The majority of cervical deformities in adults are kyphotic, and such sagittal plane deformities can produce pronounced symptoms and significant disability. Cervical deformity may result from a number of pathologies including degenerative changes, fractures, myopathies, inflammatory spondyloarthropathies, and iatrogenic complications such as postlaminectomy kyphosis. 1,2,3,4,5 Patients may suffer from dysphagia, difficulty in maintaining horizontal gaze, and gait impairment that can impair activities of daily living (ADLs). 6 Additionally, associated lengthening and flattening of the cord can cause ischemia and spinal cord injury, resulting in myelopathy. Patients may also experience compensatory severe neck pain and interscapular pain as a result of efforts to maintain horizontal gaze.
The correction of cervical deformities poses unique challenges as compared to deformities in the more rigid thoracic spine. These challenges reflect the complexity of the cervical spine, which has the widest range of motion and is critical for the maintenance of neutral head position and horizontal gaze. A number of different surgical strategies exist for deformity correction, including anterior, posterior, and combined approaches. The optimal surgical approach, extent of osteotomy, and levels involved depend on a number of anatomical and deformity-specific considerations. Extensive osteotomies, such as pedicle subtraction osteotomy (PSO), may be warranted.
Similar to its application in the correction of thoracolumbar deformities, PSO can be highly effective in the correction of sagittal plane deformities in the cervical spine. Historically, Smith-Peterson osteotomies (SPO) or combined anterior-posterior (AP) approaches have been the preferred technique for the correction of cervical deformities. 7,8,9,10 However, in cases of nonmobile, fixed cervical deformities, such as patients with ankylosing spondylitis (AS) or diffuse idiopathic skeletal hyperostosis, three-column osteotomies (PSO and vertebral column resection [VCR]) may be warranted. Unlike SPO, in which resection is limited to the posterior elements of the spine, PSO involves wedge resection of the vertebral body and facet joints (as in SPO). In a PSO, the anterior spinal column functions as a fulcrum, the spinal canal is shortened, and fusion is promoted by bone-on-bone contact. This chapter reviews the preoperative evaluation and surgical management of cervical sagittal deformities, with a focus on the role of cervical PSO.
11.2 Preoperative Evaluation
The goals of surgery in patients with cervical sagittal deformity and malalignment are deformity correction, spinal cord and nerve root decompression, restoration of horizontal gaze, and spinal stabilization through a biomechanically sound construct. 11 Evaluation of both cervical and global spinal alignment is critical for surgical planning. Preoperative evaluation typically comprises standing scoliosis (long-cassette) radiographs that allow for visualization from the external auditory canal to the femoral heads in order to evaluate global and regional sagittal alignment. Flexion and extension X-rays can be used to differentiate rigid versus flexible deformity, ultimately dictating the surgical approach and correction needed. Preoperative computed tomography (CT) and magnetic resonance imaging (MRI) may be used to evaluate vertebral anatomy and spinal cord or nerve root compression.
11.2.1 Cervical Sagittal Alignment and Quality-of-Life Outcomes
The goals of deformity correction are cervical sagittal vertical axis (C2 SVA) less than 40 mm and neutral chin–brow vertical angle (CBVA) evaluated in a fully relaxed C1–C2 position of comfort. Studies examining the correlation between cervical radiographic parameters and health-related quality-of-life (HRQOL) outcomes have been used to guide the extent of correction in cervical deformity surgery. Postoperative C2 SVA and CBVA have been shown to correlate with HRQOL and ADL-related outcomes following deformity correction. 12,13,14 C2 SVA captures regional sagittal plane translation, and is defined as the distance between the plumb line drawn from the odontoid of C2 and the posterior and superior-most point of the C7 vertebral body. 5 Correction should strive to produce postoperative C2 SVA of less than 40 mm. 15 CBVA quantifies horizontal gaze, and is measured by subtending an angle between a vertical line and a line drawn from the patient’s chin to brow on clinical photographs. CBVA should be corrected to as close to 10 degrees as possible. Correction of CBVA following cervical deformity surgery has been associated with improved horizontal gaze, ADLs, and gait. 12,13,14 In evaluating the degree of sagittal correction required, the preoperative assessment of cervical radiographic parameters should be performed on X-rays taken in a position of comfort with a fully relaxed C1–C2, rather than a position in which the patient is told to look straight ahead (▶ Fig. 11.1). X-rays taken in the position of comfort often reveals a greater angular correction required by unmasking the true extent of the sagittal imbalance.
In contrast to C2 SVA and CBVA, there is not an established correlation between C2–C7 Cobb angle (CC) and HRQOL. 16,17 In patients undergoing surgery for cervical kyphosis, Lau et al demonstrated increased kyphosis based on Cobb angles was associated with increased neck pain. 18 However, Smith et al did not find a correlation between CC and modified Japanese Orthopedic Association (mJOA) scale in preoperative patients. 16,17 Similarly, in a prospective, double-blind study, postoperative CC resulting from use of lordotic versus parallel allographs for anterior cervical discectomy and fusion (ACDF) was not correlated with postoperative clinical outcomes. 19 Reasons for the lack of correlation between CC and postoperative outcomes are multifold. Sagittal cervical alignment can be highly variable, 20,21 and normative CC may range from -25 to 44 degrees. Additionally, deformities often do not occur in isolation: structural deformity in one region may produce an abnormal secondary curve in another. Cervical lordosis thus does not necessitate higher HRQOL scores, as it may reflect compensatory changes necessary to maintain sagittal balance and horizontal gaze in patients with thoracolumbar deformity and global sagittal malalignment. 22,23
The degree of correction should also be guided by subaxial and thoracolumbar alignment. 24 The cervical spine is highly mobile and may undergo reciprocal changes to compensate for sagittal deformities elsewhere in the spine. 23,25,26 T1 slope has been identified as a potential predictor of sagittal balance. 27 T1 slope is the angle between a line parallel to the T1 endplate and a horizontal line. T1 slope serves as a surrogate for compensatory subaxial lordosis required to maintain a balanced center of gravity of the head; increasing T1 slope requires increased cervical lordosis to maintain sagittal balance and horizontal gaze. T1 slope can be used to assess whether subjacent deformity is contributing to cervical malalignment: sagittal thoracolumbar deformity is likely present in cases with a T1 slope greater than 30 degrees. 28,29 A close relationship exists between T1 slope and C2–C7 Cobb angle such that a difference greater than 17 degrees between these two measurements suggests true cervical deformity even in the presence of deformity of the thoracolumbar spine.
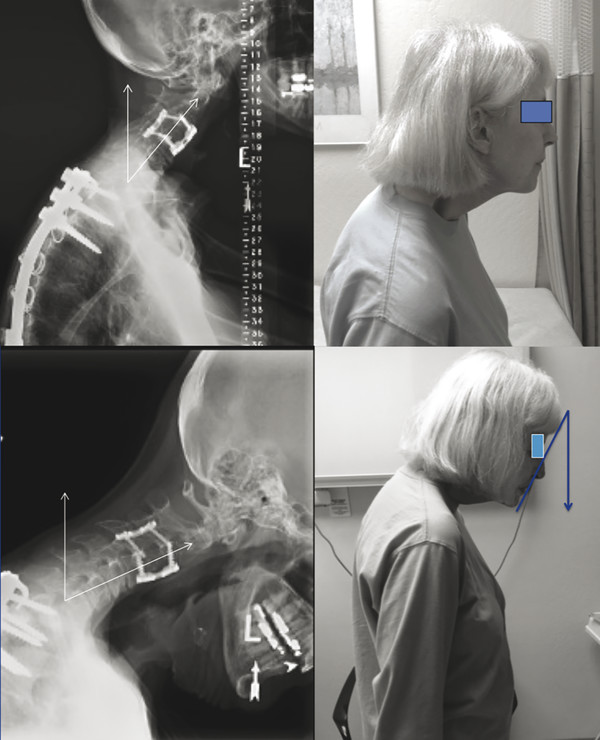
Fig. 11.1 Examples of positioning for evaluation of radiographic parameters. In the top panel, the patient is instructed to look forward. In the bottom panel, the patient is instructed to take a position of comfort, unmasking a larger degree of sagittal imbalance, C2 SVA, and CVBA.
11.3 Surgical Considerations in Cervical Deformity
The extent of deformity correction achieved intraoperatively is dependent on the approach and techniques utilized. Studies have found that 11 to 32 degrees of correction can be obtained with an anterior approach, 30,31,32,33,34 23 to 54 degrees with a posterior approach, 35,36,37,38,39,40,41,42 and 24 to 61 degrees via a combined approach. 4,43,44 Similar to the management of thoracolumbar deformities, cervical osteotomies ranging from facet joint release to complete vertebrectomy may be employed for the correction of cervical sagittal deformity. Ames et al classified cervical osteotomies into seven categories (▶ Table 11.1), and the appropriate osteotomy should be selected based on the degree of correction needed and the rigidity of the deformity (▶ Fig. 11.2). 7 A Grade 1 osteotomy (or partial facet join resection) is a partial resection of the uncinate joints and/or partial removal of the posterior facets. A Grade 2 osteotomy is a complete facet joint resection, wherein both the inferior and superior articular facets are removed. A Grade 3 osteotomy is a complete corpectomy, including adjacent discs. A Grade 4 osteotomy is a corpectomy with associated complete resection of the uncinate joints laterally to the transverse foramen. A Grade 5 osteotomy is the resection of the posterior elements (lamina, spinous process, and facets), closure of the posterior defect, and controlled fracture of the ankylosed anterior column. A Grade 6 osteotomy is a PSO comprising complete removal of the lamina, spinous process, facets, and pedicles at the desired level with a closing wedge osteotomy (CWO) in the vertebral body. A Grade 7 osteotomy is a complete vertebrectomy with removal of the vertebral body and uncinate joints anteriorly, and complete removal of the facets, lamina, and spinous process posteriorly.
Spine type | Cervical osteotomy grade | Technique |
Flexible | 1 | Partial joint resection including partial resection of the uncinate joints and/or partial removal of the posterior facets |
Flexible | 2 | Removal of both the inferior and superior articular facets |
Rigid | 3 | Corpectomy |
Rigid | 4 | Corpectomy with associated complete resection of the uncinate joints laterally to the transverse foramen |
Rigid/ankylosed | 5 | Complete resection of the posterior elements (lamina, spinous process, and facets), closure of the posterior defect, and controlled fracture of the ankylosed anterior column |
Rigid/ankylosed | 6 | PSO (complete removal of the lamina, spinous process, facets, and pedicles at the desired level), followed by creation of a closing wedge osteotomy in the vertebral body |
Rigid/ankylosed | 7 | Complete vertebrectomy (removal of the vertebral body and uncinate joints anteriorly, and complete removal of the facets, lamina, and spinous process posteriorly) |
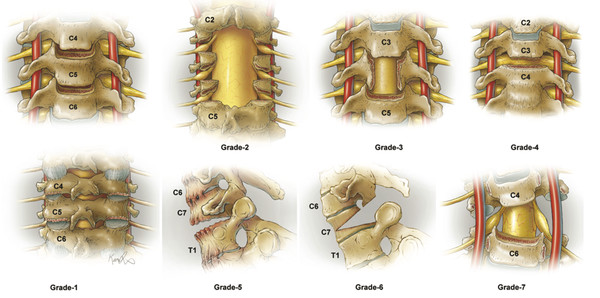
Fig. 11.2 The seven grades of cervical osteotomies offering progressive degrees of destabilization and correction. Please refer to the text for detailed description by grade.
Characterization of the underlying cause of malalignment, degree of rigidity, and type of deformity is critical in surgical planning. Cervical deformities are either rigid (a deformity that cannot be passively corrected) or flexible (a deformity that is passively correctable). Rigid deformities may be ankylosed. In patients with a cervical kyphosis that is ankylosed anteriorly, an anterior osteotomy followed by posterior decompression and instrumentation is favored. Ventral release alone may not provide adequate decompression, and the deformity cannot be corrected without initial anterior release. 43,45 In patients with rigid cervical kyphosis with ankyloses of the posterior elements, a three-step surgery is required for kyphosis correction. A posterior osteotomy is first performed, followed by anterior release with interbody grafting, followed by posterior instrumentation and fusion. This combined approach—anterior, posterior, anterior—allows for both dorsal and ventral decompression with osteotomies for full release of the ankyloses.
Combinations of multilevel discectomies and corpectomies can be performed through an anterior approach. Use of a sequential interbody dilation technique followed by placement of lordotic cages 18 or by placement of an expandable cage 46 can provide significant kyphosis correction, anterior decompression, and internal fixation by an anterior-only approach. Single-level corpectomy and two-level discectomy can provide up to 5 to 8 degrees 47,48,49 of global cervical correction. In cases of midcervical kyphosis, correction can be achieved with a posterior type 2 osteotomy and an anterior type 4 osteotomy. However, anterior approaches carry a unique risk profile with risks for vocal cord injury and dysphagia. Additionally, cases of cervical deformities with fixed posterior elements cannot be correct by an anterior approach alone, and warrant a posterior-anterior-posterior approach. 50,51,52
11.3.1 Correction of Cervical Deformities with Pedicle Subtraction Osteotomy
Cervical PSO is most often indicated in cases of severe fixed kyphotic deformities associated with AS, previous cervical surgery, or trauma. PSOs provide a number of advantages as compared to SPOs. PSOs allow for greater extent of sagittal correction, produce superior biomechanical stability, allow for more controlled closure, produce a large bone-on-bone load-bearing interface that promotes fusion and stiffness, and avoid the anterior open wedge defects associated with SPO. 53,54 Compared to studies on the application of PSO in the thoracic and lumbar spine, reports that focus on cervical PSO are limited. PSOs for cervical deformity are most frequently performed in the cervicothoracic junction at C7, T1, T2, or T3. 13,14,40,43,55,56 Reasons for the preferential application of PSO at the cervicothoracic junction are multifold: the canal diameter is smaller in the upper and middle cervical spine, iatrogenic injury at lower cervical levels can spare the upper extremities, and lower cervical PSO allows for avoidance of the vertebral arteries, which enter the transverse foramen at C6. 57,58
Selection of the lowermost instrumented vertebra (LIV) in cervical deformity correction is aimed at minimizing risk for postoperative distal junctional kyphosis (DJK). The LIV is often in the upper thoracic spine in patients with a normal C2 SVA and mild upper thoracic kyphosis who require a small degree of sagittal correction. In contrast, the LIV should be below the thoracic apex to T9 or lower in patients with significant upper or midthoracic kyphosis, or with global imbalance requiring a cervical PSO.
Traditional Cervical PSO
C7 PSO is performed via a posterior approach. The patient is placed in a prone position and a midline incision is made to expose the cervical and thoracic levels. Subperiosteal dissection is performed to expose the spinous, lateral, and transverse processes of the cervical and thoracic spine. The spine is then instrumented; depending on the construct needed, C2 pedicle screws, C3–C5 lateral mass screws, and thoracic pedicle screws may be placed. The extent of instrumentation depends on patient anatomy and degree of correction needed. Instrumentation can be extended up to C2 to allow for a stronger point of fixation with bicortical screw placement. The caudal extent of instrumentation is determined by the severity of thoracic kyphosis. In patients with normal thoracic curvature, the fusion can end at T3 for three fixation points below the C7 PSO. However, if thoracic kyphosis is pronounced, the fusion may be extended to T5 to involve the thoracic curve apex. 13
The C7 PSO begins with removal of the caudal portion of the C6 lamina and the cranial portion of the C7 lamina as needed. The C7 lateral mass is resected, and the bilateral C6–C7 and C7–T1 facets are removed. The nerve roots at C7 and C8 are exposed, and the C7 pedicle is skeletonized and removed. Sequential lumbar taps with increasing diameter are used to decancellate the vertebral body through the pedicle osteotomy, and the tapped holes are widened and connected. The C7 lateral and posterior vertebral walls are removed, and a 30-degree osteotomy through the vertebral body is performed with osteotomes and down-pushing curettes. To close the PSO, the patient’s head is carefully extended. Following wedge closure, the C7 and C8 nerve roots should be examined to identify possible nerve impingement. After appropriate correction is achieved, the rods are secured with locking caps. It is critical to utilize neuromonitoring data (both somatosensory evoked potentials and motor evoked potentials) throughout the case and particularly during closure of the PSO to prevent iatrogenic injury to the nerve roots and spinal cord. Intraoperative AP and lateral images are obtained to evaluate the degree of correction and overall sagittal alignment of the cervical spine.
Cervical Y-Type Osteotomy
A potential shortcoming of the PSO is the shortening effect on the posterior elements and consequent posterior compression following closure of the wedge osteotomy. This shortening following closure of a C7 PSO can cause root impingement of the C7 and C8 nerve roots. The Y-type osteotomy (YTO)—a modified cervical PSO—was developed to overcome some of the limitations of both CWOs such as the PSO and opening wedge osteotomies (OWOs) such as the SPO, while merging the benefits of each technique. 59 In YTO, the posterior column resection is similar to a CWO, but the tip of the wedge targets the vertebral midsagittal point. A straight plane is osteotomized anteriorly from this point parallel to the endplates. The plane can also be modified according to the intended center of surgical correction. The YTO reduces the amount of anterior distraction that results from an OWO and reduces the posterior shortening produced by CWO, while enabling significant correction. The correction angle can be increased with YTO in comparison to classic PSO as a result of the correction mechanism, while maintaining balance of posterior shortening and anterior distraction.
Case Presentation
PSO can be successfully and safely performed to produce significant correction of lower cervical deformity. An illustrative case is presented (▶ Fig. 11.3, ▶ Fig. 11.4, ▶ Fig. 11.5). A 47-year-old male with a history of AS presents with chin-on-chest deformity and myelopathy. Preoperative AP X-ray, lateral X-ray, and sagittal CT demonstrate a nonmobile, severe cervical kyphosis with scoliosis resulting in significant sagittal malalignment (abnormal C2 SVA) and slight coronal imbalance (▶ Fig. 11.3). Preoperative planning software can be utilized to calculate the angle at cervicothoracic junction and simulate the goal of correction based on standing scoliosis X-rays. An example of a preoperative cervical PSO plan used to guide deformity correction is shown in ▶ Fig. 11.4.
The patient underwent C6 PSO and instrumented fusion for deformity correction. Intraoperative photos can be seen in ▶ Fig. 11.3. Pedicle screws from C3 to T2 are inserted. Bony removal and soft-tissue dissection completely exposes the vertebral artery on both sides (▶ Fig. 11.5a). The pedicles are removed and the spinal nerves are decompressed and exposed widely to ensure compression does not occur during closure of the osteotomy (▶ Fig. 11.5b). The C6 foramen is unroofed along the dotted lines following the placement of pedicle screws (▶ Fig. 11.6a), and the right vertebral artery at C6 is dissected (▶ Fig. 11.6b) and isolated. The C6 pedicle is resected (▶ Fig. 11.6c) and the anterior tubercle is released (▶ Fig. 11.6d). The bony surface is decancellated (▶ Fig. 11.6e), and the osteotomy can be closed using the anterior column as a fulcrum. ▶ Fig. 11.6f shows the complete C6 PSO prior to osteotomy reduction providing significant correction. The instrumentation is secured and fusion graft material is laid down (▶ Fig. 11.5c). Cervical PSO instrument set used for such cases can be seen in ▶ Fig. 11.7. Postoperative AP X-ray, lateral X-ray, and sagittal CT demonstrate significant improvement in sagittal balance with restoration of cervical lordosis (▶ Fig. 11.8).

Fig. 11.3 Preoperative AP (a) and lateral (b) X-rays, and sagittal CT (c) of a patient with severe cervical kyphosis with scoliosis, resulting in significant sagittal malalignment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


