Cervical Stenosis—Asymptomatic with Intrinsic Cord Change— Decompress or Watch?
Andelle L. Teng
Cervical spondylosis is the descriptive term for degenerative changes of the cervical spine. A combination of these progressive age-related changes can lead to narrowing of the cervical canal otherwise known as cervical stenosis. If the diameter of the canal is less than the diameter of the spinal cord, there is resultant compression of the cord. With severe compression, a patient can develop myelopathy and possibly be at increased risk for spinal cord injury (SCI) with minor trauma. When a patient has clear neurologic dysfunction or unremitting pain from cervical stenosis, the decision for surgery is more easily determined. However, the justification to proceed with surgical intervention for the patient where there is cervical stenosis without clinical neurologic dysfunction or symptoms is less clear. Advances in imaging, specifically magnetic resonance imaging (MRI), have led to the ability to view the spinal cord matrix itself. Intrinsic cord signal intensity changes have been observed on T1- and T2-weighted MRI at areas of cervical stenosis. In general, it is believed that cervical stenosis without any clinical signs or symptoms can be monitored. Although the clinical significance of changes in signal intensity of the cervical spinal cord remains unanswered, does a positive finding tip the scale toward prophylactic surgery for asymptomatic cervical stenosis?
PATHOPHYSIOLOGY
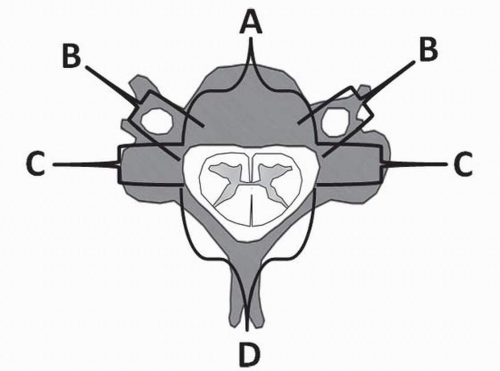
Cervical spondylosis is often due to arthritic changes of facet joints, hypertrophy or buckling of the ligamentum flavum, ossification of the posterior longitudinal ligament, intervertebral disk degeneration and herniation, or osteophyte formation (1, 2, 3, 4 and 5). Typically a combination of these factors leads to cervical stenosis (Fig. 140.1). A person can, additionally, have a dynamically unstable spine leading to cervical cord compression with motion or have an underlying congenital cervical stenosis with a developmentally narrow canal, which is less tolerant of degenerative changes or trauma. Cervical spondylosis and stenosis can lead to cervical radiculopathy if a nerve root is compressed or cervical spondylotic myelopathy (CSM) if the entire spinal cord structure is compressed (4—5). The average sagittal diameter of the adult spinal cord is 10 mm (6), and a recent cadaveric study on 469 adult skeletal specimens found an average anterior-posterior canal in all specimens of 14.1 ± 1.6 mm at the midcervical spine (7). Edwards’ and LaRocca’s (6) review of 63 patients’ radiographs with degenerative spondylosis found that patients with midcervical diameters between 10 and 13 mm were premyelopathic, between 13 and 17 mm the patients were less prone to myelopathy but were prone to symptomatic cervical spondylosis, and greater than 17 mm enabled improved tolerance of the spondylotic changes. A stenotic canal can be determined by the vertebral body ratio method by dividing the sagittal diameter of the spinal canal by the sagittal diameter of the corresponding vertebral body on plain radiographs (8). A value of 0.8 or less suggests cervical stenosis with a reduced space available for the spinal cord (SAC) and an increased risk for neurologic injury with trauma (5,8, 9 and 10). However, the clinician must be cognizant that plain radiographs only depict the bony margins of cervical canal space and does not demonstrate stenosis that often occurs from soft tissue pathology such as disk herniations or ligament buckling or predict the level and degree of cervical cord compression (11). Alternatively, stenosis has also been defined as a decrease in transverse sectional area for the spinal cord on computed tomography (CT) myelography or MRI to less than 55% to 75% of its normal value (12). Others have reported an anterior-posterior compression ratio at necropsy and correlated this with extensive demyelination of the posterolateral funiculus and infarction of the gray matter (Fig. 140.2) (13). Presumably, this ratio can be also calculated on axial cuts on an MRI.
Symptoms of stenosis depend on the specific neural region or structure involved. If a cervical nerve root is
compressed, lower motor neuron dysfunction, termed radiculopathy, can present in anatomical structures innervated by the involved nerve root. This can present as pain and/or motor/sensation abnormalities of the neck, shoulder, suboccipital region, or upper extremity along with a decreased deep tendon reflex (4). However, if the cervical spinal cord is compressed, upper motor neuron dysfunction and long tract signs, termed myelopathy, may be present. The latter may present as brisk deep tendon reflexes, extensor plantar reflexes, inverted radial reflexes, Hoffman’s sign, myelopathy hand, difficulty with fine dexterity, gait and balance abnormalities, bowel/bladder dysfunction, and/or paraparesis (3,5,10,14). CSM can be due to SCI from direct mechanical injury, vascular injury and ischemia, demyelination, and neuron necrosis (2 and 3,5).
compressed, lower motor neuron dysfunction, termed radiculopathy, can present in anatomical structures innervated by the involved nerve root. This can present as pain and/or motor/sensation abnormalities of the neck, shoulder, suboccipital region, or upper extremity along with a decreased deep tendon reflex (4). However, if the cervical spinal cord is compressed, upper motor neuron dysfunction and long tract signs, termed myelopathy, may be present. The latter may present as brisk deep tendon reflexes, extensor plantar reflexes, inverted radial reflexes, Hoffman’s sign, myelopathy hand, difficulty with fine dexterity, gait and balance abnormalities, bowel/bladder dysfunction, and/or paraparesis (3,5,10,14). CSM can be due to SCI from direct mechanical injury, vascular injury and ischemia, demyelination, and neuron necrosis (2 and 3,5).
NATURAL HISTORY OF CERVICAL SPONDYLOSIS/STENOSIS AND PROGRESSION TO MYELOPATHY
The natural history of CSM is not associated with a linear progressive deterioration. Several studies suggest that CSM is a slowly progressive entity that worsens in a stepwise fashion. A patient may therefore have long periods without new or worsening symptoms and then an exacerbation, which is again followed by a period of static symptoms (5,14, 15 and 16). Lees and Turner (16) followed 95 patients with cervical spondylosis. Forty-four had myelopathy and 51 did not. Spondylosis was determined by radiography or myelography. They reported that their patients with myelopathy generally had long periods of nonprogressive disability. These stable symptoms occasionally worsened and then settled into a static state, though often worse than previously. Patients were separated into categories of mild, moderate, and severe disability. Only two deaths were attributed to the spinal cord. In the nonmyelopathic group, 21 had no symptoms, 15 had mild or intermittent symptoms, 14 had more troublesome symptoms or moderate disability, and 1 had severe symptoms. Only one patient developed extensor plantar reflexes and local symptoms of spondylosis. However, at age 86, this patient’s legs felt normal and there were no new neurologic signs. None died of any condition associated with spondylosis. Not a single patient was unemployed because of spondylosis.
There are few studies investigating the progression of asymptomatic cervical stenosis to myelopathy. Bednarik et al. looked at patients with cervical stenosis without clear signs of myelopathy and termed this condition as “presymptomatic spondylotic cervical cord compression” (P-SCCC). Their study included 199 patients with P-SCCC followed prospectively for a minimum of 2 years (range 2 to 12 years). These patients were observed for progression to clinically symptomatic CSM. Clinical evidence of the first signs and symptoms of CSM during the follow-up period was found in 45 patients (22.6%). The 25th percentile time to clinically manifested myelopathy was 48.4 months and symptomatic CSM developed within 12 months in 16 patients (35.5%) (17).
MRI EVALUATION OF THE CERVICAL SPINE
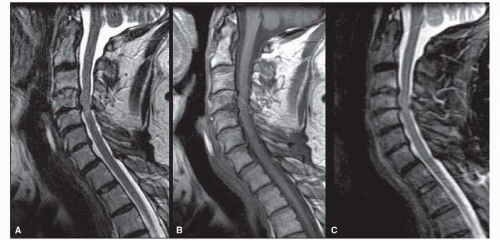
Many earlier studies determined spondylosis and stenosis by radiography or CT myelography as MRI was not yet developed or commonly employed. MRI has supplanted these other imaging modalities and currently serves as the predominant method in evaluating for stenosis and spondylosis. Depending on the various pulse sequences, MRI has the ability to demonstrate the osseous and soft tissue anatomy surrounding the spinal cord and neurologic structures (18). MRI also allows evaluation of the spinal cord itself. The spinal cord normally has a homogenous signal intensity on T1-weighted or T2-weighted images. It is thought that worsening cervical spondylosis leads to cervical stenosis and spinal cord compression. This compression may lead to intrinsic cord changes, such as decreased signal intensity on T1-weighted MR images and increased signal intensity on T2-weighted
MR images (Fig. 140.3). Besides changes of the spinal cord structure and matrix, intramedullary lesions, such as syringomyelia, may be identified as well. Intrinsic cord signal changes may suggest myelomalacia, gliosis, edema, or ischemia from spinal cord compression (11 and 12,19, 20, 21 and 22). Some investigators believe that highintensity signal changes on T2-weighted images indicate edema and gliosis, which may be reversible, whereas low-intensity signal changes on T1-weighted images can represent myelomalacia and necrosis, which may be irreversible (22, 23 and 24). The significance of intrinsic cord changes, how they develop, and whether it can predict progression to myelopathy, degree of myelopathy, or predict surgical outcome has been questioned.
MR images (Fig. 140.3). Besides changes of the spinal cord structure and matrix, intramedullary lesions, such as syringomyelia, may be identified as well. Intrinsic cord signal changes may suggest myelomalacia, gliosis, edema, or ischemia from spinal cord compression (11 and 12,19, 20, 21 and 22). Some investigators believe that highintensity signal changes on T2-weighted images indicate edema and gliosis, which may be reversible, whereas low-intensity signal changes on T1-weighted images can represent myelomalacia and necrosis, which may be irreversible (22, 23 and 24). The significance of intrinsic cord changes, how they develop, and whether it can predict progression to myelopathy, degree of myelopathy, or predict surgical outcome has been questioned.
MRI CORRELATION WITH STENOSIS
MRI signal intensity changes have been repeatedly localized to regions of cervical spinal cord compression. Takahashi et al. found correlation between cervical cord MRI high signal intensity and grade of myelopathy and degree of compression when reviewing 668 patients with compressive lesions of the cervical canal. High MRI signal intensity within the spinal cord was seen in 99 patients (14.8%). Frequency of increased signal intensity was directly proportional to the severity of clinical myelopathy and the degree of spinal canal compression observed on MRI. Patients with a high-signal-intensity area responded less well to both surgical and medical treatment than those without. When the degree of canal compression or myelopathy grade was moderate to marked, more than 60% of patients had increased signal intensity on MRI (20). In a different study, Takahashi et al. looked at 128 patients with compressive lesions of the cervical canal. They generally observed a high-signal-intensity lesion on T2-weighted images in
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree