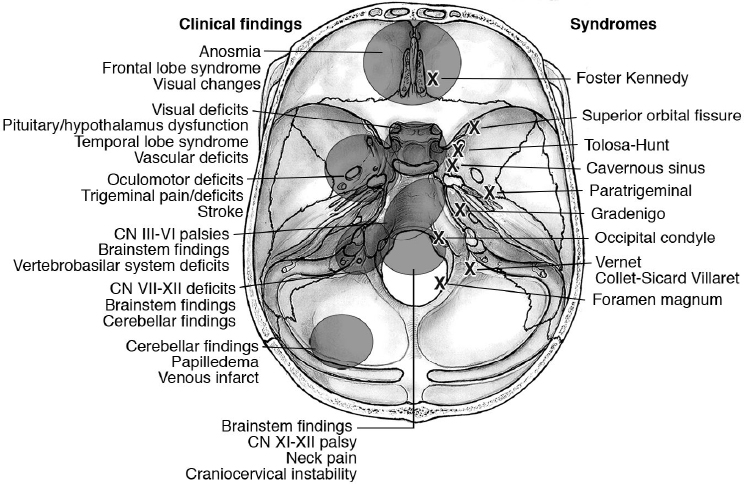
7 Clinical and Neurologic Findings in Skull Base Pathology A complete clinical and neurologic examination should be done in each patient affected by skull base pathologies. Tumoral compression or infiltration of the brain, hemorrhages, and contusions/lacerations should be investigated, as they can affect frontal, temporal, and occipital lobe function. The long pathways (motor and sensory system), cranial nerves and brainstem reflexes should be carefully examined. The main clinical features of skull base pathology are related to the anatomic localization demonstrated in Fig. 7.1. • Anosmia, frontal lobe syndrome (check neuropsychological testing as well), visual changes. • Check for involvement of the nasal/paranasal cavities (obstruction, epistaxis), orbits (diplopia, blindness, visual field loss, ophthalmoparesis, ophthalmodynia, dyschromatopsia), face (splanchnocranium fractures with skull base involvement, as in Le Fort III fractures). • Optic neuropathy (check for optic nerve and chiasm dysfunctions), cavernous sinus syndromes (ophthalmoparesis, trigeminal pain, etc.). • Check for pituitary/hypothalamus involvement. • Check for vascular involvement (arterial dissection, traumatic aneurysms, iatrogenic pseudoaneurysms, carotid-cavernous fistula). • Trigeminal dysfunctions (dysesthesia, pain, anesthesia), chewing deficits trismus • Proptosis, epistaxis • Cranial nerve involvement: all the neurologic deficits related to dysfunction of cranial nerves (CNs) III to XII • Brainstem corticospinal findings • Cerebellar findings • Uni/bilateral cranial neuropathies (e.g., CNs III to VI palsies) • Vertebrobasilar system-related deficits • Brainstem findings (e.g., rotating and progressive weakness, alternate syndromes) • CNs XI and XII palsies. • Suboccipital neck pain Examination Pearl Look for wasting of the trapezius (especially in slowly progressive lesions). • Brainstem/spinal cord findings • Craniocervical instability, occipital/suboccipital pain Examination Pearl Horner syndrome (also called Bernard-Horner syndrome), consisting of ptosis, miosis, enophthalmos, and anhidrosis, may be caused by several conditions affecting the skull base (Table 7.1). Table 7.1 Skull Base Conditions Causing Horner Syndrome
 Brain Involvement
Brain Involvement
 Clinical Features
Clinical Features
Anterior Skull Base
Middle Skull Base
Central/Paracentral
Lateral
Posterior Skull Base
Cerebellopontine Angle/Jugular Foramen
Clivus
Foramen Magnum
Craniocervical Junction
• Skull base/nasopharyngeal/orbit tumors/carcinomas • Skull base/middle ear infections • Skull base fractures • Internal carotid dissection (e.g., in trauma) • Endovascular procedures |
 Skull Base Syndromes
Skull Base Syndromes
Anterior Skull Base
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree