the narrowing of the canal that occurs with aging. Individuals with developmental cervical stenosis may have a higher risk for injuries during cervical hyperextension, as infolding of the ligamentum flavum may decrease significantly the anteroposterior diameter of the spinal canal in 30% of subjects.
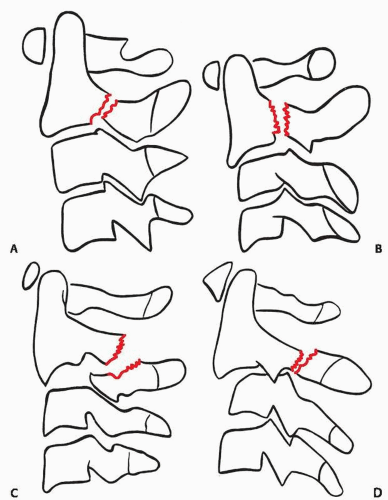
7 At autopsy, obvious hematoma in the retropharyngeal or prevertebral space is noted, and damage of the sympathetic fibers is usually present. Extension fracture with subluxation (hangman’s fracture, traumatic spondylolisthesis of C2) consists of the anterior displacement of the body and dens of C2 as a result of fracture of the C2 pedicles (
Fig. 12.3). A hangman fracture can also be caused by hyperflexionwith an axial loading component.
Axial compression injuries may result in endplate fractures, bowing of the end plate, or burst fractures, the latter usually accompanied by disc injuries and spinal cord damage. They may have an associated fracture of the vertebral arch. They are common at the cervicothoracic junction.
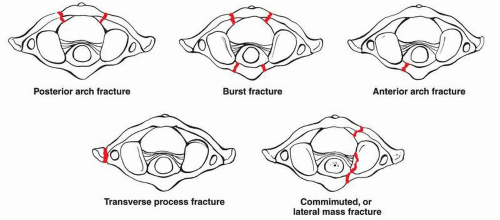
Jefferson fracture consists of fracture of the anterior and posterior arch of C1, with lateral displacement of the segments. It usually results from compression of the atlas between occipital bone and axis.
8
Anatomic Classification of Spinal Injuries
Upper Cervical Injuries (Occiput-C1 and C2)
Occipital condyle fractures are rare and can be associated with basilar skull fractures.
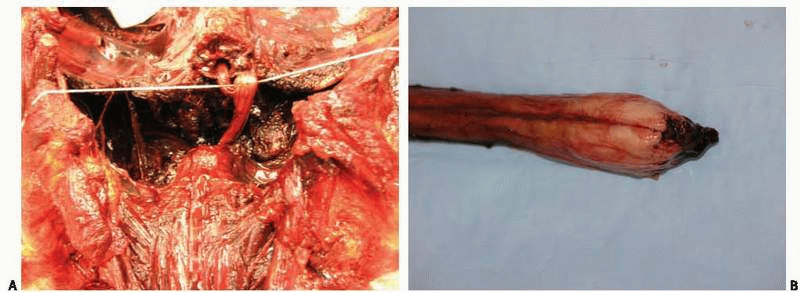
Occipitoatlantal dislocations are almost always fatal. They are produced by combined hyperextension and rotation. The occipital condyles can be displaced anteriorly or posteriorly or remain in line, but at a distance from the atlantoid facets (
Fig. 12.4). The temporal or permanent narrowing of the foramen magnum may result in contusions, lacerations, or transection of the cervicomedullary junction.
In isolation, fractures of the atlas usually do not have neurologic complications, (including Jefferson fracture) unless fragmented bones impinge into the cord (
Fig. 12.5). About half of these fractures are associated with other cervical fractures and may also be accompanied by vertebral artery injuries.
Transverse ligament fractures produce C1-C2 instability and may be associated with death. They are usually caused by hyperflexion of the upper neck.
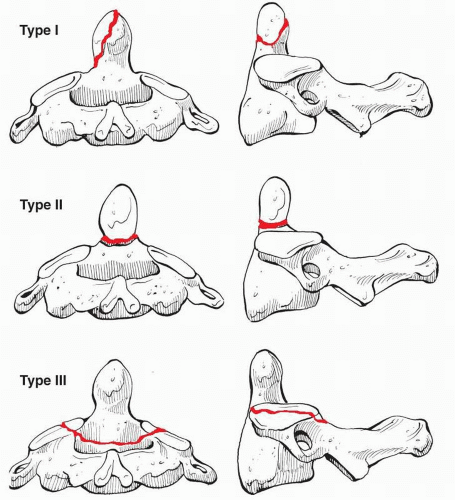
Odontoid fractures are relatively common in high-speed motor vehicle accidents. The severity of the injury depends on the degree of displacement of the dens into the canal.
Traumatic spondylolisthesis of C2 (hangman’s fracture) may be seen in high-speedmotor vehicle accidents or in high falls. There are several types; the most serious occurs when anterior displacement of C2 over C3 accompanies fracture of the neural arch (
Fig. 12.6).
Lower Cervical Injuries (C3 to C7)
Lower cervical injuries are seen in motor vehicle accidents, falls, diving accidents, and blunt force trauma.
Clay shoveler fracture is defined as avulsion of lower cervical/upper thoracic spinous process.
Sentinel fracture is defined as a fracture through either posterior lamina.
Ankylosing spondylitis is characterized by ossification of ligaments. These ossified ligaments are prone to fractures, and bone fragments have the potential to injure the spinal cord.
Thoracic and Lumbar Spine Injuries
Most of the fractures encountered in clinical studies involve the thoracolumbar spine. However, in autopsy studies
5 and in our own experience, mid-thoracic lesions are more common in forensic practice.
Classic seat-belt injuries result from forward flexion of the upper body over a lap belt during a high-speed collision. The resulting injury is due to forward translation of the spine, producing a Chance fracture or ligamentous disruption.


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access