CHAPTER 24
Cerebrospinal Fluid Examination
Analysis of the cerebrospinal fluid (CSF) can provide useful diagnostic information. As noted in Chapter 6, CSF is usually obtained from the lumbar subarachnoid space via a spinal tap, also called a lumbar puncture. Usually, this is carried out at the L3-4 or L4-5 interspace, with the patient in the lateral decubitus position. In some cases, it is easier to perform lumbar puncture with the patient in a sitting position. Because the spinal cord in adults ends at the L1-2 level, lumbar puncture can be performed below that level (and above the sacrum) without injuring the cord.
INDICATIONS
There are several indications for lumbar puncture:
(1) To verify suspected infection of the central nervous system (meningitis, encephalitis).
(2) To determine whether there is hemorrhage within the central nervous system, that is, for the diagnosis of subarachnoid hemorrhage if there is a high index of suspicion on clinical grounds and when computed tomography scanning is negative or unavailable.
(3) To examine the chemical and immunologic profile of the CSF to aid the diagnosis of disorders such as multiple sclerosis.
(4) To obtain cells for cytologic examination when carcinomatous meningitis (seeding of the meninges with neoplastic cells) is a diagnostic possibility.
The diagnosis of bacterial meningitis is a medical emergency. Untreated bacterial meningitis is almost always fatal, and the outcome of meningitis after treatment is much better if diagnosis is made and the patient is treated early in the clinical course. Similarly, early recognition and management of subarachnoid hemorrhage are high priorities, because rebleeding and vasospasm commonly occur and can lead to worsening or death, unless appropriate therapy is instituted.
CONTRAINDICATIONS
Several important contraindications to lumbar puncture exist:
(1) In patients in whom there is increased intracranial pressure—or when there is the possibility of an intracranial mass, especially in the posterior fossa—spinal puncture must be done extremely carefully or not at all. This is because shifts in CSF dynamics, as a result of lumbar puncture, can precipitate herniation of the tonsils of the cerebellum through the foramen magnum, with resultant compression of the medulla. Thus, in patients with suspected intracranial mass lesions, or in those in whom there is papilledema, lumbar puncture should be deferred until imaging has ruled out incipient herniation or a neurologist or neurosurgeon has been consulted.
(2) Infection (or suspected infection) at the site of lumbar puncture constitutes a contraindication because the needle can introduce the organism into the underlying subarachnoid space. Suspected epidural abscess at the puncture site is thus a contraindication.
(3) Coagulation disorders in patients with thrombocytopenia, hemophilia, vitamin K deficiency, and so forth can be followed by subdural or epidural bleeding at the site of lumbar puncture. Lumbar puncture under these circumstances should be performed only if the possible benefits outweigh the risks and then only after the coagulation disorder has been corrected, if possible.
ANALYSIS OF THE CSF
The manometric pressure of the CSF is measured at the beginning and at the end of the procedure. With the patient in the lateral decubitus position, the opening pressure of the CSF is normally 70 to 200 mm H2O. If lumbar puncture is performed with the patient in the sitting position, the CSF usually rises in the manometer to about the level of the foramen magnum but not higher. If the patient coughs, sneezes, or strains during lumbar puncture, there is usually a prompt rise in CSF pressure because of congestion of spinal veins and resultant increased pressure of the contents of the subarachnoid epidural spaces; the CSF pressure subsequently falls to the previous level.
After determination of the initial CSF pressure, four tubes of CSF are withdrawn (usually containing 2-3 mL each) under sterile conditions. Routine CSF examination usually includes cell counts, measurement of total protein, glucose, and gamma globulin levels. Cells are usually cultured, and, when appropriate, spinal fluid electrophoresis is performed to determine whether there are oligoclonal bands. (These are present in a variety of inflammatory disorders, most notably multiple sclerosis but also neurosyphilis, subacute sclerosing panencephalitis, and some cases of viral encephalitis.)
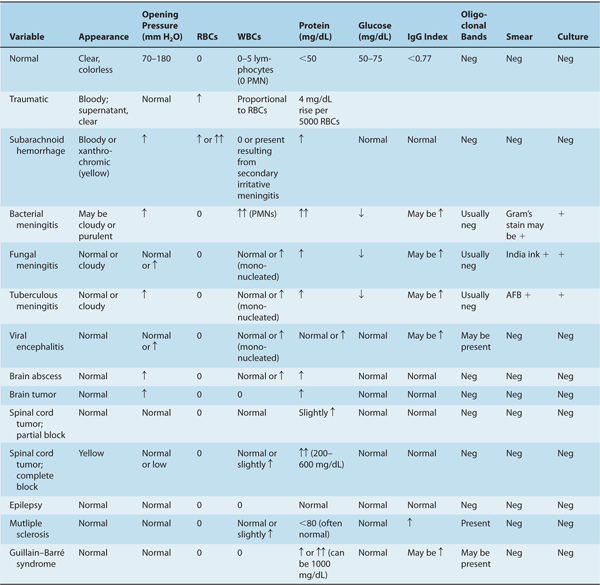
Table 24–1 illustrates the profile of the CSF after lumbar puncture in a number of neurologic disorders.
TABLE 24–1 Characteristic Cerebrospinal Fluid Profiles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








