Cervical Orthoses and Cranioskeletal Traction
Mark S. Eskander
Dahari D. Brooks
The earliest use of cervical orthoses comes from the fifth Egyptian dynasty (2750 to 2625 BC) (1). The biomechanical principles can be traced back to the devices used by Hippocrates (1). Currently, many types of cervical orthoses are available. They are sometimes named for their inventors (e.g., Benjamin-Taylor, Thomas, Guilford) or where they were designed (e.g., Philadelphia, Yale, Miami) or simply a description of the brace (e.g., four-poster, two-poster, sternooccipital mandibular immobilizer [SOMI]).
Cervical spinal orthoses are externally applied devices used to restrict motion cervical spine. These orthoses are applied to the soft tissue envelope of the head, neck, and chest and transmit forces to the bony structures. There are two main types of orthoses: cervical orthoses and cervicothoracic orthoses. Cervical orthoses are applied to the head and neck region and cervicothoracic orthoses extend from the head, neck, and upper chest. Cervical orthoses can be used in the treatment of cervical trauma, pain, and instability and in providing the postoperative setting (2).
New materials/designs have led to better braces. Thermoplastic braces are lighter than some of the earlier designs. This has helped maintain comfort and subsequently patient compliance. Also, many of the newer braces are compatible with magnetic resonance imaging (MRI). As with any new orthopaedic device, clinical trials need to be undertaken in order to fully understand when and how these braces should be used.
Each orthoses may vary widely in terms of motion restriction, comfort, and versatility. Often, when prescribing an orthosis, one must choose based on the type of instability and the level of compliance that is required. This chapter focuses on the some commonly used cervical orthoses and reviews the appropriate clinical uses of cervical orthosis.
CERVICAL BIOMECHANICS
Cervical motion has been described as having six degrees of freedom (translation and rotation in the x-, y-, and z-planes). Clinically, cervical motion is broken down into flexion-extension, lateral bending, and rotation (3). Range of motion in the cervical spine is a complex interplay between the bony and soft tissue structures. Kottke and Mundale (4) evaluated cervical motion in a normal population and reported the following averages: flexion, 70 degrees ± 10 degrees; lateral bending in each direction, 45 degrees ± 10 degrees; and axial rotation in each direction, 75 degrees ± 10 degrees. Perry and Nickel (5) described the normal arc of cervical motion to be 145 degrees of flexion-extension, 180 degrees of axial rotation, and 90 degrees of lateral flexion. Bhalla and Simmons (6) reported that the C4-C5 articulation demonstrated the greatest range of motion, whereas Kottke and Mundale (4) recorded the most mobility at C5-C6. Using cineradiography, Fielding (7) noted that flexion caused a slight ventral translation of the upper cervical vertebral bodies, whereas extension resulted in dorsal translation.
SPINAL MOBILITY WITH CERVICAL ORTHOTICS
In 1960, Jones (8) used cineradiography to qualitatively examine the motion of normal subjects wearing soft and rigid collars. Although specific measurements were not made, he concluded that rigid collars restricted motion more than soft collars, but all the collars allowed substantial motion of the cervical spine.
Subsequently, many studies have attempted to measure cervical motion in orthotics. Both goniometry (9, 10, 11 and 12) and radiography (7, 8 and 9,13, 14 and 15) have been used to measure cervical motion in normal subjects, cadavers, and mannequins. Fisher et al. (9) measured cervical motion using both goniometry and radiography and concluded that goniometry provided an adequate clinical tool to assess the overall motion of the cervical spine in the sagittal plane. Most cervical orthoses restrict more flexion-extension than lateral bending or axial rotation (3,9,10,14,16,17).
Fisher et al. (9) studied the cervical motion with the Camp collar, Philadelphia collar, four-poster brace, and the SOMI brace in normal subjects using lateral radiographs. The SOMI brace provided the best restriction to
flexion of the upper cervical spine. The four-poster brace provided the best immobilization of the middle and lower cervical spine. The Philadelphia collar was rated as most comfortable but was the least effective at immobilizing all levels, especially the occiput to C2 region. The Camp collar provided the best immobilization of the C1 to C2 but was uncomfortable (9,18).
flexion of the upper cervical spine. The four-poster brace provided the best immobilization of the middle and lower cervical spine. The Philadelphia collar was rated as most comfortable but was the least effective at immobilizing all levels, especially the occiput to C2 region. The Camp collar provided the best immobilization of the C1 to C2 but was uncomfortable (9,18).
Johnson et al. (17) evaluated normal subjects with the soft collar, Philadelphia collar, four-poster brace, cervicothoracic brace, and SOMI brace by using radiography and photographs. Also, the halo vest orthosis was evaluated in patients following cervical surgery or cervical trauma. The flexion-extension stability (most to least) is as follows: halo, cervicothoracic brace, four-poster brace, SOMI and Philadelphia collar (equal), and soft collar. Only the halo orthoses controlled flexion-extension of the occiput through C2 region. The halo provided the best immobilization of all cervical levels. The SOMI orthosis effectively limited C1-C2 flexion (but not extension) and thus was recommended for isolated atlantoaxial flexion instability. Notion between the occiput and C1 was noted to be increased by the use of a cervical collar.
Kaufman et al. (10) measured cervical motion normal subjects wearing the Philadelphia collar, NecLoc collar, and the soft collar. The NecLoc collar was the most effective, limiting flexion-extension by 62%, lateral bending by 43%, and axial rotation by 62%. In contrast, the Philadelphia collar limited flexion-extension by 46%, lateral flexion by 25%, and axial rotation by 29%.
In a similar study, Beavis (16) measured cervical motion in normal subjects wearing a soft collar, hard collar, Plastazote collar, and a custom-fit collar. Motion was restricted most by the Plastazote collar, followed by the custom collar and hard collar. Soft collars provided minimal motion restriction.
Podolsky et al. (13) evaluated methods of cervical immobilization during trauma extrication and transport. The soft collar, hard collar, Philadelphia collar, extrication collar, bilateral sandbags with tape, and Philadelphia collar combined with sandbags and tape were tested in normal volunteers. Sandbags and tape provided excellent motion restriction except in extension. The addition of the Philadelphia collar helped to further limit extension when combined with sandbags and tape.
Lunsford et al. (11) measured cervical motion and skin contact pressure in ten normal subjects wearing the Philadelphia collar, Miami J collar, Malibu collar, and Newport Extended Wear collar (Aspen collar). The Malibu collar provided the best immobilization, restricting lateral bending by 41%, extension by 40%, flexion by 57%, and axial rotation by 61%.
Koch and Nickel (19) evaluated cervical spine mobility in the halo orthosis. Lateral radiographs in various positions were taken of six patients treated in a halo cast for unstable cervical injuries. In addition, compression and traction forces were measured through the upright connectors attaching the halo ring to the cast. Snaking of the cervical vertebrae was noted, with some spinal segments assuming a flexed posture and other regions assuming an extended posture. C4-C5 experienced the greatest mobility, which averaged 7.2 degrees. C2-C3 had the highest percentage of normal motion (42% of normal motion). Forces measured at the halo uprights varied widely, from 5 pounds compression to 17 pounds traction. These forces were noted to change dramatically with changes in position or when patients abducted their arms. Neck distraction changed by an average of 3.6 mm with changes in position.
Anderson et al. (20) measured cervical motion using radiographs in 42 patients immobilized in a halo vest for injuries of the cervical spine. Lateral radiographs were taken in supine and upright positions within 5 days of injury. Noninjured levels demonstrated an average 3.9 degrees of angulation, with the greatest motion occurring between the occiput and C1 (8.0 degrees). Injured levels demonstrated an average sagittal plane angulation of 7.0 degrees and translation of 1.7 mm. Fracture site motion greater than 3 degrees of angulation or 1 mm of translation was observed at 77% of the injured levels. The authors recommended obtaining lateral radiographs in both a supine and upright position when treating unstable cervical injuries in a halo so that injuries demonstrating excess motion could be detected and treated by an alternative method.
Alberts et al. studied the Nebraska collar and compared it with the Philadelphia collar, SOMI, and the Lehrman-Minerva cervical orthosis. Flexion, extension, lateral bending, and rotation limits were tested. The Nebraska collar restricted rotation and lateral bending most significantly. In regard to the maximum extension from occiput to C7, the Nebraska collar was more restrictive than the Philadelphia collar or the SOMI. In terms of flexion, there was no significant difference among the collars. During total flexion-extension motion testing, the Nebraska and Lehrman-Minerva cervical collars were more restrictive than the Philadelphia collar (21).
ORTHOSIS COMFORT
Forces used to control the spine are applied to the surrounding soft tissues of the neck. Individual anatomy, flexibility, and soft tissue envelope will vary, thereby altering orthosis fit and efficacy. Therefore, a cervical orthosis should be carefully matched to the patient’s anatomy. Ideally, the contact area should be maximized to minimize pressure points. Soft materials should be used at the sites of skin contact. Breathable materials and extra pads should be used to minimize perspiration with the orthosis. Compliance with the treatment plan is correlated with the level of comfort while in the brace.
Skin breakdown due to elevated contact pressures beneath an orthosis remains a significant risk. The risk of skin breakdown can be decreased by trimming or shaving hair beneath the brace and maintaining good skin hygiene. Frequent inspection of skin contact areas is mandatory when using an orthosis for patients with altered sensory function or elderly/frail patients. Most patients can be successfully fitted with off-the-shelf orthoses. On occasion, a custom-made orthosis is necessary to accommodate some patients. With thermoplastics, custom fabrication is a rapid process.
Fisher (18) measured skin contact pressures and cervical motion in eight adults fitted with the SOMI brace. Skin contact pressures were noted to be well in excess of the
capillary closing pressure (CCP) with the brace applied in the “usual” fashion. When the braces were refitted to keep the contact pressures at 20 mm Hg (below CCP), there was no substantial increase in the cervical range of motion noted. The authors concluded that with the use of pressure sensors, a cervical orthosis could be applied with less pressure, thus minimizing patient discomfort and lowering the risk of skin breakdown while maintaining an acceptable level of immobilization.
capillary closing pressure (CCP) with the brace applied in the “usual” fashion. When the braces were refitted to keep the contact pressures at 20 mm Hg (below CCP), there was no substantial increase in the cervical range of motion noted. The authors concluded that with the use of pressure sensors, a cervical orthosis could be applied with less pressure, thus minimizing patient discomfort and lowering the risk of skin breakdown while maintaining an acceptable level of immobilization.
Plaisier et al. (12) measured craniofacial pressures and subjective comfort in 20 normal volunteers wearing the Stifneck collar, Philadelphia collar, Miami J collar, and Newport collar (Aspen collar) in the upright and supine positions. The Stifneck collar exceeded CCP in both the upright and supine positions, while the Philadelphia collar exceeded CCP in the supine position. In contrast, the Aspen and Miami J collars were noted to exert pressures below the CCP in both positions. The Aspen and Miami J collars were rated as comfortable, whereas the Stifneck collar was uncomfortable.
Unstable cervical conditions often require the use of a cervical orthosis during bathing. In this setting, it is useful to provide the patient with a second cervical collar made of Plastazote material, such as the Philadelphia collar.
When a rigid cervical orthosis is no longer required, a weaning should ensue. This allows the patient a chance to gradually regain normal muscle strength and proprioception. Also, it can lessen the psychological fear that patients have in removing their brace. A schedule of decreasing brace wear can be combined with the use of a soft collar and physical therapy to hasten the return of physiologic neck mobility.
Many patients identify comfort not only with the fit but also with their ease of performing their daily activities. Chin et al. found that segmental spinal motion in cervical orthoses can be caused by mastication. Seven volunteers received 5 seconds of continuous lateral cervical fluoroscopic imaging while chewing gum, without any cervical orthosis and while wearing a soft collar turned forward then backward, a Philadelphia collar, a Miami J collar, or a two-poster brace. All cervical collars produced statistically greater motion at the levels of occiput-C1 and C1-C2 versus no collar. Motion was greatest at the occiput-C1 junction and then decreased downstream to the C4 level. No motion was detected in any subject in any brace below C4. The two-poster brace produced the most segmental motion at occiput-C1 (6.3 ± 2.0 degrees) compared with the soft collar turned backward (1.9 ± 1.9 degrees). None of the subjects experienced segmental motion below C2 in the soft collar. Without a cervical brace, no segmental spinal motion was observed. In order to limit upper cervical spine segmental motion during mastication (for patients with unstable cervical spines), we recommend a two-poster brace with removal of the mandibular component allowing for free mandibular action. On the other hand (for patients with stable spines), we suggest a soft collar turned backward (22).
TABLE 7.1 Comparison of Cervical Orthoses | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Schneider et al. performed a large study examining patient comfort with selected orthoses and correlation with patient size. Data suggest that the Miami J and Aspen collars provided the best comfort. Generally, cervical collars were more comfortable than cervicothoracic orthoses. They concluded that there was no significant association between BMI and brace comfort (23).
SELECTED ORTHOSES
The soft cervical collar has gained popularity for treating cervical strains and so-called whiplash syndromes. Soft collars are inexpensive and comfortable but provide only minimal motion restriction (Table 7.1). Soft collars provide warmth, promote muscle relaxation, and provide a kinesthetic reminder to patients following minor cervical strains. Soft cervical collars are available in numerous sizes and are well tolerated by patients (Fig. 7.1).
The Philadelphia collar is a two-piece semirigid Plastazote orthosis reinforced with ventral and dorsal plastic struts (Fig. 7.2). It is relatively inexpensive and provides better motion control than a soft collar, as detailed in Table 7.1. In addition, the Plastazote construction of the Philadelphia collar makes it a good choice for use during
showering and bathing. Due to the absence of a removable liner, the Philadelphia collar is not as optimal for hygiene or comfort with long-term use as the Miami J, Aspen, and Malibu collars.
showering and bathing. Due to the absence of a removable liner, the Philadelphia collar is not as optimal for hygiene or comfort with long-term use as the Miami J, Aspen, and Malibu collars.
 Figure 7.1. The soft cervical collar has a foam insert housed in a cloth exterior. The collar is fastened with a Velcro strap dorsally. |
 Figure 7.2. The Philadelphia collar is available with a tracheostomy window as shown. It has a front and back portion with Velcro fasteners on each side. |
 Figure 7.3. The Aspen collar has removable padded inserts and malleable plastic tabs around the edges of the brace for comfort. |
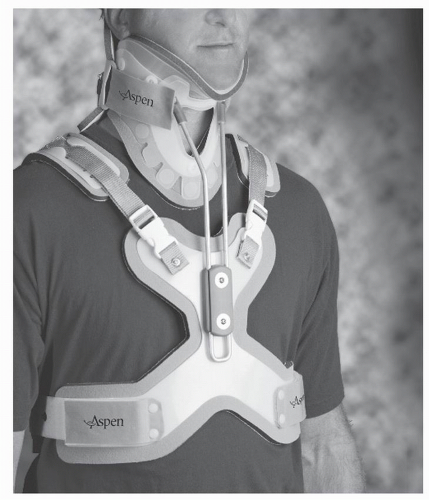 Figure 7.4. The Aspen cervicothoracic orthosis system uses an Aspen cervical collar attached to an adjustable padded vest for better control of the cervicothoracic junction. |
 Figure 7.5. The Miami J collar has comfortable padded inserts and an anterior extension to better control cervical flexion.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




