CHAPTER 293 Cervical Arthroplasty
Evolution of Cervical Arthroplasty
Anterior cervical diskectomy with fusion (ACDF) has been the “gold standard” treatment of central and paracentral herniated cervical disks for decades. Significant advances such as plated fixation have contributed to the increasingly high fusion rates of ACDF since Cloward first described this technique in 1958.1 Fusion rates, already greater than 90% with allograft and anterior cervical plate fixation, now approach rates of 100% with the use of synthetic interbody grafts such as polyetheretherketone (PEEK) and recombinant human bone morphogenetic protein-2 (rhBMP-2).2 In the setting of such a successful operation, one must thoroughly investigate what if any role arthroplasty should play as an alternative to arthrodesis.
During the past decade, ACDF has been found to be associated with symptomatic adjacent-segment disease.3–5 Hilibrand and colleagues reported that the adjacent-segment reoperation rate after ACDF was 2.9% annually. Furthermore, 10 years after ACDF, 25% of patients reported symptoms caused by adjacent-segment disease.3–5 Likewise, Goffin and coauthors reported that 92% of postoperative ACDF patients had radiographic evidence of adjacent-segment degenerative disk disease at 5 years.6 This adjacent-segment degeneration may be related both to the natural history of cervical spondylosis and to the biomechanical effects of fusion on the adjacent level. Matsunaga and colleagues have discussed higher shear strain occurring at levels adjacent to anterior cervical fusions.7 It has been postulated that cervical disk arthroplasty might reduce the incidence of this shear strain by providing motion more similar to normal neck mobility.8–10
The earliest attempts to replace the cervical intervertebral disk with a prosthetic device began in the 1960s.11 In the last decade, there has been significant growth in the enthusiasm for cervical disk arthroplasty, with early designs of these implants modeled on artificial joints implanted in the knees, hips, and shoulders.
Nomenclature of Cervical Arthroplasty
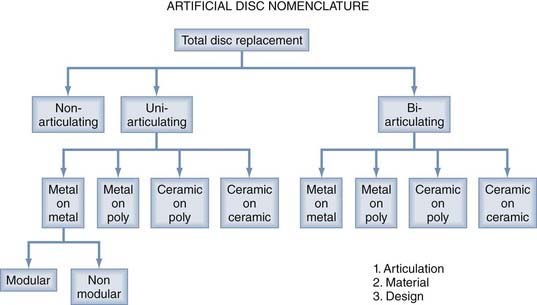
In the 1990s, numerous new-generation artificial disks were developed. To better understand the differences between evolving generations of artificial cervical disks, the Cervical Spine Study Group developed a new nomenclature system for cervical arthroplasty. They classified artificial disks into three types: nonarticulating, uniarticulating, and biarticulating. The implant concepts included a metal-on-metal design, a metal-on-polymer (e.g., ultrahigh-molecular-weight polyethylene), a ceramic-on-polymer design, and a ceramic-on-ceramic design. These prostheses can be either modular (having replaceable components) or nonmodular (lacking replaceable components). Some are fixated with supplemental vertebral body screw, whereas others are not. In addition, some disk arthroplasty devices promote biologic bone ingrowth at the disk–end plate interface. These implants may be constrained in terms of motion, or they may be semiconstrained or unconstrained. As such, classification is based on the following criteria: articulation, material, design, fixation, and kinematics (Fig. 293-1).
Clinical Trials
European, Australian, and American clinical trials have reported excellent results when using the metal-on-metal and metal-on-polymer disks as opposed to ACDF. These results were based on Neck Disability Index (NDI) and arm pain intensity visual analogue scale (VAS) scores, as well as neurological status.10,12–16 Thus far, excessive metal debris, material fatigue/fracture, and catastrophic failure have not been problematic in these trials. These trials appear to suggest that the advantages of maintenance of motion and the potential improved clinical outcome of arthroplasty outweigh the putative disadvantages of wear debris, material fatigue, and joint failure. In the United Sates, several artificial disks are undergoing prospective, randomized clinical trials (Food and Drug Administration Investigational Device Exemption [FDA IDE] Trial) in which outcomes are being compared with ACDF. Several trials have been completed (the Prestige ST Artificial Disc, Bryan Artificial Disc, and ProDisc-C).
In 2007, we reported the 2-year clinical and radiographic outcomes of a prospective randomized trial comparing ACDF and arthroplasty with the Prestige ST Cervical Disc (Figs. 293-2 to 293-4). Five-hundred-forty-one patients with single-level cervical degenerative disk disease and radiculopathy were randomly assigned to one of two treatment groups: arthroplasty with the Prestige ST or a control group treated by ACDF. Eighty percent of the arthroplasty-treated patients and 75% of the control patients reached 2 years of follow-up at the time of publication, and further follow-up is still ongoing. The NDI score and the Short Form Health Survey (36 items) (SF-36) score improved in both groups. However, the arthroplasty group had a statistically significant higher rate of neurological success, as well as a lower rate of secondary revision surgeries and supplemental fixation than did the ACDF group. The cervical disk arthroplasties maintained segmental sagittal angular motion averaging greater than 7 degrees (see Fig. 293-3). It is important to note that there were no cases of implant failure or migration in the arthroplasty group.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree