History and Background
Starting with the early clinical series of Roy-Camille in the 1960s 1,2,3,4,5,6 and gaining popularity in the 1980s, pedicle screw fixation has been used in the thoracolumbar spine for mechanical stabilization, deformity correction, and fusion. Thoracolumbar pedicle fixation was initially applied to the treatment of traumatic conditions and extended to degenerative disease, tumor, and spinal deformity afterward. Thoracolumbar pedicle screw fixation is now widely accepted as the main stabilization method for various spinal conditions. 1,2,5,7
Cervical pedicle fixation was first described at C2 for a hangman’s fracture by LeConte in 1964 8 and Borne et al in 1984. 9 However, it was not until the early 1990s that the method was clinically applied to the subaxial cervical spine by Abumi et al. 10,11,12
In 1994, Abumi et al reported the first clinical case series using subaxial cervical pedicle screws in the setting of trauma. 10 Since then, the same group has published several case series with cervical pedicle screws for various spinal conditions. 11,12,13,14,15,16,17,18 During the 1990s, multiple reports on anatomic characteristics, entry points, and biomechanical properties of cervical pedicle screws were published. Over the past two decades, research on cervical pedicle screw fixation has expanded to include drill-guide or navigation-assisted methods to minimize the risks and improve outcomes with clinical pedicle screws.
In this chapter, we review the biomechanical and anatomical characteristics, surgical technique, and clinical outcomes of cervical pedicle screw fixation. Finally, we describe clinical settings in which cervical pedicle screw fixation is helpful and advantageous.
13.2 Pros and Cons of Cervical Pedicle Screw Fixation
Cervical pedicle screws follow a trajectory from the lateral mass through the pedicle into the vertebral body. As a result, their main advantage is more rigid fixation than other types of cervical fixation, such as wiring, plating, or lateral mass screws. 19,20,21,22,23,24,25,26 This can allow for more stable fixation and correction, particularly in cervical deformity cases (e.g., one-stage posterior correction of cervical kyphosis). In addition, cervical pedicle screws may be advantageous in patients with osteoporotic bone or highly unstable spines after severe trauma or radical tumor excision. Furthermore, cervical pedicle screw placement may provide a wider fusion bed than lateral mass screws, given the entry of the pedicle screw is located lateral to the entry point for lateral mass screws.
Despite these advantages, there are several drawbacks that have prevented widespread acceptance and utilization of cervical pedicle screws. First and foremost is the risk of vertebral artery injury. 27,28,29,30 Cervical pedicles have smaller diameters and a higher medial convergence angle than those of the thoracolumbar spine. As a result, these anatomical characteristics predispose to lateral pedicle wall violation when placing cervical pedicle screws. In the majority of patients, the vertebral artery passes through the transverse foramen immediately lateral to the pedicle from C3 to C6 in the subaxial cervical spine. Although the majority of unilateral vertebral artery injury is asymptomatic, severe posterior cranial infarction may occur even with unilateral vertebral artery injury if the patient has insufficient collateral flow through their posterior circulation. 29,30
In addition, due to the smaller size of cervical pedicles and foramina, cranial or caudal pedicle wall violation is more likely to cause nerve root injury than in the thoracolumbar spine. As a result of these anatomic complexities, as well as the medicolegal environment in many places and a steep learning curve, many surgeons have shied away from cervical pedicle screw placement and instead performed anterior-posterior combined surgery with traditional lateral mass screws when stronger fixation is warranted.
13.3 Biomechanical Characteristics of Cervical Pedicle Screw Fixation
The first biomechanical study on cervical pedicle screws was performed by Kotani et al in 1994. 19 They found that transpedicular cervical fixation provides greater stability than conventional anterior and/or posterior wiring fixation in multilevel constructs under axial, torsional, and flexion loading in a calf cadaveric model.
Since then, several biomechanical studies have compared the pullout strength of cervical pedicle to that of lateral mass screws. In 2004, Kothe et al showed that cervical pedicle screw fixation has significantly higher initial flexion/extension stability as well as stability after cyclic loading compared to lateral mass screw fixation. 20 Johnston et al confirmed these results and demonstrated significantly less screw loosening and higher pullout strength in cervical pedicle compared to lateral mass screws. 31
In a more recent study in 2014, Ito et al found that the mean pullout strength of cervical pedicle screws was nearly four times greater than the mean pullout strength of lateral mass screws (762 vs. 191 N) after torsion loading, and two times greater after flexion/extension loading (571 vs. 289 N). 32 Duff et al showed that a 360-degree reconstruction model (corpectomy spacer with anterior plating and posterior lateral mass screws from C3 to C7) provided only slightly greater stability compared to C3 and C7 posterior-only fixation with pedicle screws. 24
These biomechanical reports are limited in that they are cadaveric studies that do not consider dynamic stabilizing factors. However, with its three-column fixation, cervical pedicle screw does appear to provide greater stability than lateral mass screws and may therefore be justified in patients with poor bone quality or highly unstable conditions that require more rigid fixation than the usual clinical settings.
13.4 Anatomical Considerations for Cervical Pedicle Screw Placement
13.4.1 Cervical Spine Pedicles
Cervical Pedicle Anatomy
In 1991, Panjabi et al described in detail the anatomical dimensions of the subaxial cervical spine, including pedicle width, height, cross-sectional area, and medial and sagittal angles. 33 Since then, several other studies have attempted to quantify the dimensions and angulations of cervical pedicles using cadavers or computed tomography (CT) images. Common findings from these studies are as follows:
The width and height of the subaxial cervical pedicles are smallest at C3 and gradually increase down to C7.
The medial angle of the pedicle is greatest at C3 (approximately 45 degrees; range: 42–55 degrees) and gradually decreases down to C7 (approximately 32 degrees; range: 24–48 degrees).
The sagittal angle changes from a cranial orientation at C3 and C4 (3–15 degrees), to an almost neutral orientation at C5, to a caudal orientation at C6 and C7 (0–11 degrees). 34,35,36,37,38,39
Despite these general principles, it is essential to examine and measure the cervical pedicles on preoperative imaging given the extensive variability in individual spines.
Rao et al reported the mean width and height at all subaxial levels were sufficiently large to accommodate standard 3.5-mm pedicle screws in 98% of the young, healthy volunteers enrolled in a normative CT study. 38 Pedicle widths smaller than 4 mm were rare exceptions (1.7% of the pedicles) and generally observed in women. In general, cervical pedicle screw fixation is not recommended in young children, 40 unless preoperative imaging shows sufficient size of their pedicles for appropriate fixation.
Another important anatomic characteristic of the cervical pedicles is in their 3D structure. 36,40,41 They have an elliptical to triangular cross-sectional shape, with a medial wall that is 1.4 to 3.6 times thicker than the lateral wall, similar to the thoracolumbar spine. This is yet another reason that lateral wall violation is more likely than medial wall violation for cervical pedicle screws and may predispose to vertebral artery injury.
Entry Points
Many researchers have published various cervical screw entry points in the literature. In 1994, Jeanneret et al recommended an “entry point 3 mm beneath the facet joint on the vertical line in the middle of the articular mass’” with an average 45-degree medial angle 35 . Common recommendations from the subsequent studies are as follows:
The entry point should be close to the bony notch below the facet joint in the cranial-caudal plane, furthest away at C7 and getting gradually closer at C3.
In the medial-lateral plane, the entry point should be the most lateral at C3 and gradually move medially by C7. However, it should not be in the medial half of the lateral mass. 34,35,36,37,38
Perhaps most importantly, like pedicle screw trajectory, length, and diameter, the entry point should be individualized to local anatomy and measurements on preoperative images.
13.4.2 Vertebral Artery and Nerve Roots in Subaxial Cervical Spine
The vertebral artery arises from the subclavian artery and enters the transverse foramen at the C6 level in more than 90 to 92% of patients. However, in some patients, the vertebral artery may enter the foramen at an abnormal level: specifically, C5, C4, and C7 in order of frequency in the literature. 27,42,43 The following points about the course of the vertebral artery in the cervical spine should be noted:
The course is not always straight; it may be tortuous following degenerative changes in the cervical spine.
The location of the vertebral artery within the transverse foramen is anterior and medial, instead of central.
There may be a significant difference in flow/diameter of the right and left vertebral arteries, with one side extremely small or even absent. If one side is known to be dominant from preoperative imaging, the surgeon should be extremely careful to avoid vertebral artery injury on that side during surgery.
Anatomical studies show that, unlike lumbar nerve roots, cervical nerve roots pass through the foramina closer to the inferior than superior pedicle in the sagittal plane. 44 In the coronal plane, the nerve root exit angle is largest at C3 (where it is approximately 90 degrees) and gradually decreases to C6 and C7. 44 The cervical nerve root overlies the intervertebral disc level at C4–C5 and traverses the proximal part of the intervertebral disc at the C5–C6 and C6–C7 levels. These findings imply that superior pedicle wall violation is more likely than inferior wall violation to produce nerve root symptoms in the cervical spine. 45
13.5 Cervical Pedicle Fixation Techniques
13.5.1 Abumi’s Technique and Modifications
Abumi’s Original Technique
In their initial article, 10 Abumi et al described the cervical pedicle screw entry point as “slightly lateral to the center of the articular mass and close to the posterior margin of the superior articular surface,” with a medial angulation of 30 to 40 degrees. For safe insertion of pedicle screws, they made their entry point with a high-speed burr, 3 to 4 mm in diameter. This allowed them to bury their screw anchor heads, and also to visualize the entrance of the pedicle with a “funnel” technique, similar to that described in thoracic pedicle screw placement. They used fluoroscopy to confirm the sagittal location of the entry point and trajectory angle.
Modified “Funnel” Techniques
Several modifications of cervical screw placement technique have been reported since 2012, 46,47,48 and mirror the development of new cervical implant technologies. For example, Lee et al described a “key slot” technique which is a modified entry hole that creates a slot in the coronal plane and a triangular shape in the axial plane based on the pedicle medial angle. This technique may avoid the bony defect produced by the Abumi’s “funnel” and fits better with modern polyaxial screw heads. 46
Authors’ Preferred Technique
Preoperative Examination
To check for vertebral artery abnormal course and dominance, we obtain vascular-enhanced CT scans on all patients prior to cervical pedicle fixation surgery. We also use these preoperative CT scans to measure the convergence angle and the minimum diameter of the pedicle in the axial plane at each instrumented cervical vertebra (▶ Fig. 13.1). We select the length of the screw so that it passes into the anterior one-third of the vertebral body on preoperative imaging. If patients have a pedicle diameter less than 3.5 mm or a pedicle convergence angle greater than 50 degrees, we do not perform cervical pedicle screw fixation at these levels.
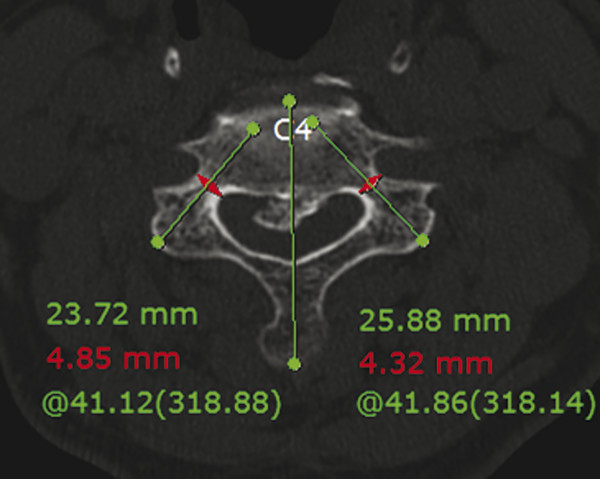
Fig. 13.1 Preoperative measurement of the pedicle diameter, medial convergence angle, and screw length on the axial CT.
Insertion Technique
To find the correct trajectory, we target the virtual pedicle entry point, which is on the line perpendicular to the pedicle’s axis (▶ Fig. 13.2a). We begin by creating a key slot–shaped entry on the medial half of the lateral mass with a 3-mm matchstick burr. The key-slot entry shape is a rectangle in the coronal plane (▶ Fig. 13.2b) and a right-angled triangle in the axial plane (▶ Fig. 13.2c). The apex of the triangle is the virtual pedicle inlet, and the oblique side of the triangle is the pedicle’s axis (▶ Fig. 13.2a, c). In the sagittal plane, the depth of the drilled entry point is two-thirds of the lateral mass thickness (▶ Fig. 13.2d).
The exact width, depth, and angle of the slot are adjusted according to the individual anatomy of the cervical vertebra on preoperative CT images. When a surgeon is first learning to place cervical pedicle screws, he or she may confirm the location of the entry point and screw trajectory in the sagittal plane with lateral fluoroscopy. With practice and experience, cervical pedicle screw placement is possible without fluoroscopic guidance.
After drilling the key slot–shaped entry, we gently probe the pedicle as close to the medial wall as possible with a 15-degree curved awl. After probing to an approximate 2-cm depth, we confirm the lack of pedicle breach using a ball-tip probe. If we detect a pedicle breach, we change the screw trajectory or skip this level. After confirming there is no pedicle breach, we sequentially drill, tap, and insert the screw in the usual fashion.
A screw with a head that is located on the lateral margin of the lateral mass with a tip that is medial to the uncovertebral joint on plain radiographs is considered to be in the safest position. A screw tip positioned laterally to the uncovertebral joint or a head located out of the lateral mass is expected to increase the risk of pedicle breach 49 (▶ Fig. 13.3).
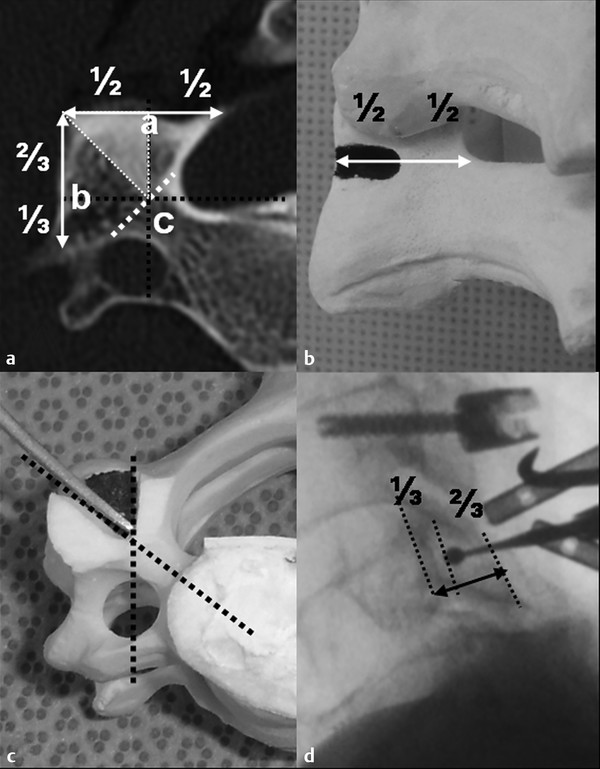
Fig. 13.2 Cutting burr (3 mm). The entry shape is a rectangle in the coronal plane (a) and a right-angled triangle in the axial plane (b). The apex of the triangle is the virtual pedicle inlet and the oblique side is the pedicle’s axis (c). In the sagittal plane, the drilled entry depth is two-thirds of the lateral mass thickness, as seen on fluoroscopy (d).
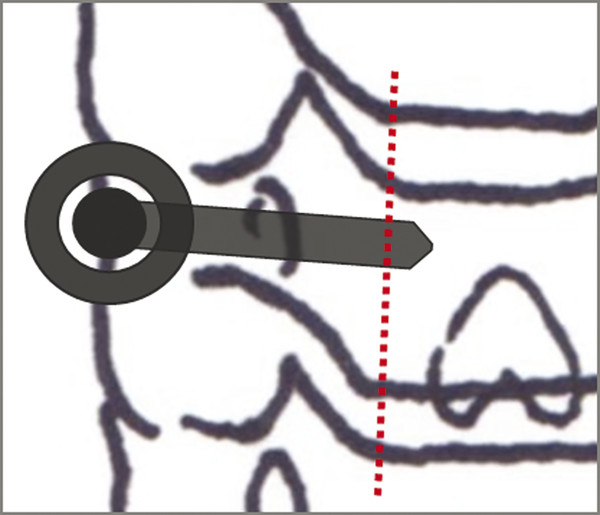
Fig. 13.3 A schematic drawing of an ideal screw trajectory on an anterior-posterior radiograph. A screw with a head that is located on the lateral margin of the lateral mass with its tip medial to the uncovertebral joint is considered to be in the safest position. A screw tip positioned laterally to the uncovertebral joint area or a screw head located out of the lateral mass is expected to increase the risk of pedicle breach.
13.5.2 Foraminotomy-Assisted Technique
In 1998, Albert et al 50 described their “laminoforaminotomy” technique for lower cervical pedicle screws. They recommended direct pedicle medial wall palpation via a C6–C7 laminoforaminotomy. Since then, several authors have reported similar modifications using foraminotomies to place cervical pedicle screws. 47,48,51
The foraminotomy is a simple method to visualize the medial pedicle wall and is helpful for cervical pedicle screw fixation in C7 or T1. It is also possible to perform foraminotomies for pedicle screw placement in the midcervical spine. However, it may take more operative time, requiring greater bony removal and higher blood loss, from C3 to C5 because these levels have greater pedicle medial angles and lateral mass anterior-posterior dimensions than the C6–C7 level.
13.5.3 Navigation-Assisted Technique (▶ Fig. 13.4)
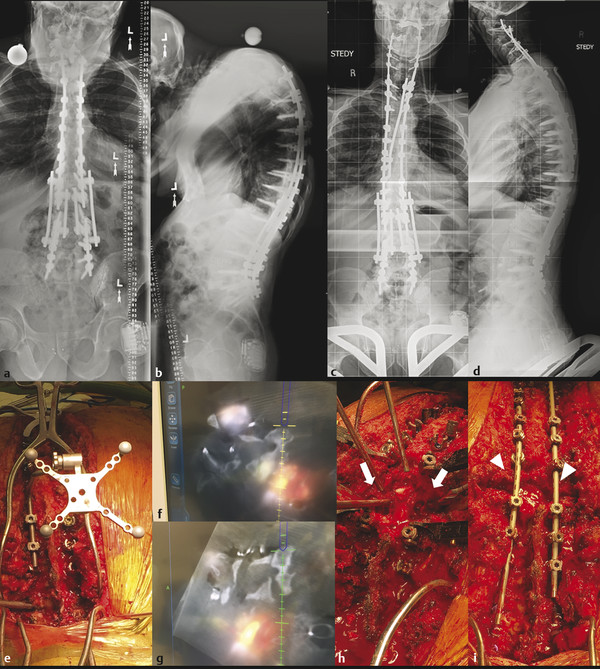
Fig. 13.4 Preoperative (a,b) radiographs of a 61-year-old male patient with a history of multiple thoracolumbar deformity surgeries and proximal junctional kyphosis at T3. A posterior vertebral column resection (PVCR) was performed at T3 with extension of fusion up to C2. Postoperative radiographs show significant improvement of sagittal balance (c,d). Cervical pedicle screws were inserted for cervical spine fixation using the O-arm and Stealth navigation-assisted technique (e-g). (h,i) The bony gap after T3 PVCR (arrows in h) was closed after reduction and rod assembly (arrowheads in i).
In an effort to enhance accuracy and safety, computer-assisted navigation techniques have been applied to cervical pedicle screw placements. Several cadaveric studies in the 2000s demonstrated improved accuracy with navigation-assisted cervical pedicle screw placement compared to conventional techniques. 52,53,54,55 In 2003, Kotani et al reported the first clinical outcomes which showed significantly improved accuracy with navigation-assisted cervical pedicle screw placement: 1.2 versus 6.7% pedicle wall breach rates compared to the conventional freehand technique. 52 Since this report, many clinical case series using different types of intraoperative navigation systems (3D fluoroscopy, O-arm, intraoperative CT, etc.) have confirmed these findings. 54,55,56,57,58,59,60,61,62,63 Taken together, these studies suggest that navigation-assisted pedicle screw placement is more accurate than the freehand technique, although there is no clear difference in terms of neurovascular complications and reoperation rates. However, we recommend navigation-assisted cervical pedicle screw placement especially for unusual anatomy, revision surgery, and pediatric or complex spinal deformity cases.
13.5.4 Drill and Screw-Guide Template-Assisted Technique
The use of templates based on a patient’s individual anatomy have been developed to avoid the high financial and time cost of navigation equipment, the learning curve of using navigation technology, and the additional radiation exposure for the patient. Initial efforts in the 2000s used a custom-made guiding device or CT film template, but more recently in the 2010s, 3D remodeling software and printing systems have been applied to cervical pedicle screw placement. 64,65,66,67 Clinical case series show good accuracy of templates comparable to those of surface landmark–guided or navigation-guided cervical pedicle screw placement.
13.6 Clinical Series and Outcomes
In the first case series, Abumi et al treated 13 patients with traumatic conditions using cervical pedicle screws, reporting satisfactory clinical outcomes without pseudarthrosis or other major complications. 10 Abumi and coworkers have reported good neurological and radiographic outcomes in several consecutive case series using cervical pedicle screw fixation for nontraumatic cervical spine pathology including kyphosis, spondylotic myelopathy, ossification of the posterior longitudinal ligament, rheumatoid arthritis, and metastatic tumors (▶ Table 13.1).
Authors | Number of patients/screws | Placement technique | Accuracy criteria | Pedicle breach rate | Complications | Other |
Abumi et al (2000) 71 | 180/667 | Fluoroscopy-guided, freehand | Pedicle breach or no breach | 6.7% | Radiculopathy (2) VAI (1) | |
Yoshimoto et al (2005) 72 | 27/134 | Fluoroscopy-guided, freehand | No breach Partial: <1/2 screw diameter Complete: >1/2 screw diameter | Partial: 7.4% Complete: 3.7% | None | Breach rate decreased from 12 to 7% after the first 18 cases |
Kast et al (2006) 67 | 36/94 | Mixed: navigation-assisted, freehand | Correct: <1 mm violation Minor: <25% of transverse foramen Major: >25% | Correct: 70% Minor: 21% Major: 9% | Radiculopathy (3) | More common pedicle perforation at C3 and C4 Perforation rate decreased from 13 to 4% after the first 20 cases |
Ito et al (2008) 57 | 50/176 | 3D fluoroscopy navigation-guided | Grade 1: no breach Grade 2: <2 mm Grade 3: >2 mm | Grade 2: 2.8% Grade 3: 0% | None | |
144/417 | Fluoroscopy axial view–guided technique | Exposure: <50% of screw diameter Perforation: >50% | Exposure: 9.2% Perforation: 3.9% | Radiculopathy (1) VAI (1) | ||
Ishikawa et al (2010) 56 | 21/108 | O-arm-based navigation | Grade 0: no exposure Grade 1: <2 mm Grade 2: 2–4 mm Grade 3: <4 mm | Grade 1: 8.3% Grade 2: 2.8% Grade 3: 0 | None | |
Lee et al (2012) 46 | 50/277 | Fluoroscopy-guided freehand (modified Abumi technique) | Grade 0 Grade 1: <25% screw diameter exposure Grade 2: 25–50% Grade 3: >50% | Grade 1: 12.6% Grade 2: 7.6% Grade 3: 2.2% | None | Breach rate decreased from 20 to 2.7% after the first 10 cases |
Nakashima et al (2012) 69 | 84/390 | Mixed: fluoroscopy-guided, freehand, navigation-assisted | Grade 1: <50% of screw diameter Grade 2: >50% | Grade 1: 15.4% Grade 2: 4.1% | Radiculopathy (3) VAI (2) | High breach rate in cervical kyphosis and cerebral palsy patients |
Hojo et al (2014) 55 | 283/1065 | Fluoroscopy-guided, freehand | Grade 1: <50% of screw exposure Grade 2: >50% | Grade 1: 9.6% Grade 2: 5.3% | VAI (2) | High perforation rate in rheumatoid patients. |
Uehara et al (2014) 60 | 129/579 | Navigation-assisted | Grade 1: no breach Grade 2: <50% of screw diameter Grade 3: >50% | Grade 2: 13.3% Grade 3: 6.7% | None | Breach is more common at C3–C5 |
Kaneyama et al (2015) 65 | 20/80 | Patient-specific drill guide template | Class 0: no breach Class 1: <50% screw diameter exposure Class 2:>50% Class 3: complete exposure | Class 1: 2.5% No class 2 or 3 | 3D printing technique | |
Abbreviation: VAI, vertebral artery injury. Note: No VAI in the case series reported was symptomatic. | ||||||
Other groups have confirmed the favorable outcomes and low complication rates of cervical pedicle screw placement. 46,51,56,57,59,69,71,72,73,74 One study proposed that cervical pedicle screw placement is a good fixation option for cervical fractures involving both the lateral mass and pedicle in order to minimize the necessary points of fixation. 17 Rajasekaran et al reported good outcomes in a cohort of pediatric patients (mean age = 9.7 years old) requiring craniovertebral junction stabilization, suggesting cervical pedicle screw fixation may be an option in children as well. 68 Watanabe et al demonstrated an 81% fusion rate with posterior-only cervical pedicle screw fixation in athetoid cerebral palsy patients. 70 In summary, the literature suggests the cervical pedicle screw fixation technique can be applied to nearly any clinical condition requiring posterior fixation of the cervical spine.
13.7 Accuracy and Complications
The accuracy of cervical pedicle screw placement has been extensively assessed by numerous authors. However, it is not easy to compare results between series as they often use variable diagnostic criteria for pedicle breaches (▶ Table 13.1). In Abumi’s first case series, the authors found 3 cortical breaches out of 52 screws (5.8%), based on postoperative CT scans. 10 Consecutive studies from the same authors report pedicle breach rates ranging from 4.7 to 6.9%.
In the literature, the incidence of noncritical pedicle breach (<50% of screw diameter exposed) ranges from 14.8 to 20%, and critical pedicle breach (>50% of screw diameter exposed) ranges from 4.1 to 9%. On average, 60 to 70% of pedicle perforation is in the lateral direction and approximately 30% is in the medial direction. In addition, several studies demonstrate learning curves of cervical pedicle screw placement. More specifically, the incidence of critical pedicle breach decreases significantly after the initial 15 to 25 cases. 46,69,71
Fortunately, most cases of the misplaced cervical pedicle screws described in the literature are asymptomatic. However, the most serious complication of cervical pedicle wall breach is vertebral artery injury due to a lateral breach, followed by cervical nerve root injury due to a superior or inferior breach. Spinal cord injury is less common as the cervical pedicle medial wall is thicker, medial breaches are rare, and there is a lot of space between the medial pedicle wall and the spinal cord itself.
In 2000, the first comprehensive study by Abumi et al on cervical pedicle screw complications reported 3 patients with neurovascular complications (1.7% of the patients; 0.4% of 669 total cervical pedicle screws in 180 patients). 68 Kast et al found 2 patients with critical screw breaches resulting in neurological symptoms out of 94 pedicle screws placed in 26 patients (2.1% of screws; 7.7% of patients). 67 Yukawa et al reported one vertebral artery injury (0.16%) and one radiculopathy (0.16%) out of 620 cervical pedicle screws in 114 patients. 73 In 2012, Nakashima et al reported three nerve root injuries (3.6%) and two vertebral artery injuries (2.4%) out of 84 patients undergoing cervical pedicle screw fixation for nontraumatic pathology. 69 Up until 2018, only two cases of cerebellar and/or brainstem stroke due to cervical pedicle screw misplacement have been reported in the English literature. 29,30
In a systematic review by Yoshihara et al, perioperative neurological and biomechanical complication rates (including pseudarthrosis) are similarly low for cervical pedicle and lateral mass screws, but vertebral artery injuries are significantly more common with cervical pedicle screw placement. 76
13.8 Clinical Applications of Cervical Pedicle Fixation
In this section, we present several broad categories of clinical applications for cervical pedicle screw fixation. Indications can be expanded depending on the individual patient’s bone quality, fusion levels, and local anatomy.
13.8.1 Rigid Fixation for Weak Bone
As several biomechanical studies indicate, cervical pedicle screw fixation provides better fixation strength not only immediately postoperatively but also later after repetitive cyclic loading. One can therefore avoid an anterior-posterior combined surgery by placing strong three-column stabilization via posterior cervical pedicle screws alone. This is particularly advantageous in patients with severe osteoporosis (mean T-score at femoral neck of -4.5 in ▶ Fig. 13.5 example), rheumatoid arthritis, destructive arthropathies, chronic steroid usage, or other pathologies that predispose to weak bone.
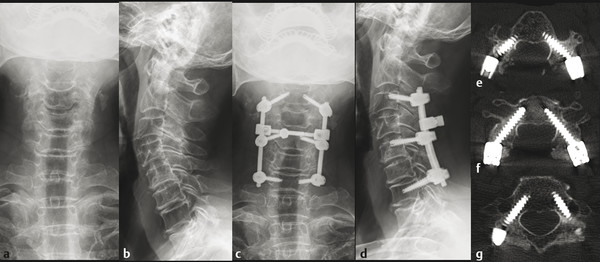
Fig. 13.5 A 78-year-old female with multilevel cervical spondylotic myelopathy and history of severe osteoporosis (mean T-score at femur neck of -4.5) underwent posterior laminectomy and fusion from C3 to C7. Preoperative (a,b) and postoperative radiographs (c,d) are shown. Cervical pedicle screws were successfully placed at C3, C5, and C7 (e–g) without pedicle wall perforation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


