, Jorn Fierstra2, Kees P. Braun1 and Luca Regli2
(1)
Department of Neurology and Neurosurgery, Brain Center Rudolf Magnus, UMC Utrecht, 85500, Utrecht, 3508 GA, The Netherlands
(2)
Department of Neurosurgery, University Hospital Zürich, Frauenklinikstrasse 10-CH-8091, Zürich, Switzerland
Abstract
Moyamoya vasculopathy (MMV) leads to chronic hypoperfusion predominantly in the middle cerebral artery (MCA) and anterior cerebral artery (ACA) territories. Most revascularization techniques focus on revascularization of the MCA territory. Augmentation of blood flow in the frontal area is important for neurocognition and lower extremity function. In this article we describe a new combined (direct and indirect) one-stage bypass technique consisting of a superficial temporal artery to middle cerebral artery (STA-MCA) bypass with encephalo-duro-synangiosis (EDS) for unilateral MCA revascularization, along with an encephalo-duro-periosteal-synangiosis (EDPS) for bifrontal blood flow augmentation. The strength of this technique is the revascularization of three vascular territories during a single surgical intervention: the MCA unilaterally; and the frontal territories bilaterally. Bifrontal EDPS may also be considered as a supplementary independent procedure for patients who previously underwent revascularization treatment in the MCA territory, but develop symptoms due to frontal hypoperfusion.
Keywords
Bilateral frontal territoriesBypass surgerySTA-MCA bypassIndirect revascularizationMoyamoyaNeurocognitionAbbreviations
ACA
Anterior cerebral artery
CBF
Cerebral blood flow
CVR
Cerebrovascular reserve
EDS
Encephalo-duro-synangiosis
EDMS
Encephalo-duro-myo-synangiosis
EMS
Encephalo-myo-synangiosis
EDPS
Encephalo-duro-periosteal-synangiosis
EPS
Encephalo-periosteal-synangiosis
[15O]H2O-PET
[15O]H2O-positron emission tomography
ICA
Internal carotid artery
IF
Interhemispheric fissure
MCA
Middle cerebral artery
MMD
Moyamoya disease
MMS
Moyamoya syndrome
MMV
Moyamoya vasculopathy
SSS
Superior sagittal sinus
STA
Superficial temporal artery
TIA
Transient ischemic attack
Introduction
Moyamoya disease (MMD) is a rare cerebrovascular disease of unknown etiology that is characterized by progressive bilateral stenosis of the intracranial internal carotid arteries (ICAs) and their proximal branches, resulting in cerebral hypoperfusion with subsequent ischemic symptoms or, less often, intracerebral hemorrhage [14, 21]. If moyamoya vasculopathy (MMV) is associated with other conditions (i.e., Down’s syndrome, neurofibromatosis type I), patients are diagnosed as having moyamoya syndrome (MMS) [21].
In MMV, reduced cerebral perfusion leads to compensatory development of collateral vasculature by small vessels near the apex of the carotid, on the cortical surface, leptomeninges, and branches of the external carotid artery supplying the dura and the skull base; these processes rarely involve the posterior circulation [22]. Surgical cerebral revascularization is considered to be the only effective treatment modality and can be achieved by direct, indirect or combined methods [1, 3, 14]. Direct techniques consist of an anastomosis of a donor artery, generally the superficial temporal artery (STA), to a cortical recipient arterial branch of the middle cerebral artery (MCA), which instantly augments blood supply. Indirect methods for cerebral revascularization are based on the approximation of vascularized tissue such as the temporal muscle, pericranium, dura or omentum onto the cortex in order to promote neoangiogenesis over time [1, 4]. Combined techniques provide the advantages of both methods; however, there is no evidence of one technique having advantages over the other [3]. Most techniques focus on revascularization of the MCA territory, yet revascularization in the frontal territory is gradually receiving more attention: part of the ischemic presentation of (pediatric) moyamoya patients consists of neurocognitive disorders as well as lower extremity function, caused by frontal hypoperfusion [2, 5, 12, 24]. Re-establishing cerebral blood flow (CBF) in the frontal territory may prevent, stabilize or improve neurocognitive decline [6, 7, 15, 17–20, 24].
In this paper, we describe a combined one-stage procedure for revascularization of the MCA territory unilaterally by a direct STA-MCA bypass and encephalo-duro-myo-synangiosis (EDMS) and the bifrontal territory by an encephalo-duro-periosteal-synangiosis (EDPS). To illustrate the procedure, the treatment of a girl affected by MMS is reported.
Materials and Methods
Illustrative Case
A 9-year-old girl affected by neurofibromatosis type I presented with multiple transient ischemic attacks (TIAs) consisting either of diplegia of the legs or monoparesis of the left arm, combined with frequent headaches. Neurological examination showed no deficits. Neuroimaging (MRI, MRA and DSA) demonstrated bilateral occlusion of the terminal ICA and the M1 and A1 segments, with bilateral typical compensatory moyamoya vessels. The patient was diagnosed as having MMS. An [15O]H2O-positron emission tomography ([15O]H2O-PET) scan documented extensive decreased baseline CBF in the right MCA and frontal area as well as severely impaired cerebrovascular reserve (CVR) in almost the entire right hemisphere after the administration of acetazolamide. Moderately decreased baseline CBF was seen in the left hemisphere, especially the frontal area, with well-preserved CVR in the MCA and posterior cerebral artery territory, but decreased frontal CVR (Fig. 1a, c). Based on the symptomatic course of the disease and the hemodynamic insufficiency, surgical revascularization was indicated and aimed at increasing the blood supply to the right MCA and frontal territories.
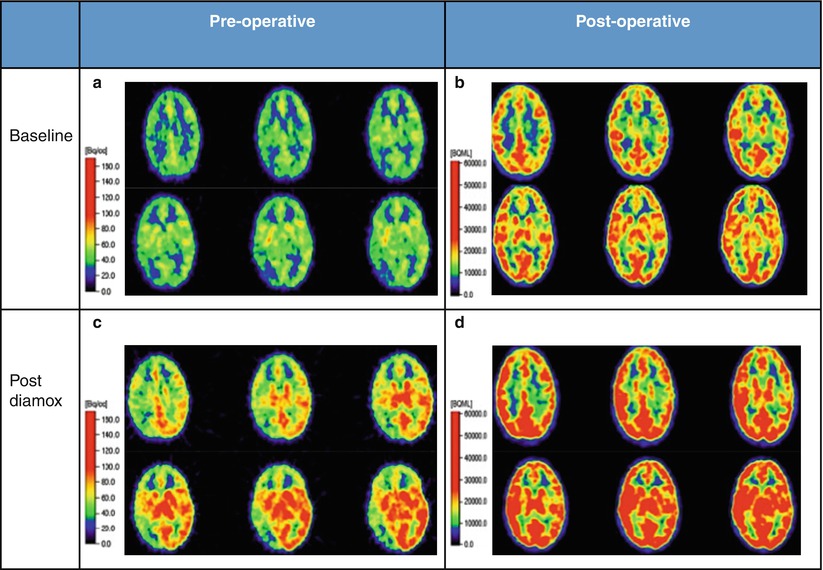
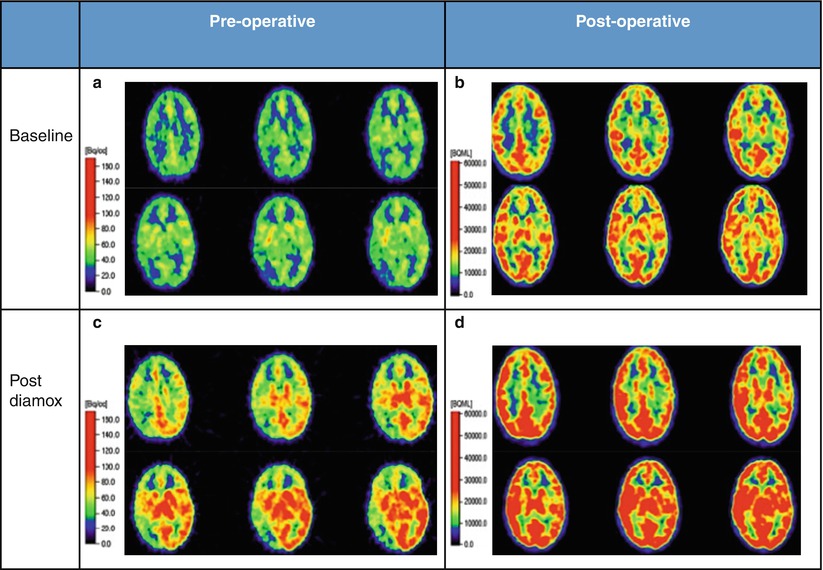
Fig. 1
(a, c) Pre-operative [15O]H2O-PET scan revealed severe baseline perfusion deficits and almost absent CVR after acetazolamide administration in almost the entire right hemisphere. Left hemispheric baseline CBF was moderately affected and CVR was largely preserved, with exception of the left frontal region. (b, d) One year and 8 months postoperatively, the [15O]H2O-PET revealed clear improvement of CVR in the right hemisphere and the left frontal regions. The non-operated left MCA territory showed decreased CVR compared to preoperatively
Combined Technique for Unilateral MCA and Bifrontal Revascularizazion
After general anesthesia, the patient was placed in the supine position with the head mildly extended and rotated 30° to the left in a Mayfield headrest. The first procedure step consisted of a right-sided STA-MCA bypass along with EMS. A linear incision located behind the hairline over the course of the STA was performed, without shaving the hair. The classic technique of an STA-MCA bypass was followed [9]. The parietal branch of the STA was dissected and the small branches arising from the STA were coagulated and cut. The donor vessel was kept intact until the anastomotic procedure was started. The temporal muscle was dissected and cut along the skin incision and a craniotomy was performed along the Sylvian fissure. The dura mater was thereafter carefully opened in a star fashion to maintain the main branches of the middle meningeal artery; dural flaps were reflected over the brain surface underneath the bone window and EDS was obtained by creating contact between the external surface of the dura and the brain surface. Afterwards, the cortex was surveyed for the largest cortical recipient artery. After identification of the most suitable recipient vessel, it was dissected by means of an arachnoid opening. A temporary non-traumatic microvascular clip was placed across the proximal exposed STA. A fish-mouth cut was then executed at the distal STA to increase the donor vessel’s opening diameter. The STA was passed through a small cut performed in the temporal muscle (in order to allow its intracranial entrance, with no risk of compression). A blue dye was put onto the surface of the cutting edges of the donor and recipient vessels to visualize the edges clearly during the anastomotic procedure. Non-traumatic microvascular clips were applied on the recipient vessel and two silicon triangle-shaped background sheets inserted beneath, in order to simplify the construction of the anastomosis. Thereafter, a linear arteriotomy on the cortical recipient vessel was performed. Two 10-0 monofilament sutures were used to anchor the donor and recipient vessel at the toe and the heel of the anastomotic site. The anastomosis was then completed by means of interrupted microsutures to allow eventual anastomosis growth with time. First the distal and then the proximal temporary clips on the cortical MCA recipient artery, and subsequently the clip on the proximal STA were removed. Verification of the bypass patency was performed by Indocyanine Green Videoangiography (performed by using a commercially available surgical microscope, OPMI® Pentero™, The Carl Zeiss Co., Oberkochen, Germany). Bidirectional flow through the MCA was assessed and all flows were quantified (18 ml/min) using a flow probe (Transonic system, Inc.© Ithaca, NY, USA). After establishing the bypass, EMS was performed. The previously made burr hole was enlarged to permit the intracranial entrance of the bypass without risk of compression, and the bone was returned to its normal position and secured in place.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








