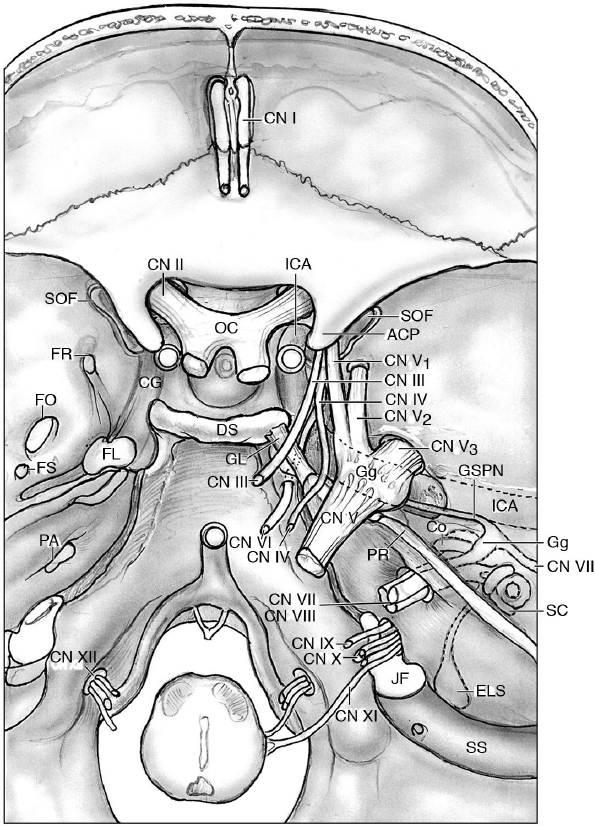
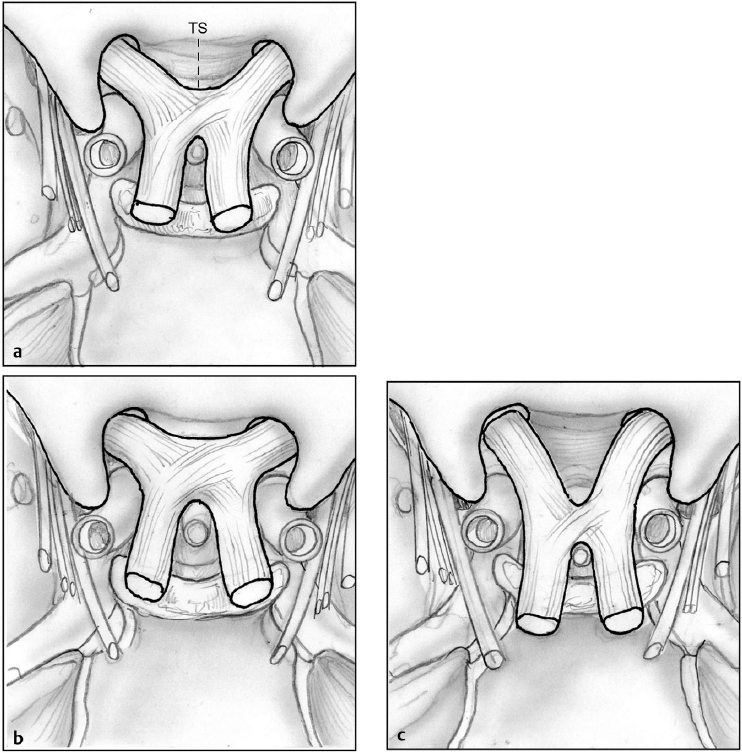
3 Functional Anatomy of the Cranial Nerves Review the anatomic relationship of the 12 pairs of cranial nerves (CNs) that pertain to the skull base as shown in Fig. 3.1. The olfactory nerve is formed by about 20 olfactory filaments, which collect the olfactory fibers coming from the olfactory epithelium in the nasal mucosa. They cross the foramina of the cribriform plate of the ethmoid bone, reaching the olfactory bulb. • The olfactory bulb is the rostral enlargement of the olfactory tract, where mitral cells project their axons to the olfactory cortex via the medial and lateral (and intermediate) olfactory striae in the region of the olfactory trigone at the anterior perforated substance. Surgical Anatomy Pearl Fractures of the anterior skull base with the involvement of the cribriform plate may give rise to cerebrospinal fluid (CSF) leakage with associated anosmia. Typical tumors giving rise to anosmia are cribriform plate meningiomas, nasal/paranasal tumors, and esthesioneuroblastoma. The optic nerve is composed of a bundle of nervous fibers (almost one million fibers) carrying visual information, which leave the retina posteriorly to reach the optic chiasm. It passes through the optic canal, joining the contralateral optic nerve in the optic chiasm, where approximately 50% of the axons coming from the nasal retina cross the midline. The posterior limbs of the chiasm are the optic tracts. The optic nerve is ~ 50 mm long, formed by four segments: • Intraocular, the head of the optic nerve, 1 mm long • Intraorbital, between the globe and the optic canal, ~ 25 mm long • Intracanalicular, within the optic canal, together with the ophthalmic artery and sympathetic plexus, ~ 9 mm long • Intracranial, reaching the optic chiasm in the perioptic and chiasmatic cisterns, 4 to 16 mm long The optic chiasm may have three different positions (Fig. 3.2), in relation to the surrounding structures1,2: • Above the diaphragma sellae (~ 70%) • Above the tuberculum sellae (prefixed, ~ 15%) • Above the dorsum sellae (postfixed, ~ 15%) Fig. 3.2a–c Optic chiasm types. (a) The optic chiasm is above the diaphragm sellae, which is the most typical type. (b) Prefixed type, with a shorter distance between the tuberculum sellae (TS) and the anterior margin of the optic chiasm. (c) Postfixed type, with the optic chiasm above the dorsum sellae. Vascularization occurs mainly from the ophthalmic artery, whereas the optic chiasm is vascularized by perforators from the internal carotid artery, anterior communicating artery, posterior communicating artery, and posterior cerebral artery. The optic nerve also carries some fibers involved in the pupillary reflexes: retinopretectal tract and retinocollicular tract. The pathophysiological spectrum of the nerve opticus is wide. The visual field deficits associated with skull base pathologies are: • Blindness, in cases of involvement of the entire nerve • Bitemporal hemianopsia, due to the compression of the optic chiasm caused by pituitary tumors extending cranially • Junctional scotoma: monocular central scotoma with contralateral supero-temporal field loss, due to a lesion at the optic nerve/chiasm border (see Fig. 10.2 on page 259). Pupillary reflexes: see Table 3.1. Typical skull base pathologies involving the optic nerve are pituitary adenomas, craniopharyngiomas, meningiomas, and trauma. The nerves involved in oculomotion are CNs III, IV, and VI (innervating the six extraocular muscles) (see also Chapter 2, Figs. 2.6 on page 22 and 2.13 on page 44). The oculomotor nerve has the following functions and attributes: • It innervates all the extrinsic muscles of the eye, except the lateral rectus and the superior oblique muscles: • It leaves the mesencephalon medially to the cerebral peduncle • It crosses the roof of the cavernous sinus and enters the orbit via the superior orbital fissure, where it divides into the following: Additional information about the oculomotor nerve: • The parasympathetic fibers originate from the Edinger-Westphal nucleus (in the mesencephalon), innervating the constrictor muscle of the iris, causing miosis, and the ciliary muscles, involved in the control of the shape of the lens (accommodation reflex). • Five segments of the nerve can be topographically defined: cisternal, petroclinoid, cavernous, fissural, and orbital.3 • The cavernous segment begins at the oculomotor triangle and runs to the superolateral wall of the cavernous sinus, where it reaches the superior orbital fissure. Surgical Anatomy Pearl The cisternal segment of the CN III, in the posterior fossa, always passes between the superior cerebellar artery and posterior cerebral artery. In the specific innervated extraocular muscles, with associated strabismus or diplopia, the following conditions can occur: • Lid drop (eyelid ptosis) and mydriasis. • Oculomotor palsies, which can be isolated or associated with other neuropathies (complex), can be complete or incomplete, and can have varying pupil involvement. • Complete oculomotor palsy: eye “down-and-out.” • Compressive lesions: sellar region and cavernous sinus tumors; cerebellopontine angle (CPA) tumors (meningioma, schwannoma) or aneurysms (of the posterior cerebral artery [PCA]), giving rise to compression of the parasympathetic fibers, which run peripherally to the nerve and can lead to ipsilateral fixed and dilated pupil. • Schwannomas of the oculomotor nerve have been described but are very rare. The trochlear nerve is the only nerve that originates dorsally to the brainstem. • The trochlear nerve is the smallest cranial nerve, with only 2,400 axons. • It runs into the lateral wall of the cavernous sinus and enters the orbit via the superior orbital fissure, above the annulus of Zinn, to innervate the superior oblique muscle. This muscle has a tendon that curves around on the trochlea of the orbit (hence the name of the nerve) to reach the superior part of the eye. Table 3.1 Anatomic Basis of the Cranial Nerve Reflexes
 Twelve Pairs of Cranial Nerves
Twelve Pairs of Cranial Nerves
Cranial Nerve I: Olfactory Nerve
 Lesions: anosmia/hyposmia
Lesions: anosmia/hyposmia
Cranial Nerve II: Optic Nerve
Vascularization
Lesions
Cranial Nerve III: Oculomotor Nerve
 Inferior rectus: depresses the eye
Inferior rectus: depresses the eye
 Superior rectus: elevates the eye
Superior rectus: elevates the eye
 Medial rectus: adducts the eye
Medial rectus: adducts the eye
 Inferior oblique: elevates the eye during eyeball adduction, or rotates it laterally when the eye is abducted
Inferior oblique: elevates the eye during eyeball adduction, or rotates it laterally when the eye is abducted
 Levator palpebrae superioris: raises the eyelid
Levator palpebrae superioris: raises the eyelid
 Superior branch: supplying the superior rectus muscle and the levator palpebrae superioris
Superior branch: supplying the superior rectus muscle and the levator palpebrae superioris
Lesions
Cranial Nerve IV: Trochlear Nerve
Function/Reflex | Anatomic Basis |
Emotional response to odors | CN I to medial olfactory stria to septal area/subcallosal gyrus |
Salivation with odors | CN I to lateral olfactory stria to piriform cortex to amygdala then via stria terminalis to hypothalamus then to superior and inferior salivatory nuclei (medulla) |
Accelerated peristalsis and increased gastric secretion with odors (“cephalic” phase of digestion or “gastrocolic” reflex) | CN I to lateral olfactory stria to piriform cortex to amygdala, then via stria terminalis to hypothalamus, then to dorsal motor nucleus of CN X (medulla) to CN X to GI tract |
Pupillary light reflex | CN II to retinopretectal tract to pretectum then via pretecto-oculomotor tract to bilateral Edinger-Westphal nuclei to CN III (parasympathetic) to ciliary ganglion to sphincter pupillae muscle |
Light-induced circadian rhythms | CN II to retinohypothalamic tract to suprachiasmatic nucleus (SCN) of hypothalamus |
“Near” reflex | 1. Pupillary constriction (miosis)—via bilateral Edinger-Westphal nuclei to CN III (parasympathetic) to ciliary ganglion to sphincter pupillae muscle 2. Lens accommodation—via bilateral Edinger-Westphal nuclei to CN III (parasympathetic) to ciliary ganglion to ciliary muscles (contraction causes lens to bulge, increasing diopter power) 3. Ocular convergence—via superior colliculus to bilateral CN III (medial rectus) |
Corneal reflex | CN V1 to principal sensory nucleus of CN V to CN VII to orbicularis oculi |
Jaw jerk (masseter reflex) | CN V3 sensory to mesencephalic nucleus of CN V to motor nucleus of CN V to masseter and temporalis |
Tearing | CN V1 to superior salivatory nucleus (medulla) to GSPN parasympathetics (initially in nervus intermedius) to pterygopalatine ganglion to lacrimal gland and mucosa of nose and mouth (palatal and nasal glands) |
Crying | Limbic system to hypothalamus to superior salivatory nucleus and lacrimal nucleus (medulla) to GSPN parasympathetics (initially in nervus intermedius) to pterygopalatine ganglion to lacrimal gland and mucosa of nose and mouth (palatal and nasal glands) |
Anterior two thirds of tongue to chorda tympani nerve (of CN VII) to geniculate ganglion to rostral nucleus solitarius to superior and inferior salivatory nuclei or posterior one third of tongue to CN IX to rostral nucleus solitarius to superior and inferior salivatory nuclei | |
Salivation | Superior salivatory nucleus to chorda tympani parasympathetics to submandibular ganglion to submandibular and sublingual glands; inferior salivatory nucleus to CN IX parasympathetics via tympanic nerve (Jacobson’s nerve) to LSPN to otic ganglion to parotid gland |
Sneezing | CN V sensory to the nucleus ambiguus to the respiratory center of the reticular formation, phrenic nerves, and intercostal muscles |
Acoustic reflexes | Mediated by CN VIII (cochlear nerve) to spiral ganglion to ventral cochlear nucleus to superior olivary complex to (1) both motor CN VII nuclei to the stapedius muscles to decrease amplitude of sound waves by reducing ossicle movement; and (2) both motor CN V nuclei to the tensor tympani muscles to decrease sensitivity of tympanic membrane by pulling it taut; reflex activated during loud sounds to protect cochlea and during speech production to decrease hearing of one’s own speech. |
Vestibulo-ocular reflex (VOR) | Keeps visual image still by compensating for horizontal eye movements; left head movement increases activity in left horizontal semicircular canal to CN VIII (vestibular nerve) to superior and medial vestibular nuclei to contralateral CN VI (stimulate right lateral rectus) and via medial longitudinal fasciculus to ipsilateral CN III (stimulate left medial rectus) |
Gag reflex | CN IX sensory to caudal nucleus solitarius to nucleus ambiguus to CN X to pharyngeal muscles |
Cough reflex | CN X sensory (usually larynx, trachea, or bronchial tree) to caudal nucleus solitarius to medullary respiratory center for forced expiration and to nucleus ambiguus to CN X to muscles of larynx and pharynx for cough |
Vomiting reflex | CN X sensory to caudal nucleus solitarius to nucleus ambiguus to CN X to close glottis and also to reticulospinal tract to cause contraction of diaphragm and abdominal muscles; may be stimulated also by increased intracranial pressure and by emetics stimulating the area postrema of caudal medulla |
Abbreviations: CN, cranial nerve; GI. gastrointestinal; GSPN, greater superficial petrosal nerve; LSPN, lesser superficial petrosal nerve.
Source: From Binder, Sonne, Fischbein. Cranial Nerves: Anatomy, Pathology, Imaging. New York: Thieme; 2010.
• The cisternal segment runs under the free edge of the tentorium, reaching the cavernous sinus below the petroclinoid ligament.
Lesions
Weakness of the downward movement of the eyeball and vertical diplopia can occur. Trochlear lesions are the most common cause of vertical strabismus. Excyclodeviation, the outer rotation of the globe, can be corrected by instructing the patient to tilt the head to the side opposite the paretic muscle. This paresis makes it very difficult to descend a staircase, for example, or read a newspaper.
• Lesions causing trochlear nerve palsy: trauma (especially orbit trauma), vascular compression, tumors (tentorial meningiomas, or the very rare trochlear schwannoma, which is generally cystic), and iatrogenic causes.
Cranial Nerve V: Trigeminal Nerve
At its origin is on the ventral surface of the pons, the trigeminal nerve has a major branch (portio major, which is sensory) and a minor radix (portio minor, which is motor). Both branches reach the semilunar ganglion (of Gasser), from which the nerve splits mediolaterally into three branches: the ophthalmic nerve (V1), the maxillary nerve (V2) and the mandibular nerve (V3). After exiting the lateral mid-pons level, the trigeminal nerve has a cisternal segment, a Meckel’s cave segment, and three peripheral divisions.
Segments
Cisternal Segment
The cisternal segment is a large sensory root (receiving somatosensory sensation from the entire face, except the angle of the jaw innervated by the cervical plexus) called the portio major and a smaller motor root called the portio minor. The trigeminal cistern surrounds the nerve; the superior petrosal vein complex lies in the cistern’s posterolateral space.4
Meckel’s Cave Segment
Meckel’s cave segment passes below the tentorial edge and superior petrosal sinus to reach the interdural layer of Meckel’s cave. The abducens nerve is inferomedial to the porus trigeminus. The cave is situated on the trigeminal impression of the bone at the petrous apex and is formed by a dural cleft from the posterior fossa to the posteromedial middle fossa. The arachnoid extends within the cave, forming a pocket along the rootlets of the nerve and the trigeminal ganglion (cistern around the ganglion). The greater superficial nerve is posterolateral to the Meckel’s cave.
Divisions
• V1 enters the lateral wall of the cavernous sinus running in the wall inferior to the trochlear nerve and into the orbit, via the superior orbital fissure, where further divisions occur:
 Lacrimal: It enters the orbit above the annulus of Zinn, innervating the lateral conjunctiva and skin near the lacrimal gland, as well as receiving postganglionic parasympathetic fibers (via the zygomatic and greater superficial petrosal nerve) for lacrimation.
Lacrimal: It enters the orbit above the annulus of Zinn, innervating the lateral conjunctiva and skin near the lacrimal gland, as well as receiving postganglionic parasympathetic fibers (via the zygomatic and greater superficial petrosal nerve) for lacrimation.
 Frontal: It reaches the orbit above the annulus of Zinn, dividing into the supraorbital nerve (for frontal sinuses, forehead) and supratrochlear nerve (forehead, side of the nose, medial conjunctiva, medial upper lid).
Frontal: It reaches the orbit above the annulus of Zinn, dividing into the supraorbital nerve (for frontal sinuses, forehead) and supratrochlear nerve (forehead, side of the nose, medial conjunctiva, medial upper lid).
 Nasociliary: It enters the orbit through the annulus of Zinn, branching into the infratrochlear nerve, anterior and posterior ethmoidal nerves, internal and external nasal nerves, long ciliary nerves (which also carry the sympathetic fibers from the internal carotid artery [ICA] to the dilator pupillae muscle), and short ciliary nerves (sensation for the globe, also carrying postganglionic parasympathetic fibers from the oculomotor nerve and ciliary ganglion to the sphincter pupillae and ciliary muscle).
Nasociliary: It enters the orbit through the annulus of Zinn, branching into the infratrochlear nerve, anterior and posterior ethmoidal nerves, internal and external nasal nerves, long ciliary nerves (which also carry the sympathetic fibers from the internal carotid artery [ICA] to the dilator pupillae muscle), and short ciliary nerves (sensation for the globe, also carrying postganglionic parasympathetic fibers from the oculomotor nerve and ciliary ganglion to the sphincter pupillae and ciliary muscle).
 Meningeal branches: for the dura of the anterior and middle cranial fossae, tentorium cerebelli, and cavernous sinus.
Meningeal branches: for the dura of the anterior and middle cranial fossae, tentorium cerebelli, and cavernous sinus.
• V2 runs in the inferolateral wall of the cavernous sinus, enters the pterygopalatine fossa via the foramen rotundum, and reaches the orbit via the inferior orbital fissure (infraorbital nerve).
 Branches in the pterygopalatine fossa (see Fig. 2.12)
Branches in the pterygopalatine fossa (see Fig. 2.12)
 Infraorbital nerve: It enters the orbit via the inferior orbital fissure, travels in a canal to exit on the splanchnocranium via the infraorbital foramen, where it innervates the midportion of the face. Branches of the infraorbital nerve are: alveolar nerves, inferior palpebral nerves, external nasal branches, and superior labial branches to the upper lip.
Infraorbital nerve: It enters the orbit via the inferior orbital fissure, travels in a canal to exit on the splanchnocranium via the infraorbital foramen, where it innervates the midportion of the face. Branches of the infraorbital nerve are: alveolar nerves, inferior palpebral nerves, external nasal branches, and superior labial branches to the upper lip.
 Zygomatic nerve: It enters the orbit via the inferior orbital fissure (IOF), to give rise to the zygomaticotemporal nerve (running in the lateral wall of the orbit and exiting through the zygomaticotemporal foramen). It innervates the lateral side of the forehead and the angle of the orbit. The zygomaticofacial nerve exits the zygomaticofacial foramen (which is a landmark in the orbitozygomatic approaches) to innervate the skin of the cheek and has postganglionic parasympathetic fibers for lacrimation.
Zygomatic nerve: It enters the orbit via the inferior orbital fissure (IOF), to give rise to the zygomaticotemporal nerve (running in the lateral wall of the orbit and exiting through the zygomaticotemporal foramen). It innervates the lateral side of the forehead and the angle of the orbit. The zygomaticofacial nerve exits the zygomaticofacial foramen (which is a landmark in the orbitozygomatic approaches) to innervate the skin of the cheek and has postganglionic parasympathetic fibers for lacrimation.
• V3 carries a sensory component and the motor component of the minor branch of CN V, exiting the base of the skull via the oval foramen. V3 gives rise to branches innervating the tensor muscle of velum palatinum and the tensor of the tympanum (the latter involved in the regulation of sound intensity).
 Meningeal recurrent branch, medial pterygoid nerve, masseteric nerve, deep temporal nerves, buccal nerve, lateral pterygoid nerve, auriculotemporal nerve, lingual nerve (for innervation of the mucosa of the mouth, gums, and anterior two thirds of the tongue, joined by the chorda tympani from the facial nerve, which also provides parasympathetic innervation to the submandibular gland), inferior alveolar nerve.
Meningeal recurrent branch, medial pterygoid nerve, masseteric nerve, deep temporal nerves, buccal nerve, lateral pterygoid nerve, auriculotemporal nerve, lingual nerve (for innervation of the mucosa of the mouth, gums, and anterior two thirds of the tongue, joined by the chorda tympani from the facial nerve, which also provides parasympathetic innervation to the submandibular gland), inferior alveolar nerve.
• The motor component innervates the chewing muscles (masseter; temporal, medial, and lateral pterygoid muscles; tensor tympani, involved in the acoustic reflexes; tensor veli palatini, involved in the mechanism of control of the pressure in the middle ear; mylohyoid; anterior belly of the digastric muscle).
Functions
The sensory branches of the trigeminal nerve carry touch, pain, thermal, and proprioceptive information from the whole face, conjunctiva, cornea, orbit, frontal sinuses, nasal cavity, palate, nasopharynx, and meninges.
Lesions
Hypo-anesthesia in somatic sensations, such as light touch, pain, or temperature, and paresthesias/dysesthesias can occur. The most common neurologic condition associated with the trigeminal nerve is trigeminal neuralgia, a lancinating pain in the specific territories innervated by the branches of CN V. The condition can be idiopathic, secondary to neurovascular compression (see Section 22.8, page 615), or secondary to tumors.
Motor Evaluation
With the mouth open, the jaw deviates toward the paralyzed side (due to the contralateral pterygoid muscle action).
Pathology
In the posterior fossa, tumors can affect the cisternal segments of the trigeminal nerve. In the middle cranial fossa, and extracranially, the nerve may be compressed/injured by tumors or trauma.
Cranial Nerve VI: Abducens Nerve
The abducens nerve innervates the lateral rectus muscle, which makes “abduction” (lateral movement) of the eye possible. The abducens nerve has the following attributes:
• It emerges from the lateroventral side of the brainstem, between the pons and medulla, medial to the facial nerve, therefore entering the cavernous sinus via the dura/periosteum on the lateral clivus and the Dorello’s canal in the petrous apex.
• In the cavernous sinus, it runs free, unlike the other intracavernous nerves, which are included in the meningeal lateral wall.
• It enters the orbit via the superior orbital fissure.
• Topographically, five segments can be identified: cisternal, gulfar, cavernous, fissural, and intraconal.5
Surgical Anatomy Pearl
The abducens nerve is therefore the only true intracavernous nerve! In the cavernous sinus it is lateral to the ICA and medial to V1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Inferior branch: supplying the medial rectus, inferior rectus, and inferior oblique muscles, as well as some parasympathetic fibers for the ciliary ganglion
Inferior branch: supplying the medial rectus, inferior rectus, and inferior oblique muscles, as well as some parasympathetic fibers for the ciliary ganglion Palatine nerves, posterior superior nasal nerve (to the septum and lateral wall of the nasal fossa, via the sphenopalatine foramen), orbital branches, pharyngeal branches.
Palatine nerves, posterior superior nasal nerve (to the septum and lateral wall of the nasal fossa, via the sphenopalatine foramen), orbital branches, pharyngeal branches.