Chapter 34 Cervical Spine and Cervicothoracic Junction
Cervical and Nuchal Anatomy
An understanding of anatomy is the most basic tenet of surgery. Because both ventral and dorsal approaches are commonly used when operating on the cervical spine, it is essential that the spine surgeon be familiar with the anatomy of both the cervical and nuchal regions.1
Anatomic Overview of the Neck
Frick et al. have presented an overview of the anatomy of the neck with the cervical spine as the centerpiece.2 Dorsal to the cervical spine lies the nuchal musculature, which is covered superficially by two large muscles: the trapezius and the levator scapulae. Just ventral to the vertebral bodies lies the visceral space, which contains elements of the alimentary, respiratory, and endocrine systems. The visceral space is surrounded by the cervical musculature and portions of the cervical fascia. Dorsolateral to the visceral space but separated from the visceral space, as well as the cervical musculature, lie the paired neurovascular conduction pathways. Thus, in this scheme, the neck may be divided into five distinct regions: cervical spine, nuchal musculature, visceral space, cervical musculature, and neurovascular conduction pathways.
Surface Anatomy of the Neck
The prominent surface structure of the ventral neck is the laryngeal prominence, which is produced by the underlying thyroid cartilage. The thyroid cartilage is composed of two broad plates that are readily palpable. This cartilage protects the vocal cords, which lie at the midpoint of the ventral surface. Rostral to the thyroid cartilage lies the horseshoe-shaped hyoid bone, which is easy to palpate with the neck extended. The hyoid bone lies in the mouth-cervical angle3 and mediates the muscular attachments of the muscles of the floor of the mouth (middle pharyngeal, hyoglossus, and genioglossus muscles), as well as those of the six hyoid muscles (stylohyoid, thyrohyoid, geniohyoid, omohyoid, mylohyoid, and sternohyoid). The hyoid bone provides some movement during swallowing. This movement is limited caudally to the fourth cervical vertebral body by the stylohyoid ligament.2 The transverse process of the atlas may be palpated at a point marked by a line between the angle of the mandible and a point 1 cm ventrocaudal to the tip of the mastoid process.3
Triangles of the Neck
The sternocleidomastoid muscle divides the neck into two large triangles, posterior and anterior, which are then subdivided into two and four triangles, respectively. Knowledge of these triangles includes a definition of the borders and the contents of each triangle (Fig. 34-1).
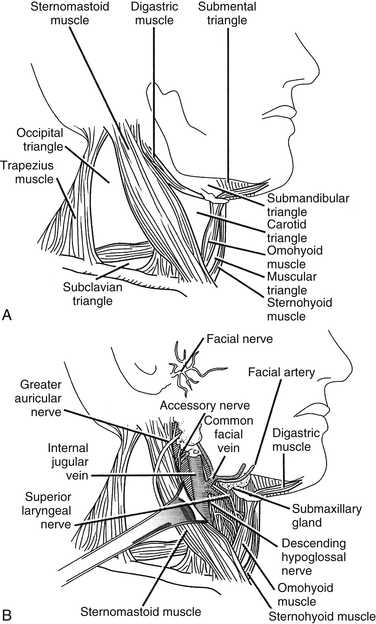
FIGURE 34-1 A, Cervical triangles. B, Carotid triangle and its contents.
(Copyright University of New Mexico, Division of Neurosurgery, with permission.)
Posterior (Dorsal) Triangle
Caudal to the spinal accessory nerve are many important anatomic structures. The external jugular vein, which is formed by the confluence of the posterior auricular and the posterior division of the retromandibular vein at the angle of the mandible, courses over the sternocleidomastoid muscle obliquely to enter the dorsal cervical triangle caudally, en route to joining the subclavian vein approximately 2 cm above the clavicle.3 Two branches of the thyrocervical trunk cross the dorsal cervical triangle. The suprascapular artery runs rostral to the clavicle before passing deep to the clavicle to supply the periscapular muscles. The transverse cervical artery lies 2 to 3 cm rostral to the clavicle and also runs laterally across the dorsal cervical triangle to supply the periscapular muscles.
Anterior (Ventral) Triangle
The submental triangle is bounded by the hyoid body and laterally by the ventral bellies of the right and left digastric muscles. This triangle has, as its floor, the two mylohyoid muscles that connect to each other in the midline by forming a median raphe. Within this triangle lie the submental lymph nodes that drain the ventral tongue, the floor of the oral cavity, the middle portion of the lower lip and the skin of the chin, and several small veins that ultimately converge to form the anterior jugular vein.
The carotid triangle is bounded by the ventral border of the sternocleidomastoid muscle, the rostral edge of the rostral belly of the omohyoid muscle, and the caudal edge of the dorsal belly of the digastric muscle. Within the carotid triangle lie the bifurcation of the common carotid artery, the internal jugular vein laterally, the vagus nerve dorsally, and the ansa cervicalis (see Fig. 34-1B).
Cervical Fascia
An understanding of the cervical fascia aids the surgeon approaching a targeted cervical spine level by providing an avascular plane of dissection. There are three layers of the cervical fascia: investing, visceral, and prevertebral (Fig. 34-2). The investing fascia surrounds the entire neck, splitting to enclose the sternocleidomastoid and trapezius muscles and the submandibular and parotid glands. Rostrally, the investing fascia is connected to the hyoid bone, caudal border of the mandible, zygomatic arch, mastoid process, and superior nuchal line. Caudally, the investing fascia splits to attach to the ventral and dorsal surfaces of the sternum, thus forming the suprasternal space.3 The investing fascia forms the roof of both the ventral and dorsal cervical triangles.
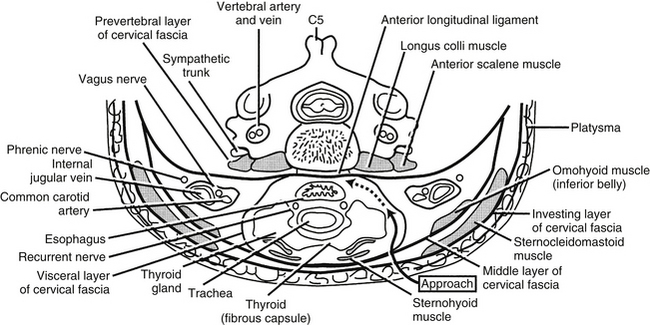
FIGURE 34-2 Cervical fascia.
(Copyright University of New Mexico, Division of Neurosurgery, with permission.)
Cervical Sympathetic Chain
The cervical sympathetic chain (CSC) usually consists of three cervical ganglia that lie at the levels of the first rib, the transverse process of C6, and the atlantoaxial complex, respectively. The CSC lies directly over the longus colli muscles and beneath the prevertebral fascia.4 The chain runs in a superior and lateral direction with an average angle of 10.4 ± 3.8 degrees relative to the midline.4 The superior ganglion is typically located at C2-34 or C45 and lies more laterally on the splenius capitis. The average distance between the CSC and the medial border of the longus colli muscles at C6, however, is 10.6 ± 2.6 mm.4 Therefore the CSC is considerally more vulnerable to damage at lower levels due to its more medial location. While the longus colli diverge laterally when descending down the cervical spine, the CSCs converge medially at C6.4 The average diameter of the CSC at C6 is 2.7 ± 0.6 mm.4 Potential damage to the CSC may result during longus colli dissection off the anterior vertebral bodies or during lateral rectraction of the carotid sheath and/or longus colli.4 Fibers from the superior cervical ganglia pass to the internal carotid artery to innervate the pupil. Interruption of the sympathetic trunk in the neck results in an ipsilateral Horner syndrome.
Cervical Musculature
The cervical musculature is divided into two layers: superficial and deep. The muscles of the superficial layer include the platysma, the sternocleidomastoid, and the infrahyoid group. The platysma lies just under the surface of the skin and is one of the muscles of facial expression, innervated by the cervical ramus of the seventh cranial nerve. It is draped like an apron from the mandible to the level of the second rib and laterally as far as the acromion processes. The sternocleidomastoid muscle arises from the region of the jugular notch and courses rostrolaterally to the mastoid process. It is dually innervated by the 11th cranial nerve and ventral branches of the C2-4 spinal nerves. The spinal accessory nerve enters the deep surface of the muscle at the border of the middle and rostral thirds. The two main actions of the sternocleidomastoid muscle are to turn the head to the contralateral side and to flex the head ipsilaterally. The infrahyoid group represents the rostral continuation of the rectus muscular system of the trunk.2 This group contains four muscles: sternohyoid, sternothyroid, omohyoid, and thyrohyoid. The first three members of this group are innervated by the ansa cervicalis, and the thyrohyoid receives its innervation from the C1 spinal nerve via the hypoglossal nerve. The main actions of the infrahyoid group are to assist in swallowing and mastication. This group, together with the suprahyoid group, determines the rostrocaudal location of the larynx between the hyoid bone and the rostral thoracic aperture and can help flex the cervical spine and lower the head.
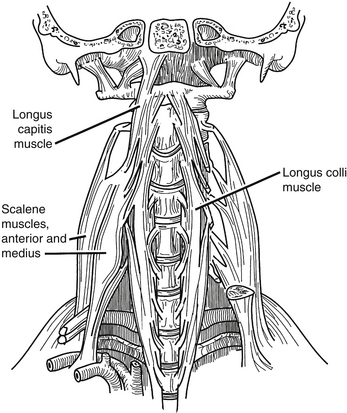
The deep layer of cervical musculature includes two groups: scalene and longus groups. The scalene group includes three muscles: anterior, medius, and posterior. These muscles form a roof over the cupula of the lung. As a group, these muscles arise from the transverse processes of the subaxial cervical spine and project to the first and second ribs. The scalene muscles are innervated by the ventral rami of C4-8. They help to elevate the rib cage during respiration. The longus group also includes three muscles: rectus capitis anterior, longus capitis, and longus colli (Fig. 34-3). As a group, these muscles arise from the ventral vertebral body, transverse processes, and basilar portion of the occiput. They project caudally along the ventrolateral aspects of the cervical and upper thoracic vertebral bodies. These muscles are innervated by the ventral rami of C1-6, and their main action is to flex the head and the cervical spine.
Longus Colli
The longus colli attach to the anterior atlas, the vertebral bodies of C3-T3, and the transverse processes of C3-6.6 The distance between the medial borders of the longus colli muscles increases in a rostral to caudal direction, measuring 7.9 ± 2.2 mm at C3, 10.1 ± 3.1 mm at C4, 12.3 ± 3.1 mm at C5, and 13.8 ± 2.2 mm at C6.6 A great deal of variation exists in this musculature, so care should be taken in using it as a landmark for lateral dissection.
Cervical Viscera
The pharynx is a fibromuscular tube that projects from the pharyngeal tubercle of the clivus to its transition into the esophagus near the level of C6. The dorsal surface of the pharynx lies on the prevertebral fascia and must be mobilized during ventral approaches to the cervical spine. The muscles of the pharynx may be divided into two groups: constrictors and internal muscles of the pharynx. The constrictor group includes three muscles whose main action is to sequentially constrict the pharynx during swallowing, propelling food caudally. All of the constrictors are innervated by the pharyngeal plexus, which receives its branches from both the glossopharyngeal and vagus nerves. The constrictors do not form a continuous tube but are open at four points, allowing certain structures to pass into the pharynx. Rostral to the superior constrictor, the ascending palatine artery, the eustachian tube, and the levator veli palatini muscles pass to enter the pharynx. Between the superior and inferior constrictors pass the glossopharyngeal nerve, the stylohyoid ligament, and the stylopharyngeus muscle. In the gap between the middle and inferior constrictors pass the internal laryngeal nerve and the superior laryngeal artery and vein. Caudal to the inferior constrictor pass the recurrent laryngeal nerve and the inferior laryngeal artery. The internal muscle groups of the pharynx have a common function of elevating the larynx and pharynx during swallowing and a common innervation by the glossopharyngeal nerve. At the level of C6, the pharynx blends into the esophagus, which passes through the superior thoracic aperture to the stomach. In the root of the neck, the esophagus is in close approximation to the thoracic duct as it empties into the left subclavian vein.
Thoracic Duct
The thoracic duct is located on the left side within a triangle bounded medially by the longus colli muscles and the esophagus, laterally by the anterior scalene muscle, and inferiorly by the first rib.7,8 Although it may ascend as high as C6, it is most often found between C7 and T1, before it descends to empty into a variable termination at the jugulosubclavian junction.7,8 The rostral extension of the thoracic duct appears to vary by gender, as in patients who have a narrow thoracic inlet, as most women do, the duct may ascend as high as the level of the C6 vertebral body. Conversely, in patients who have a wide thoracic inlet, as most men do, the duct may ascend to the level of the C7-T1 disc, never truly leaving the mediastinum. Many have cited the increased possibility of injuring this structure in the left upper thorax as a reason for preferring a right-sided approach, especially to the upper thoracic vertebrae.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree