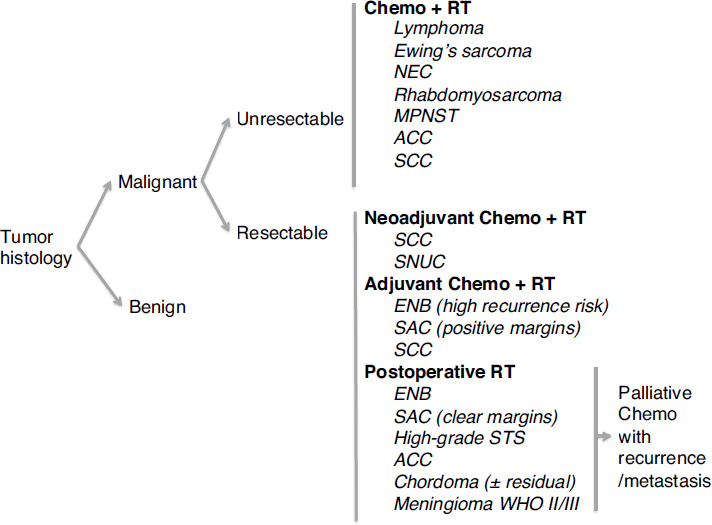
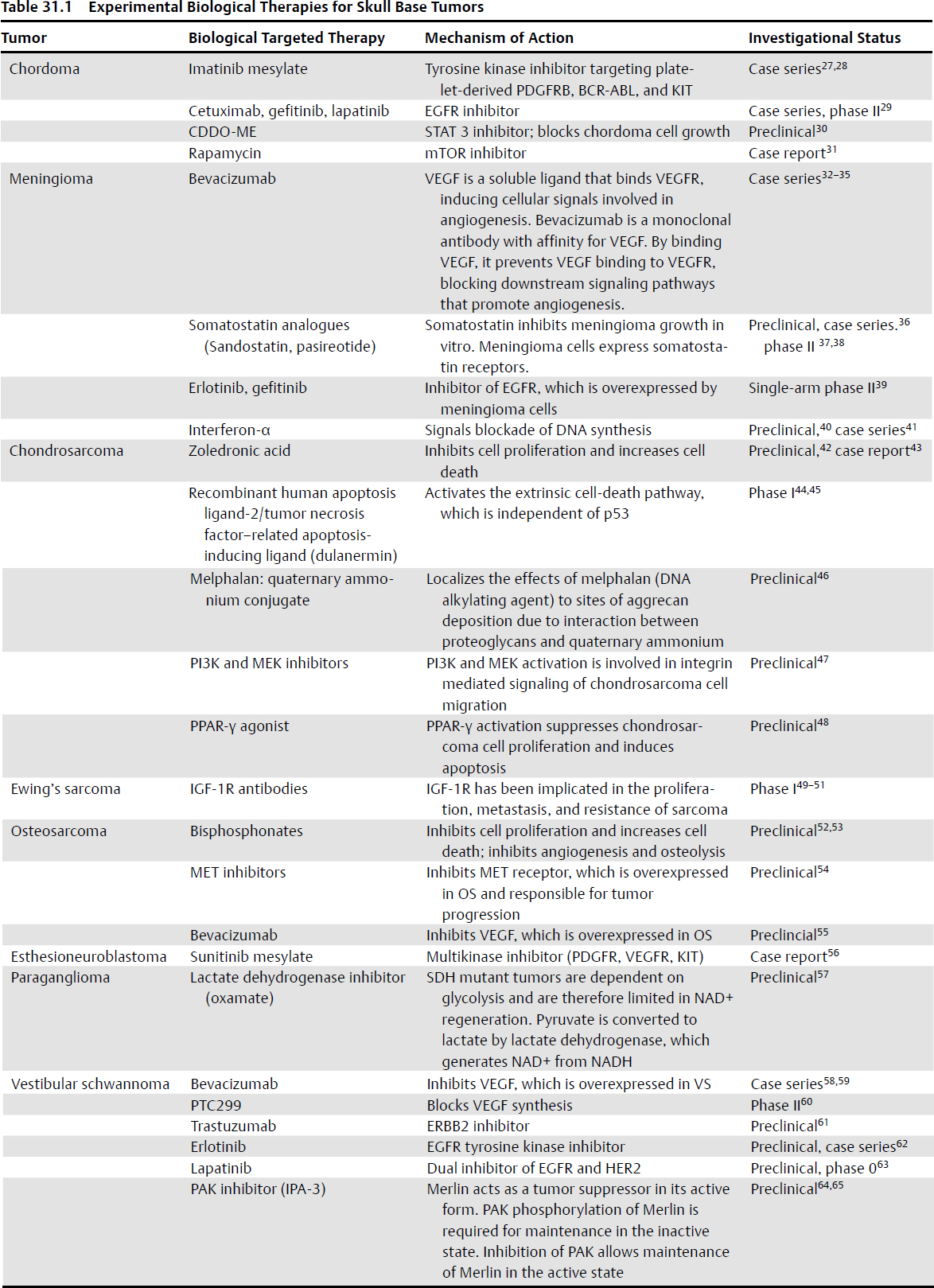
31 Chemotherapy of Skull Base Malignancies Chemotherapy involves the use of synthetic or natural molecules for the purposes of blocking tumor cell functions required for cell division or maintenance of cell viability. • The hallmark traits of cancer that serve as targets of cancer therapy1 are resistance to cell death, angiogenesis, replicative immortality, sustained proliferation signaling, evasion of growth suppressors, activation of migration or invasion, alteration of energy metabolism, and evasion of immune response. • The development of chemotherapeutics for skull base malignancies has focused on the adaptation of cytotoxic agents that have been shown to induce significant tumor cell death or tumor growth inhibition in preclinical models of solid malignancy. • Given the rare nature of skull base malignancy and the diverse pathology, large clinical trials evaluating the use of chemotherapeutic agents are infrequent. Current chemotherapeutic strategies for selected tumors have relied on case series or phase II studies with comparison to historical or contemporaneous control groups. The use of chemotherapy for the management of skull base malignancy is dependent on the histological diagnosis.2 Chemotherapy may be administered prior to surgery or radiation, following surgery, or in the palliative setting for primary or recurrent tumors where surgical or radiation options are absent or limited. Chemotherapy in combination with radiation may be considered as the primary treatment paradigm for moderately to poorly differentiated neuroendocrine carcinomas, lymphoma, Ewing’s sarcoma, rhabdomyosarcoma, and malignant peripheral nerve sheath tumors of the skull base.2 • Induction chemotherapy for reduction of tumor burden prior to surgical resection should be considered for patients with squamous cell carcinoma3–5 and sinonasal undifferentiated carcinoma.6,7 • The addition of chemotherapy to standard radiation treatment in nasopharyngeal carcinoma provides a 20% overall survival advantage at 2 to 4 years over treatment not involving chemotherapy.8 • Squamous cell cancer of the head and neck is treated with induction chemotherapy using the TPF regimen, which consists of docetaxel, cisplatin, and 5-fluorouracil.4,9 This regimen may be combined with concurrent radiation in the event of temporal bone tumors.10 • Concurrent chemotherapy with postoperative radiation is employed for esthesioneuroblastoma patients at high risk of recurrence. Neoadjuvant chemotherapy can be considered for advanced cases of esthesioneuroblastoma.11 • Nonresectable malignant skull base tumors may be treated with a regimen of radiation therapy and concomitant cisplatin or mitomycin C plus adjuvant cisplatin and vinblastine.12 • Chemotherapy for salivary gland carcinomas has not been shown to have a survival effect and is reserved for cases in which the tumor is causing severe symptoms or showing rapid progression.13 • Effective chemotherapy regimens for chordoma, meningioma, or chondrosarcoma have not been described to date. Biological therapies for these tumors are currently under investigation. Fig. 31.1 shows the current treatment indications for chemotherapy in the management of malignant skull base tumors. Cytotoxic chemotherapeutic agents act by inducing DNA damage or impairing DNA synthesis, which initiates cell death pathways in cells that are in the midst of an active cell cycle. DNA damage may be induced directly (doxorubicin [Adriamycin], cyclophosphamide, etoposide, ifosfamide, cisplatin) or indirectly by interfering with mitosis (vincristine, taxanes). Antimetabolites such as methotrexate and hydroxyurea block production of DNA precursors required for DNA synthesis. These agents do not discriminate between proliferating normal cells and tumor cells, which explains side effects involving proliferative tissues of the hematopoietic system, skin, and gastrointestinal tract. • Mitotic inhibitors: vincristine, vinblastine, paclitaxel, docetaxel • Antimetabolites: methotrexate, 5-fluorouracil, hydroxyurea • Anthracycline: doxorubicin (Adriamycin) • DNA-damaging: cyclophosphamide, ifosfamide, cisplatin, mitomycin-C • Topoisomerase inhibitor: etoposide Fig. 31.1 Current treatment indications for chemotherapy in the management of malignant skull base tumors. ENB, esthesioneuroblastoma; SCC, squamous cell carcinoma; ACC, adenoid cystic carcinoma; SAC, sinonasal adenocarcinoma; SNUC, sinonasal undifferentiated carcinoma; NEC, neuroendocrine carcinoma; MPNST, malignant peripheral nerve sheath tumor; RT, radiation therapy; STS, soft tissue sarcoma; WHO, World Health Organization.8,12–26 • Epidermal growth factor inhibitors: e.g., gefitinib • Vascular endothelial growth factor inhibitors: e.g., Bevacizumab Targeted biological therapies are in development for neoplasms that have shown poor response to cytotoxic chemotherapy in the past. These include meningioma, chordoma, chondrosarcoma, and neurofibromatosis type 2 (NF2)–associated vestibular schwannoma. These therapies take advantage of an understanding of the molecular mechanisms underlying tumor cell growth, survival, and migration pathways, and attempt to interfere with these pathways to arrest tumor growth, induce cell death, or block migration and invasion. Table 31.1 shows the current experimental biological therapies for various types of skull base neoplasms. Boldfaced references are of particular importance. 1. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011; 144:646–674 PubMed 2. Demonte F. Management considerations for malignant tumors of the skull base. Neurosurg Clin N Am 2013;24:1–10 PubMed 3. Posner MR, Hershock DM, Blajman CR, et al; TAX 324 Study Group. Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N Engl J Med 2007; 357:1705–1715 PubMed 4. Vermorken JB, Remenar E, van Herpen C, et al; EORTC 24971/TAX 323 Study Group. Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer. N Engl J Med 2007;357:1695–1704 PubMed 5. Hanna EY, Cardenas AD, DeMonte F, et al. Induction chemotherapy for advanced squamous cell carcinoma of the paranasal sinuses. Arch Otolaryngol Head Neck Surg 2011;137:78–81 PubMed 6. Diaz EM Jr, Kies MS. Chemotherapy for skull base cancers. Otolaryngol Clin North Am 2001;34:1079–1085, viii PubMed 7. Righi PD, Francis F, Aron BS, Weitzner S, Wilson KM, Gluckman J. Sinonasal undifferentiated carcinoma: a 10-year experience. Am J Otolaryngol 1996;17:167–171 PubMed
 Indications
Indications
 Mechanism of Action
Mechanism of Action
Cytotoxic Agents
Biological Agents
 Side effects: rash, diarrhea, corneal keratopathy, anemia, fatigue
Side effects: rash, diarrhea, corneal keratopathy, anemia, fatigue
 Side effects: impaired wound healing, elevated liver enzymes, proteinuria, hypertension, hemorrhage, thromboembolism
Side effects: impaired wound healing, elevated liver enzymes, proteinuria, hypertension, hemorrhage, thromboembolism
Biological Therapies
 References
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree