Cerebrovascular Disorders
Cesar C. Santos
Harvey B. Sarnat
E. Steve Roach
Cerebrovascular disorders are now frequently recognized in children, probably because of increased awareness of these conditions by clinicians; the widespread application of noninvasive diagnostic studies such as magnetic resonance imaging (MRI), magnetic resonance angiography (MRA), computed tomography (CT); and, in the neonate, cranial ultrasound studies (1). These studies allow confirmation of a diagnosis that in previous years would have been missed or at least not recognized as a vascular lesion. Additionally, the number of children who develop cerebrovascular lesions from certain risk factors may have increased, as more effective treatments for some causes of stroke have allowed patients to survive long enough to develop vascular complications.
The most important distinction between cerebrovascular diseases in children and those of adults is the variety of conditions that cause stroke in children versus adults (Table 13.1) (1,2). Congenital heart disease and sickle cell disease, for example, are common causes of ischemic stroke in children, while atherosclerosis is rare in children. Treatment of the risk factors is essential if subsequent strokes are to be prevented, and it is sometimes the underlying condition that determines the patient’s outcome.
Recent advances in diagnosis notwithstanding, cerebrovascular lesions are often more difficult to diagnose in children, particularly in very young children who are unable to adequately describe their symptoms and who are sometimes less cooperative during an examination. Once the diagnosis is considered, however, these difficulties can usually be solved with careful observation and diagnostic studies.
STROKE
Incidence
Schoenberg and colleagues studied the incidence of cerebrovascular disease in the children of Rochester, Minnesota, from 1965 through 1974 (3,4). Excluding strokes related to birth, intracranial infection, and trauma, they identified three hemorrhagic strokes and one ischemic stroke in a risk population of 15,834, for an estimated annual incidence of 1.89/100,000/year and 0.63/100,000/year for hemorrhagic and ischemic strokes, respectively. The overall average annual incidence for children through 14 years of age in this study was 2.52/100,000/year. In this well-defined population, hemorrhagic strokes were seen more commonly than ischemic strokes, while in the Mayo Clinic referral population, ischemic strokes were more common. Several years later, Broderick and coworkers found a similar 2.7 pediatric stroke cases/100,000/year (5).
These earlier estimates may be low. One report on the incidence of vascular disease in Dijon, France, between the years 1985 and 1993 found childhood stroke in 13.0/100,000 children/year (6). Stroke is among the top ten causes of death in children in the United States (7), and the 1998 estimated mortality rate from stroke in children below one year of age was 7.8/100,000 children (7). The risk of stroke seems to be particularly high among neonates, patients who were not included in the earlier surveys. Cerebral ischemic infarction is recognized in 12% to 14% of neonates with seizures (8), and neonates comprise one-fourth of all childhood strokes (9). Data from the National Hospital Discharge Survey conducted from 1980 through 1998 indicate a stroke rate during the first month of life of 26.4/100,000; hemorrhagic stroke occurred in 6.7/100,000 and ischemic stroke occurred in 17.8/100,000. Based on these numbers, stroke in neonates occur in approximately 1 per 4,000 live births per year (10).
Clinical Manifestations
The clinical presentation depends on the child’s age, the presence of underlying risk factors, the location of the lesion, and the type of stroke. The diagnosis of stroke is often missed or delayed in children. In one retrospective study of children with stroke, the average time from the onset of symptoms until diagnosis was 35.7 hours (11). Some neonates initially appear normal but neurological impairment is recognized months later after they develop premature handedness or delayed milestones (12). In general,
stroke occurs more often in boys and in African American children, even after adjusting for trauma and for sickle cell disease (12,13).
stroke occurs more often in boys and in African American children, even after adjusting for trauma and for sickle cell disease (12,13).
TABLE 13.1 Risk Factors for Pediatric Stroke1 | ||
|---|---|---|
|
Ischemic Infarction
It is often impossible to determine whether an ischemic infarction has resulted from an embolism or a thrombosis on purely clinical grounds. Sudden-onset symptoms suggest an embolism, but the precise onset of the symptoms is often unknown, especially in very young children. Specific risk factors sometimes suggest whether the stroke has resulted from an embolus or a thrombus. Cardiac disease, for example, results in embolism more often than thrombosis, while the presence of cerebral arteritis would favor thrombosis.
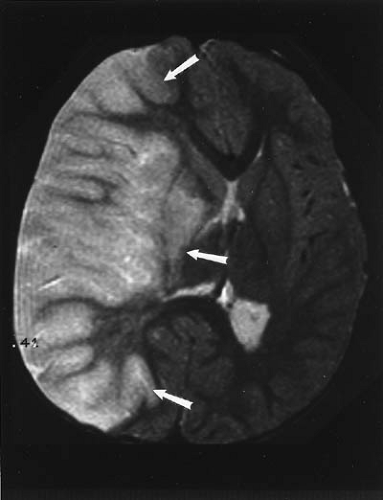 FIGURE 13.1. An MRI showing an acute embolic infarction (arrows) of most of the right cerebral hemisphere with mass effect. |
The specific signs and symptoms of an ischemic infarction depend on the size and location of the lesion. The anterior circulation is affected more often than the vertebrobasilar system. The basal ganglia and thalamus are together the most frequent location for ischemic infarction in children (Fig. 13.1) (14). An infarction in this region results directly from occlusion of the small penetrating arteries that supply this area, but in many cases, an ipsilateral carotid or middle cerebral artery is occluded. Infarction in these individuals is limited to the basal ganglia because this area lacks the collateral blood flow that rescues the nearby cortex. Because the vessels most often occluded are the supraclinoid internal carotid arteries and the branches of the middle cerebral arteries, typical signs include hemiparesis, hemianesthesia, and aphasia. However, a wide array of signs and symptoms are possible depending on the area of the brain affected. Hemichorea also has been described in children with basal ganglia infarction (15). Epileptic seizures are common. In one report of 43 children from 1 to 16 years of age, the most common presenting symptom was weakness followed by seizures (16). Acute ataxia and other cerebellar and brain stem findings occur in patients with a posterior circulation infarction.
Neonatal Infarction
Although not nearly as common as the germinal matrix hemorrhage in premature patients, ischemic infarction in term neonates may occur more often than previously suspected (see Chapter 6). The infarction typically occurs in a term baby after an uneventful pregnancy and a routine delivery. The infarction is often identified after the onset of focal seizures, and most of the time, the physical findings are nonspecific with only mild lethargy, irritability, hypotonia, or subtle hemiparesis. Focal motor seizures more often involve the right body because about three-fourths of single infarcts occur in the left cerebral hemisphere. The initial radiographic appearance of the lesion sometimes suggests that the infarction occurred even before birth. Some babies with cerebral infarction are probably missed because the findings are often subtle, and not all babies develop seizures. Similar lesions of long-standing duration are sometimes discovered in older children who are being evaluated for epileptic seizures or developmental delay.
Most neonatal infarctions probably result from emboli. Systemic emboli can occasionally be demonstrated in these neonates, and the left hemisphere predominance is more easily explainable by embolic than by thrombotic infarction. Interruption of aortic laminar flow by blood from the still patent ductus arteriosus might explain emboli being preferentially directed to the left hemisphere. The source of the emboli is not known with certainty, but they may arise from degenerating placental vessels or the just-activated pulmonary vascular bed.
Watershed infarcts are frequent in the neonate. Two patterns are found. The first is similar to watershed infarcts in the adult, in areas between the territories of the anterior and middle cerebral arteries and between the middle and posterior cerebral arteries. The difference from adults is that in term neonates, about one-third of such supratentorial watershed infarcts are hemorrhagic, whereas in the adult nearly all are ischemic infarcts without hemorrhage. In preterm infants of less than 35 weeks gestation, two-thirds of cerebral cortical watershed infarcts are hemorrhagic, so that there is a shift in watershed infarcts toward coagulation necrosis as the brain matures. The second pattern is that of symmetrical tegmental infarcts in the brainstem. They involve the superior and inferior colliculi and tegmentum of the midbrain, pons, and medulla oblongata near the floor of the fourth ventricle. This tegmental watershed zone is between the territories of the paramedian penetrating arteries and the long circumferential arteries, both arising on each side from the basilar artery as a series of 25 to 30 sets, hence the infarction as a longitudinal column. Because tegmental structures in this zone include the fasciculus and nucleus solitarius (central “pneumotaxic” center of respiratory drive) and the nucleus ambiguous (somatic vagal component of muscles of deglutition), clinical manifestations include lack of central respiratory drive and dysphagia, in addition to multiple
cranial neuropathies, Möbius syndrome, and sometimes micrognathia and ankylosis of the jaw because of infarction including the motor trigeminal nucleus (16a) (see Chapter 5).
cranial neuropathies, Möbius syndrome, and sometimes micrognathia and ankylosis of the jaw because of infarction including the motor trigeminal nucleus (16a) (see Chapter 5).
Venous Occlusion
Cortical vein and dural sinus thrombosis can be difficult to recognize because the clinical findings are sometimes less dramatic than those of arterial occlusion. Focal or generalized seizures are common with cortical vein thrombosis, and dural sinus thrombosis often leads to increased intracranial pressure. In the face of seizures, focal neurological dysfunction due to sinovenous occlusion is easily mistaken for postictal deficit. Venous occlusion is frequently associated with a nearby infection such as chronic otitis, sinusitis, or orbital cellulitis; it also is seen in children with hemoglobinopathy, congestive heart failure, polycythemia, and dehydration.
Etiology
The risk factors for stroke in children (Table 13.1) are different from those of adults, although there is some overlap (1,2). Even after a thorough diagnostic evaluation, about one-fourth of children with ischemic infarction have no obvious cause for stroke, and others have suspected risk factors that may or may not explain the infarction. On the other hand, a likely cause for intracranial hemorrhage is usually found after a complete evaluation, including a cerebral angiogram.
Cardiac Disorders
The most common cause of ischemic infarction in children is congenital or acquired heart disease (17), although the likelihood of stroke due to heart disease seems to have decreased in recent years as newer and more effective treatments have become available. In the Canadian Pediatric Ischemic Stroke Registry, cardiac disease occurred in 24% of children with arterial stroke, and stroke in 20% and 17% of cases following cardiac surgery and catheterization, respectively. Complex cardiac anomalies are by far the biggest problem, but any cardiac lesion can lead to stroke. Particularly concerning are the cyanotic cardiac lesions associated with polycythemia, which increase the risk of both thrombosis and embolism. If a right-to-left cardiac shunt is present, a venous (paradoxical) embolus can bypass the pulmonary circulation and reach the brain. Many patients are already known to have heart disease prior to stroke, but in other instances, a less obvious cardiac lesion is discovered only after stroke. Surgical correction of congenital heart disease decreases the risk of stroke, although risk of embolism in these children remains higher than normal. Rheumatic valvular heart disease and other acquired cardiac conditions are known to cause stroke in children. Some children with congenital heart disease seem to have an increased risk for intracranial aneurysms and arterial dissection (18). Cerebral embolism has been reported in patients with cardiac rhabdomyomas, atrial myxomas, and primary cardiac lymphomas (19,20,21).
Hematological Disorders
Although stroke is occasionally linked to other hemoglobinopathies and to sickle cell trait, homozygous sickle cell disease (SCD) accounts for most of the individuals with stroke. The cumulative risk of having stroke increases with age: 11% by age 20, 15% by age 30, and 24% by age 45 (22). Moreover, after the first sickle cell–related stroke, that individual’s risk of having a second stroke soars to over 50%. Stroke accounts for 12% of deaths in individuals with sickle cell disease (23). Most sickle cell–related strokes are ischemic, but both intraparenchymal and subarachnoid hemorrhages occur. Stroke is somewhat more likely during a thrombotic crisis, but most of the time, an infarction occurs in an otherwise asymptomatic individual. Silent infarction, evident with MRI in an individual without an obvious neurologic deficit, occurs in 22% of children with homozygous SCD (24). See Chapter 17.
Although both large and small cerebral arteries are affected by SCD, the distal internal carotid arteries and their immediate branches are usually involved (25,26). Elevated cerebral blood flow velocity measured by transcranial Doppler (TCD) predicts a much higher stroke risk due to SCD. A randomized multicenter controlled study (the STOP trial) compared prophylactic blood transfusion with standard medical care in individuals at high risk for stroke based on TCD measurements (27). This study showed conclusively that the time-averaged mean blood flow velocity measured by TCD indicates a higher stroke risk due to SCD and demonstrated that prophylactic blood transfusion reduces the occurrence of first stroke by over 90% (28,29). The neurologic complications of sickle cell disease and the other hemoglobinopathies are further discussed in Chapter 17.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








