CHAPTER 4
Clinical Neuroanatomy
I. Skull, Cerebrovascular Supply, and Venous Drainage
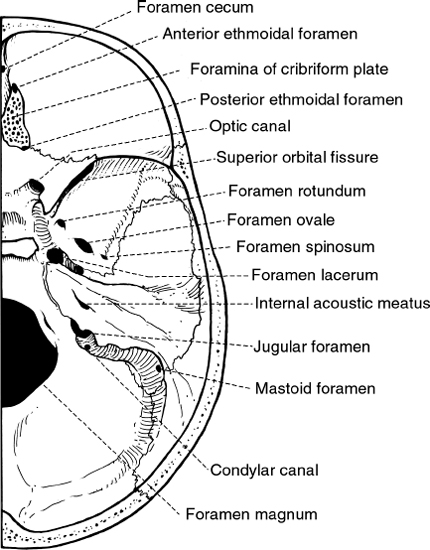
Figure 4.1 Basal view of the skull highlighting the foramina.
A. Foramina of the skull
FORAMEN | STRUCTURES |
Foramen cecum | Vein to superior sagittal sinus |
Anterior ethmoidal foramen | Anterior ethmoidal artery, vein, and nerve |
Foramina of cribriform plate | Olfactory nerve bundles |
Posterior ethmoidal foramen | Posterior ethmoidal artery, vein, and nerve |
Optic canal | CN II Ophthalmic artery |
Superior orbital fissure | CN III CN IV Ophthalmic nerve CN VI Superior ophthalmic vein |
Foramen rotundum | Maxillary nerve |
Foramen ovale | Mandibular nerve Accessory meningeal artery Lesser petrosal nerve (occasionally) Emissary veins |
Foramen spinosum | Middle meningeal artery and vein Meningeal branch of the mandibular nerve |
Foramen of Vesalius (inconstant) | Small emissary vein |
Foramen lacerum | Internal carotid artery Internal carotid nerve plexus |
Hiatus of canal of lesser petrosal nerve | Lesser petrosal nerve |
Hiatus of canal of greater petrosal nerve | Greater petrosal nerve |
Internal acoustic meatus | CN VII CN VIII Labyrinthine artery |
Vestibular aqueduct | Endolymphatic duct |
Mastoid foramen | Emissary vein Branch of occipital artery |
Jugular foramen | Inferior petrosal sinus CN IX CN X CN XI Sigmoid sinus Posterior meningeal artery |
Condylar canal (inconstant) | Emissary vein Meningeal branch of the ascending pharyngeal artery |
Hypoglossal canal | CN XII |
Foramen magnum | Medulla oblongata Meninges Vertebral arteries Spinal roots of CN XI |
B. Arterial supply
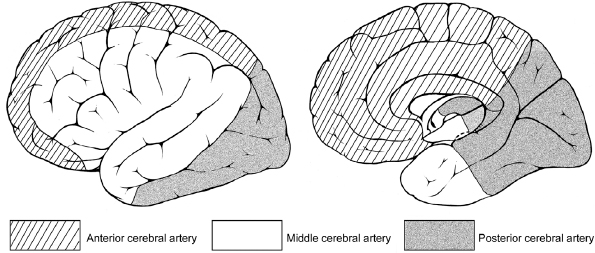
Figure 4.2 Sagittal view and section of the brain showing the major arterial supplies.
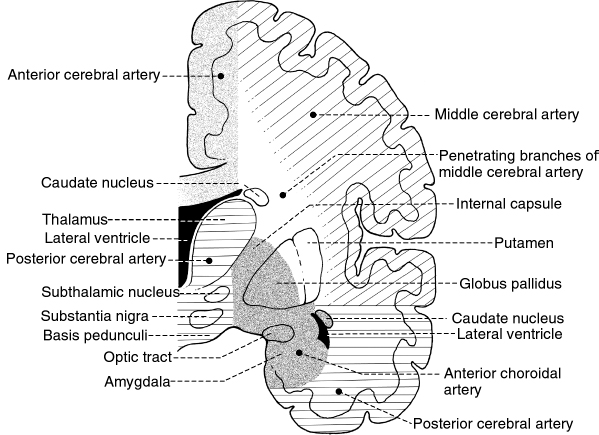
Figure 4.3 Coronal section of the brain at the level of the internal capsule and thalamus showing the arterial supply.
C. Venous drainage
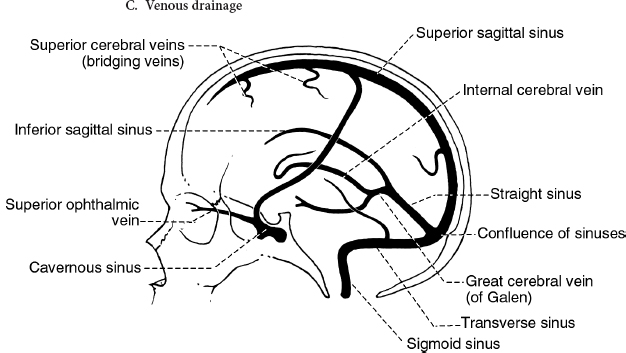
Figure 4.4 The venous system.
II. Cerebral Cortex: Thin gray covering of both hemispheres of the brain; two types: neocortex (90%) and allocortex (10%); motor cortex is the thickest (4.5 mm) and visual cortex is the thinnest (1.5 mm).
A. Layers of the neocortex: layers II and IV are mainly afferent; layers V and VI are mainly efferent.
1. Layer I: molecular layer
2. Layer II: external granular layer
3. Layer III: external pyramidal layer; gives rise to association and commissural fibers
4. Layer IV: internal granular layer; receives thalamocortical fibers from the thalamic nuclei of the ventral tier and also input from the lateral geniculate body
5. Layer V: internal pyramidal layer; gives rise to corticobulbar, corticospinal, and corticostriatal fibers; contains giant pyramidal cells of Betz (found only in the motor cortex)
6. Layer VI: multiform layer; major source of corticothalamic fibers; gives rise to projection, commissural, and association fibers
B. Functional areas
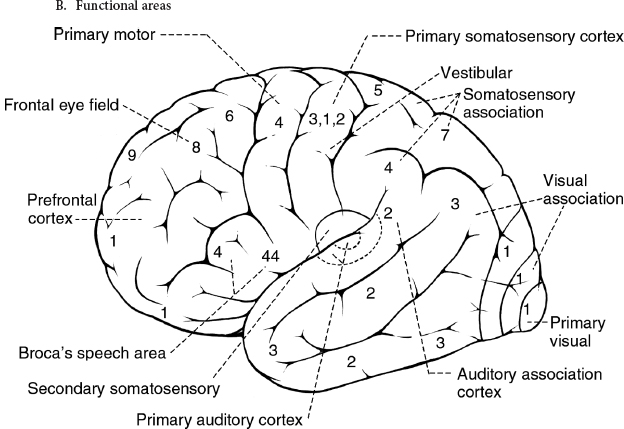
Figure 4.5 Gross lateral view of the brain illustrating the functional (Brodmann’s) areas.
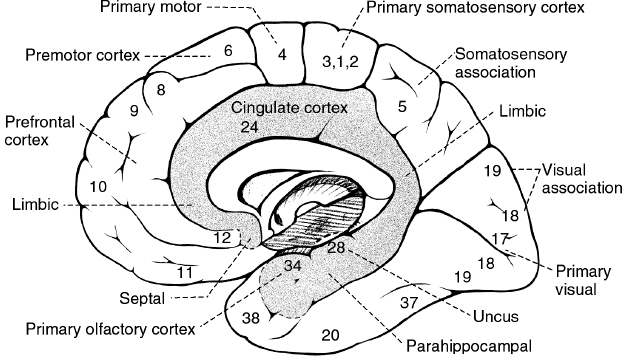
Figure 4.6 Medial surface of the brain hemisphere highlighting the functional (Brodmann’s) areas.
1. Frontal lobe
a. Motor cortex (Brodmann’s area 4) and premotor cortex (Brodmann’s area 6): destruction causes contralateral spastic paresis.
b. Frontal eye field (Brodmann’s area 8): destruction causes deviation of the eyes to the ipsilateral side.
c. Broca’s speech area (Brodmann’s areas 44 and 45): located in the posterior part of the inferior frontal gyrus in the dominant hemisphere; destruction results in expressive, nonfluent aphasia.
d. Prefrontal cortex (Brodmann’s areas 9–12, 46, 47): destruction of the anterior two-thirds results in deficits in concentration, orientation, abstracting ability, judgment, and problem-solving ability; destruction of the orbital (frontal) lobe results in inappropriate social behavior.
 NB:
NB:
Medial frontal cortex lesions may result in akinetic mutism, whereas orbitofrontal cortex lesions may result in impulsive and antisocial behavior. Left dorsolateral frontal lesions may produce depression.
2. Parietal lobe
a. Sensory cortex (Brodmann’s areas 3, 1, 2): destruction results in contralateral hemihypesthesia and astereognosis.
b. Superior parietal lobule (Brodmann’s areas 5 and 7): destruction results in contralateral astereognosis and sensory neglect.
 NB:
NB:
Asomatognosia is a form of neglect in which patients deny ownership of their limbs (also described as lack of awareness of the condition of all or part of one’s body). It frequently accompanies anosognosia (an inability or refusal to recognize a defect or disorder that is clinically evident). The lesion is located in the nondominant supramarginal gyrus (and/or angular gyrus).
c. Inferior parietal lobule of the dominant hemisphere: damage results in Gerstmann’s syndrome: (1) right-left disorientation, (2) finger agnosia, (3) dysgraphia (+/- dyslexia), (4) dyscalculia, possibly contralateral hemianopia, or lower quadrantanopia as well.
d. Inferior parietal lobule of the nondominant hemisphere: destruction results in topographic memory loss, anosognosia, construction apraxia, dressing apraxia, contralateral sensory neglect, contralateral hemianopia, or lower quadrantanopia.
3. Temporal lobe
a. Primary auditory cortex (Brodmann’s areas 41 and 42): unilateral destruction results in slight hearing loss; bilateral loss results in cortical deafness.
b. Wernicke’s speech area in the dominant area (Brodmann’s area 22): found in the posterior part of the superior temporal gyrus; destruction results in receptive, fluent aphasia.
c. Olfactory bulb, tract, and primary cortex (Brodmann’s area 34): destruction results in ipsilateral anosmia; irritative lesion of the uncus results in olfactory and gustatory hallucinations.
d. Hippocampal cortex (archicortex): bilateral lesions result in the inability to consolidate short-term memory into long-term memory.
e. Anterior temporal lobe (including amygdaloid nucleus): bilateral damage results in Klüver-Bucy syndrome—visual agnosia, hyperphagia, docility, hypersexuality.
f. Inferomedial occipitotemporal cortex: bilateral lesions result in the inability to recognize once-familiar faces (prosopagnosia).
4. Occipital lobe
a. Bilateral lesions: cortical blindness
 NB:
NB:
Individuals with Anton’s syndrome have cortical blindness, often with denial or unawareness of the blindness.
b. Unilateral lesions: contralateral hemianopia or quadrantanopia
5. Corpus callosum
a. Anterior corpus callosum lesions: may result in akinetic mutism or tactile anomia
b. Posterior corpus callosum (splenium) lesion: may result in alexia without agraphia
 NB:
NB:
Left posterior cerebral artery syndrome presents alexia without agraphia (often also have right homonymous hemianopia and achromatopsia and/or color anomia). The lesion is in the splenium of the corpus callosum.
 NB:
NB:
Surface dyslexia is characterized by impairment in linking the visual form system with the phonological output lexicon. Patients are therefore unable to access the visual word images to link to proper pronunciation and will need to rely on “print-to-sound conversion” and have difficulty reading words that do not sound the way they are spelled (e.g., words such as yacht and thought pronounced as spelled).
c. Split-brain syndrome: a disconnection syndrome that results from transection of the corpus callosum (e.g., in a patient with alexia in the left visual field, the verbal symbols seen on the right visual cortex have no access to the language centers of the left hemisphere)
III. Spinal Cord: An elongated, cylindrical mass of nerve tissue occupying the upper two-thirds of the adult spinal canal within the vertebral column; normally 42 to 45 cm long; conus medullaris: the conical distal end of the spinal cord; filum terminale: extends from the tip of the conus and attaches to the distal dural sac; it consists of pia and glial fibers and often contains a vein.
A. Segments and divisions: divided into 30 segments—8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and a few small coccygeal segments; cross sections show a deep anterior median fissure (commonly contains a fold of pia and blood vessels; its floor is the anterior/ventral white commissure) and a shallow posterior median sulcus; the dorsal nerve roots are attached to the spinal cord along the posterolateral sulcus; the ventral nerve roots exit the spinal cord in the anterolateral sulcus.
B. Gray matter
1. Columns: a cross section of the spinal cord shows an H-shaped internal mass of gray matter surrounded by white matter; made up of two symmetric portions joined across the midline by a transverse connection (commissure) of gray matter that contains the minute central canal or its remnants.
a. Ventral (anterior) gray column: contains the cells of origin of the fibers of the ventral roots
b. Intermediolateral gray column: position of the gray matter between the dorsal and ventral gray columns; a prominent lateral triangular projection in the thoracic and upper lumbar regions but not in the midsacral regions; contains the preganglionic cells of the sympathetic division of the autonomic nervous system
c. The dorsal gray column: reaches almost to the posterolateral sulcus; Lissauer’s tract: dorsolateral fasciculus, compact bundle of small fibers as part of the pain pathway
2. Laminas: a cross section of the gray matter shows a number of laminas (layer of nerve cells), termed Rexed laminas after the neuroanatomist who described them.
a. Lamina I: thin marginal layer, contains neurons that respond to noxious stimuli and send axons to the contralateral spinothalamic tract.
b. Lamina II: substantia gelatinosa; small neurons, some respond to noxious stimuli; substance P is the neuropeptide involved in pathways mediating sensitivity to pain, which is found in high concentration in laminae I and II.
c. Laminae III and IV: nucleus proprius; main input is from fibers that convey position and light-touch sense.
d. Lamina V: this layer contains cells that respond to both noxious and visceral afferent stimuli.
e. Lamina VI: the deepest layer of the dorsal horn and contains neurons that respond to the mechanical signals from joints and skin.
f. Lamina VII: a large zone that contains the cells of the dorsal nucleus of Clarke medially, as well as a large portion of the ventral gray column; Clarke’s column contains cells that give rise to the posterior cerebellar tract; also contains the intermediolateral nucleus.
g. Laminae VIII and IX: represent motor neuron groups in the medial and lateral portions of the ventral gray column; the medial portion contains the lower motor neurons (LMNs) that innervate the axial musculature; the lateral motor neuron column contains LMNs for the distal muscles of the arm and leg; in general, motor neurons for flexor muscles are located more centrally, whereas motor neurons for extensor muscles are located more peripherally.
h. Lamina X: represents the small neurons around the central canal or its remnants.
C. White matter
1. Columns: each lateral half of the spinal cord has white columns (funiculi)—dorsal (posterior), lateral, ventral (anterior); the dorsal column lies between the posterior median sulcus and the posterolateral sulcus (in the cervical region, it is divided into fasciculus gracilis and fasciculus cuneatus); the lateral column lies between the posterolateral sulcus and the anterolateral sulcus; the ventral column lies between the anterolateral sulcus and the anterior median fissure.
2. Tracts
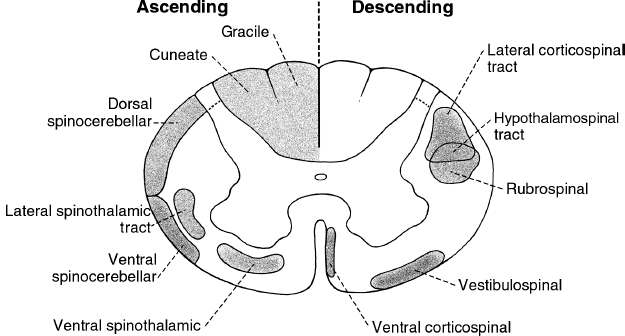
Figure 4.7 Cross section of the spinal cord highlighting the major ascending and descending tracts.
a. Descending tracts in the spinal cord
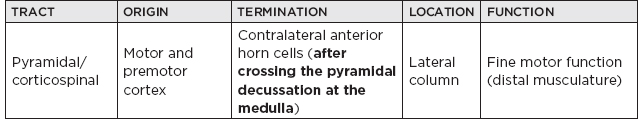
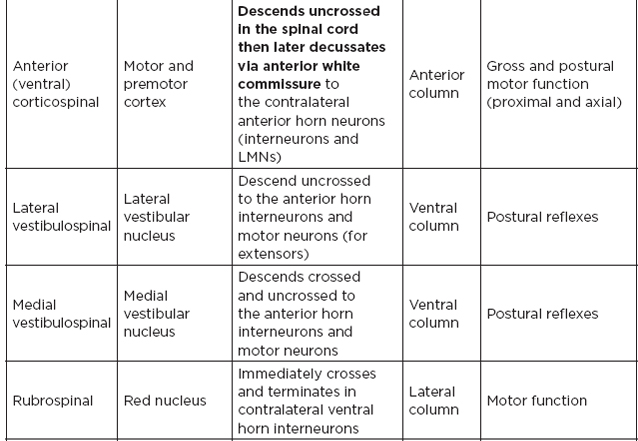
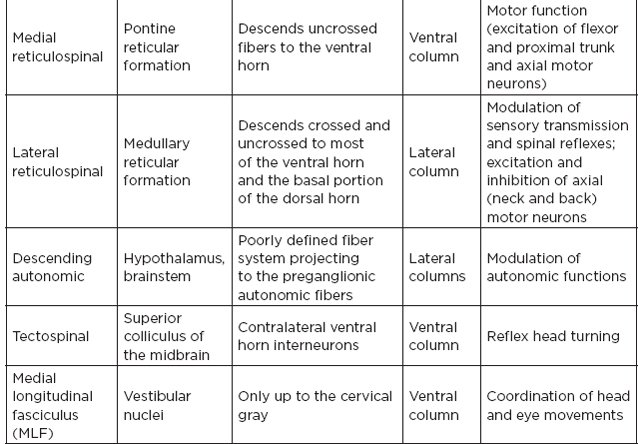
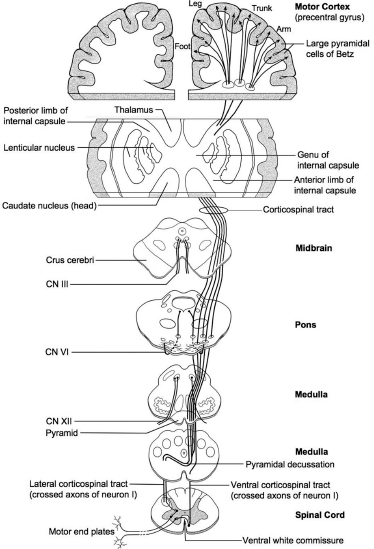
Figure 4.8 The route of the lateral corticospinal tract in the spinal cord from the motor and premotor cortex down to the contralateral anterior horn cells after crossing the pyramidal decussation at the medulla.
b. Ascending tracts of the spinal cord
 NB:
NB:
The dorsal and ventral spinocerebellar tracts are the most lateral tracts in the spinal cord and are most likely to be affected first from an extrinsic lateral insult.
D. Spinal cord syndromes
1. Small central lesion (e.g., syringomyelia): affects the decussating fibers of the spinothalamic tract from both sides without affecting other ascending or descending fibers, producing dissociated sensory abnormalities with loss of pain and temperature sensibility in appropriate dermatomes but with preserved vibration and position sense.
2. Large central lesion: in addition to the pain and temperature pathways, portions of the adjacent tracts, gray matter, or both, are affected, producing LMN weakness in the segments involved, together with upper motor neuron (UMN) dysfunction, and occasionally with joint position and vibration sense loss below the lesion.
 NB:
NB:
Central cord syndrome at the cervical levels may produce LMN findings in the upper extremities, UMN findings in the lower extremities, and a disturbance of pain and temperature sensation noticeable in the upper extremities.
3. Dorsal column lesion (e.g., tabes dorsalis): proprioception and vibratory sensation are involved, with other functions remaining normal.
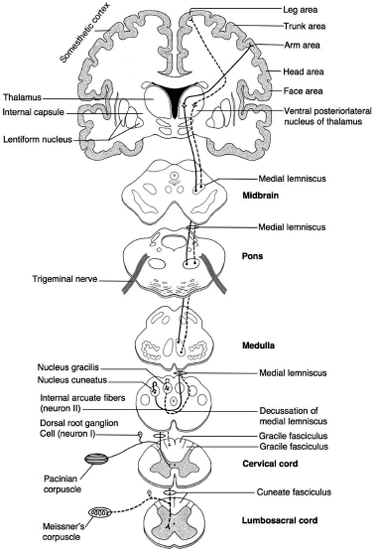
Figure 4.9 The route of the dorsal column system from the dorsal column nuclei to the contralateral thalamus to its termination in the sensory cortex.
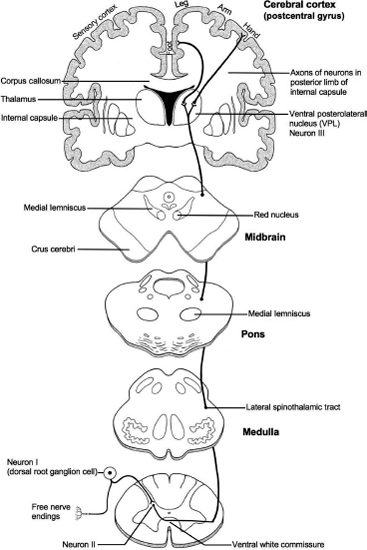
Figure 4.10 The route of the lateral spinothalamic tract from the nucleus in the dorsal horn through the contralateral thalamus to its termination in the sensory cortex.
 NB:
NB:
Examples of conditions presenting findings from dorsal column lesions include latent Treponema pallidum infection and vitamin B12 deficiency
4. Brown-Sequard syndrome: hemisection of the spinal cord as a result of bullet or stab wound, syrinx, tumor, hematomyelia, and so forth; signs:
a. Ipsilateral LMN paralysis in the segment of the lesion (damage of the LMNs)
b. Ipsilateral UMN paralysis below the level of the lesion (due to damage of the corticospinal tract)
c. Ipsilateral cutaneous anesthesia in the segment of the lesion (damage of yet uncrossed afferent fibers)
d. Ipsilateral loss of proprioceptive, vibratory, and two-point discrimination sense below the level of the lesions (damage of dorsal columns)
e. Contralateral loss of pain and temperature sense below the lesion (damage of spinothalamic tracts that have already crossed)
5. Subacute combined degeneration of the spinal cord: deficiency of vitamin B12 (cyanocobalamin) results in degeneration of dorsal and lateral columns; loss of position sense, two-point discrimination, and vibratory sensation; ataxic gait (damage to the spinocerebellar tracts), muscle weakness, hyperactive reflexes, spasticity of the extremities, and positive Babinski sign.
6. Spinal shock: acute transection of or severe injury to the spinal cord from sudden loss of stimulation from higher levels or from overdose of spinal anesthetic; all body segments below the level of the injury become paralyzed and have no sensation; all reflexes (including autonomic) are suppressed; usually transient; may disappear in 3 to 6 weeks followed by a period of increased UMN signs.
 NB:
NB:
Autonomic dysreflexia may occur in patients with lesions at T5, T6, and above. Symptoms include diaphoresis, hypertension, tachycardia, and others. If not treated promptly, death may result.
7. Combined UMN and LMN disease (e.g., amyotrophic lateral sclerosis): damage to the corticospinal tracts with pyramidal (UMN) signs and by damage to the anterior horn cells to produce LMN signs; no sensory deficits
 NB:
NB:
About 5%–10% of ALS is familial. Mutations in the C9orf72 gene are responsible for 30%–40% of familial ALS in Europe and the U.S. Superoxide dismutase (SOD1) gene mutations cause 15%–20% of familial ALS, and TARDBP and FUS gene mutations each account for ~5% of cases.
8. Ventral spinal artery occlusion: causes infarction of the anterior two-thirds of the spinal cord but spares dorsal columns and horns; damage to the following structures: lateral corticospinal tracts (bilateral spastic paresis with pyramidal signs below the lesion), lateral spinothalamic tracts (bilateral loss of pain and temperature sensation below the lesion), hypothalamospinal tract (at T2 and above, results in bilateral Horner’s syndrome), ventral (anterior) horns (results in bilateral flaccid paralysis of the innervated muscles), corticospinal tracts to the sacral parasympathetic centers at S2 through S4 (results in bilateral damage and loss of voluntary bladder and bowel control).
9. Cauda equina syndrome: for spinal roots L3 through coccygeal; results usually from a nerve root tumor (also ependymomas, dermoid tumor, or from a lipomas of the terminal cord); clinical: severe radicular unilateral pain; sensory distribution in unilateral saddle-shaped area; unilateral muscle atrophy; absent quadriceps (L3–L4) and ankle jerks (S1); incontinence and sexual functions are not marked (initially, at least); onset is often gradual.
10. Conus medullaris syndrome: for segments S3 through coccygeal; usually results from an intramedullary tumor, such as ependymomas; clinical: pain usually bilateral but not severe, sensory distribution in bilateral saddle-shaped area, muscle changes are not marked, quadriceps reflexes are normal (ankle jerk may be affected), incontinence and sexual functions are severely impaired, onset is often sudden and bilateral.
 NB:
NB:
The collateral blood supply at the T5 through T7 level of the spinal cord (SC) is relatively tenuous, making this “watershed” area most susceptible to ischemia.
IV. Peripheral Nerves
A. Brachial plexus: originates from the anterior rami of spinal nerves C5 through T1; variations are common.
1. Certain muscles of the shoulder girdle innervated by nerves that originate proximal to the formation of the brachial plexus; these muscles are important to evaluate clinically and by nerve conduction study/electromyography (EMG) when trying to determine if the lesion is at the level of the plexus or roots.
a. Serratus anterior: innervated by the long thoracic nerve (C5–C7)
b. Rhomboids: innervated by the dorsal scapular nerve (C5)
2. Trunks of the brachial plexus
a. Upper trunk: C5, C6; branches include:
i. Suprascapular nerve: innervates the supraspinatus and infraspinatus muscles
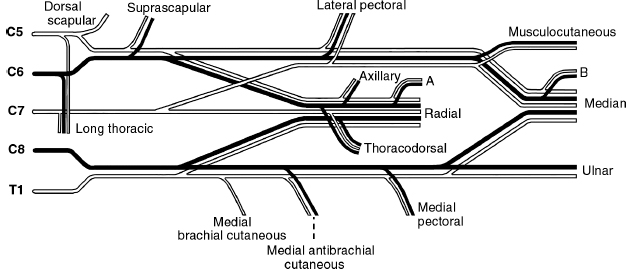
Figure 4.11 Schematic diagram of the brachial plexus. A, branch to extensor carpi radialis longus and brachioradialis; B, branch to flexor carpi radialis and pronator teres.
 NB:
NB:
The suprascapular nerve is susceptible to compression in the suprascapular notch.
ii. Nerve to the subclavius muscle: innervates the subclavius
b. Middle trunk: C7
c. Lower trunk: C8, T1
3. Cords of the brachial plexus
a. Lateral cord: formed by the anterior divisions of the upper and middle trunks (C5–C7); branches include
i. Part of the median nerve: supplies pronator teres, flexor carpi radialis
 NB:
NB:
The sensory supply to the median nerve derives from the lateral cord.
ii. Musculocutaneous nerve: supplies the biceps, brachialis, and coracobrachialis
iii. Lateral antebrachial cutaneous nerve (continuation of the musculocutaneous nerve): skin of the lateral forearm
iv. Branch to the pectoral nerve: supplies the pectoralis major
b. Medial cord: formed by the anterior division of the lower trunk (C8, T1)
i. Part of the median nerve: supplies the flexor digitorum superficialis, one-half of the flexor digitorum profundus, pronator quadratus, flexor pollicis longus, and 1st and 2nd lumbricals, abductor pollicis brevis, opponens pollicis, and one-half of flexor pollicis brevis (superficial head)
 NB:
NB:
Martin-Gruber anastomosis occurs in 15% to 30% of the population, consisting of a communicating branch from the median nerve to the ulnar nerve in the forearm to supply the first dorsal interosseous, and/or adductor pollicis, and/or abductor digiti minimi.
ii. Ulnar nerve: supplies one-half of the flexor digitorum profundus, flexor carpi ulnaris, 3rd and 4th lumbricals, interossei, adductor pollicis, abductor digiti minimi, opponens digiti minimi, and one-half flexor pollicis brevis (deep head)
iii. Medial cutaneous nerve: supplies the skin to the medial arm
iv. Medial antebrachial cutaneous nerve: supplies the skin to the medial forearm
 NB:
NB:
This nerve is a branch of the medial cord and would be expected to be injured in neurogenic thoracic outlet syndrome, and would be spared in an ulnar nerve mononeuropathy at the elbow.
v. Medial pectoral nerve: supplies the pectoralis major and minor muscles
c. Posterior cord: formed by the posterior division of the upper, middle, and lower trunks (C5–T1); branches include:
i. Upper and lower subscapular nerves: supplies the subscapularis and teres major
ii. Thoracodorsal nerve: supplies latissimus dorsi
iii. Axillary nerve: supplies the deltoid and teres major
iv. Radial nerve: supplies the triceps, brachioradialis, extensor carpi radialis longus, extensor carpi radialis brevis, anconeus, supinator, extensor digitorum communis, extensor carpi ulnaris, abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, and extensor indicis proprius muscles
v. Posterior antebrachial cutaneous nerve
4. Anatomic lesions of the brachial plexus
 NB:
NB:
Lesions in the brachial plexus will spare the paraspinal muscles at the corresponding levels.
a. Trunk lesions
i. Upper trunk lesion: Erb-Duchenne paralysis; nerves involved: suprascapular nerve (paralysis of the shoulder adductors/external rotators), C5, C6 portions of the lateral cord and posterior cord (paralysis of forearm flexors, elbow flexors, external rotators of the forearm), lateral antebrachial cutaneous nerve; clinical presentation: arm is adducted, internally rotated and extended (porter tip position) with sparing of the intrinsics, absent biceps/brachioradialis reflexes, absent sensation over the lateral forearm
ii. Lower trunk lesions: Klumpke’s paralysis—involves the C8, T1 portion of the medial cord; paralysis of the finger flexors and intrinsics; paresis of triceps and extensor digitorum communis (C8, T1 portion of the posterior cord); the arm is mildly flexed at the elbow and wrist, with a “useless” hand; may be accompanied by Horner’s syndrome
iii. Middle trunk lesions: rarely in isolation
b. Cord lesions
i. Lateral cord: weakness in the elbow and wrist flexors; sensory loss over the lateral forearm
ii. Medial cord: weakness in the hand intrinsics and partial weakness in long finger flexors; sensory loss over medial forearm
iii. Posterior cord: weakness in shoulder abduction and elbow/wrist/finger extensors; sensory loss over posterior aspect of the arm and hand
 NB:
NB:
Idiopathic brachial plexopathy (Parsonage Turner syndrome)—most common among young, healthy males; 25% preceded by a viral syndrome; symptoms include pain (severe at onset), weakness, paresthesias; elevated cerebrospinal fluid protein in 10%; two-thirds begin to improve by 1 month and two-thirds recover by 1 year.
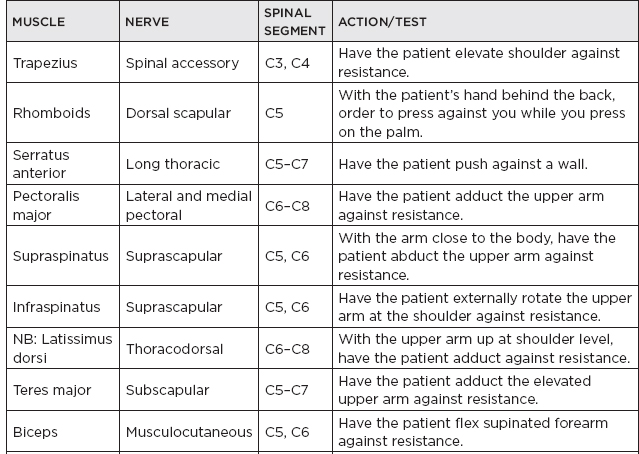
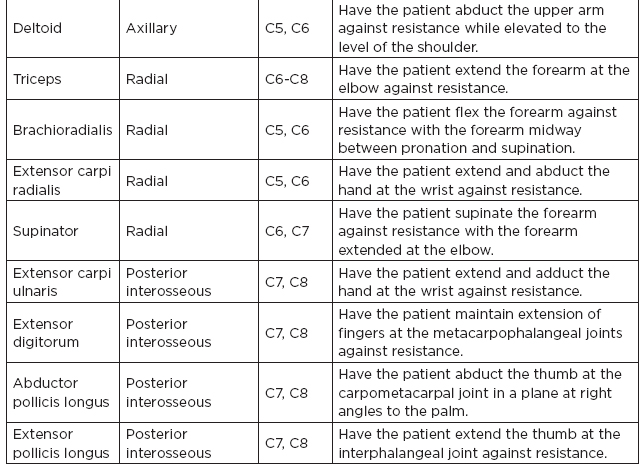
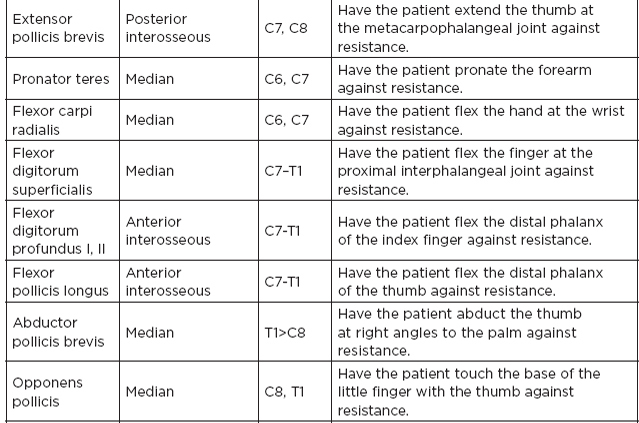
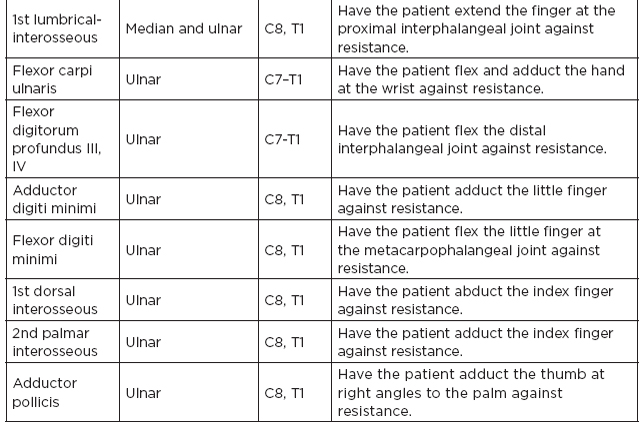
5. Muscles innervated by the brachial plexus
B. Median nerve: derived from the lateral cord (C5, C6) and medial cord (C8, T1) of the brachial plexus; passes between the two heads of the pronator teres muscle
1. Innervates: pronator teres, flexor carpi radialis, flexor digitorum superficialis, and palmaris longus muscles
2. Anterior interosseous innervation—flexor digitorum profundus (the radial half, i.e., the lateral two out of the four tendons), flexor pollicis longus, pronator quadratus
3. Branches to palmar cutaneous nerve, which supplies the skin of the proximal median palm; arises at the lower part of the forearm; travels superficial to the flexor retinaculum; therefore, this portion of the median nerve usually remains spared in carpal tunnel syndrome.
The median nerve passes through the carpal tunnel to innervate the abductor pollicis brevis, opponens pollicis, one-half of flexor pollicis brevis (superficial head), skin of the distal median palm and 1st through 3rd digits, and one-half of the 4th digit.
4. Clinical syndromes
a. Carpal tunnel syndrome: symptoms: pain, tingling, or burning in thumb, 1st two fingers, most prominent at night, aggravated by activities involving repetitive wrist action; clinical findings: thenar muscle weakness, sensory deficit, Phalen’s sign, Tinel’s sign (to percussion at wrist flexor crease); EMG/nerve conduction study (NCS): relative slowing of the conduction between the palm and wrist as compared to the adjacent ulnar nerve may be the most sensitive method of detecting carpal tunnel syndrome, the motor conduction and compound motor action potential amplitude are normal in the majority, unless severe disease.
 NB:
NB:
The median sensory nerve action potential is the most sensitive study for the detection of carpal tunnel syndrome. Motor studies are recorded over the abductor pollicis brevis.
b. Anterior interosseous nerve syndrome: symptoms: spontaneous onset or associated with vigorous exercise, pain over proximal flexor surface of the forearm but can be painless, weakness is a common complaint; clinical: tenderness over proximal flexor surface of the forearm, weakness of the flexor pollicis longus is most common, no weakness of the thenar muscles, no sensory deficit; etiology: accessory head of the flexor pollicis longus, fibrous origin or tendinous origin of the flexor digitorum superficialis to the long finger; EMG: abnormalities in the flexor pollicis longus, 1st and 2nd flexor digitorum profundus, and pronator quadratus sparing all other muscles, especially thenar groups
 NB:
NB:
Approximately one-half of the cases of Martin-Gruber anastomosis arise from the anterior interosseous nerve.
c. Pronator syndrome: symptoms: pain in the flexor muscles of the proximal forearm, paresthesias of the hand, symptoms worse with forceful pronation, weakness of grip is not a common complaint; clinical: tenderness over pronator teres, Tinel’s sign over site of entrapment, weakness is often slight, sensory deficit over the cutaneous distribution of the median nerve including the thenar eminence; etiology: hypertrophy of the pronator teres, fibrous band from the ulnar head of the pronator teres to the “sublimis bridge,” ligament from medial epicondyle to the radius; EMG/NCS: sparing of the pronator teres, abnormalities of other median innervated forearm muscles plus the thenar muscles, slowing of the conduction through proximal forearm distal latencies
d. Humeral supracondylar spur syndrome (ligament of Struthers): presents clinically like a pronator syndrome; aggravated by forearm supination and elbow extension, which may obliterate the radial pulse, the spur may be palpable, EMG abnormalities of all median nerve–innervated muscles, including pronator teres; supracondylar conduction abnormalities may be demonstrated
C. Ulnar nerve: derived directly from the lower trunk and medial cord (C8, T1) of the brachial plexus; in the midarm, it becomes superficial and reaches the groove behind the median epicondyle; it passes between the two heads of the flexor carpi ulnaris (cubital tunnel); runs down the medial forearm, innervating the flexor carpi ulnaris and the ulnar half of the flexor digitorum profundus.
1. Before entry into the Guyon’s canal, gives off two small branches: dorsal cutaneous (supplies the dorsal ulnar aspect of the hand) and palmar cutaneous (supplies the skin of the ulnar palm)
2. Within Guyon’s canal, gives off two branches: superficial branch to the skin over the distal ulnar palm and 5th digit and one-half of 4th digit, and deep branch to innervate adductor digiti minimi, opponens digiti minimi, flexor digitorum minimi, 3rd and 4th lumbricals, all interossei, one-half flexor pollicis brevis (deep head), adductor pollicis





