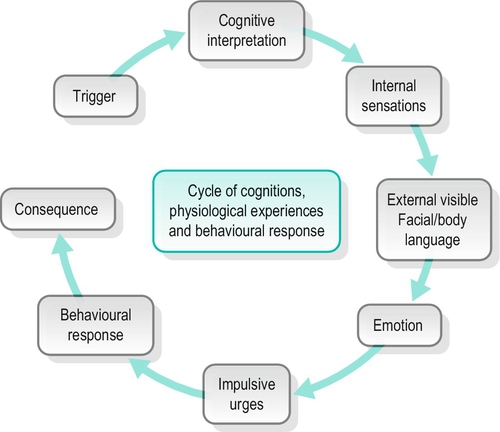
15 CHAPTER CONTENTS Acceptance and Commitment Therapy AN OVERVIEW OF THE THEORETICAL FRAMEWORK OF COGNITIVE BEHAVIOURAL THERAPY GENERAL CHARACTERISTICS OF COGNITIVE BEHAVIOURAL THERAPY The Cognitive Behavioural Frame of Reference in Occupational Therapy Occupational Therapy and Cognitive Functioning Assessing Cognitive Functioning: The Role of the Occupational Therapist Application of the Occupational Therapy Process The Oxford English Dictionary (2004) defines cognition as ‘the mental action or process of acquiring knowledge through thought, experience, and the senses’. Cognitive learning theories, therefore, describe ways in which the brain learns to interpret, store and recall information. Accordingly, it has been noted that cycles of both adaptive and maladaptive behaviours are developed on the basis of how an individual thinks and feels about their actions and their consequences (Hagedorn 2000; Segal et al. 2002) (see Fig. 15-1). FIGURE 15-1 The cycle of cognition. In the field of psychology, there has long been an understanding of the significant role of cognitions and the ways in which they influence human performance. Therefore, it is essential for occupational therapists to understand not only what is meant by cognition and cognitive impairment but also how cognitive deficits will directly affect occupational performance. This chapter describes how cognitive impairment can present in mental health practice, considers the effect of the impairment on occupational performance and participation, and explores cognitive interventions. An overview of psychological approaches, assessments and case presentations of interventions will assist readers in integrating theory into practice. There are two primary areas in which cognitive impairment can have a significant effect on occupational performance: organic brain syndrome and mental health problems. Organic brain syndrome is the term used to describe a range of disorders in which an underlying neurological dysfunction causes problems with attention, concentration and memory. The individual may also appear confused, anxious and/or depressed, as a result of damage to, or disease in, the brain. These disorders include, acquired brain injury (traumatic), cardiovascular disease (strokes, vascular dementia) and degenerative disease (Creutzfeldt–Jacob disease and Huntington’s disease). Since these disorders are of a more physical nature, this chapter will not expand further but will focus on problems commonly encountered in mental health practice. This section introduces a range of mental health problems that are likely to present with elements of cognitive impairment, and begins to describe the impact of this on functioning. Affective spectrum disorder is the overarching term to describe a wide range of mental health problems which include those typically associated with intense changes in mood or extremes of mood-affecting thoughts and behaviours, such as depression, bipolar disorder and general anxiety disorders. Some individuals with affective disorder may also experience psychotic episodes, including delusions, hallucinations or other losses of contact with reality, although this is not necessarily so in all cases (Forty et al. 2009; Mazzarini et al. 2010). Individuals who experience anxiety disorders may experience problems in their functional performance, as a result of cognitive impairment due to attention deficits and memory difficulties (Ferreri et al. 2011). Routine and roles may be lost during significant mood changes and due to the self-critical judgements often prominent in depression. With anxiety disorder, worrying has a tendency to be overwhelming and affects daily life, interfering with routine activities, including job roles and social life. There has been a significant increase in both the understanding of autism and Asperger syndrome and in the number of individuals diagnosed with Autistic Spectrum Disorder (ASD). Limited space within this chapter allows only the elements of cognition and cognitive impairment to be discussed and readers are encouraged to explore ASD further elsewhere (see Frith 1991, 2003; Frith and Hill 2004). The term spectrum disorder implies a vast range of symptoms that may be present and the difficulties an individual may experience, which can vary from mild to very severe. There may also be a co-existing learning disability and the need for long-term support with specialist intervention. Autism and Asperger syndrome both develop in early life and persist throughout adulthood, affecting three areas of neurological development: communication, social interaction and creativity (Frith and Hill 2004). The cognitive impairment can be wide ranging from severe learning disabilities to high cognitive functioning. Consequently, individuals with ASD will require comprehensive assessment and the amount of support will depend on the level of functioning. Dementia is a disorder in which there is a progressive decline in the cognitive functioning of an individual outside of the normal ageing process – such as in Alzheimer’s disease (APA 2000). Dementia is characterized by multiple cognitive deficits including memory loss, attention deficit and disorientation of people, place and time. Individuals with dementia also experience difficulties with problem solving, a decline in their ability to learn new things and often their speech and language ability are impaired. Psychosis has become the overarching term for a number of mental health problems, including schizophrenia, bipolar disorder and schizoaffective disorder. The term ‘psychosis’ describes a set of symptoms that include delusions, hallucinations (usually auditory or visual but may be other sensory modalities also), disorganized speech and confused or disturbed thoughts with a loss of contact with reality (APA 2000). These symptoms may also be apparent in some forms of dementia, epilepsy, Parkinson’s disease and as a result of occasional or continual alcohol or substance misuse. People living with psychosis frequently experience a range of cognitive deficits, which impact on their functional ability, including attention deficits, memory problems and problem-solving skills. There may also be the additional cognitive impairment where alcohol or substance misuse problems co-exist (see Ch. 28). Personality-disordered individuals may experience transient psychotic episodes, including ‘transient, stress-related paranoid ideation or severe dissociative symptoms’ (APA 2000). These individuals may also experience periods of intense flashbacks and heightened emotional dysregulation that may have a similar presentation to psychotic episodes. Emotion dysregulation is an inability to regulate emotions, particularly negative emotions, and a high sensitivity to emotional stimuli with a slow return to an emotional base line (Linehan 1993a). Consequently, there may be cognitive deficits which will impact on individuals’ functional capacity in similar ways to those described previously, although these may be of a shorter duration: Emotions, in turn usually have important consequences for subsequent cognitive, physiological and motor behaviour. (Linehan 1993a, p. 38) Much of the work in developing cognitive behaviour therapy stemmed from the theory that a person’s clinical depression or anxiety problems were closely linked to their cognitions, thinking patterns and beliefs. Cognitive behaviour therapy has been further developed to include dialectical behaviour therapy and mindfulness-based cognitive therapy, both of which will be of interest and relevance to occupational therapists and will be discussed in more detail later. Cognitive behavioural therapy (CBT) was developed by Aaron Beck in the 1960s, as short-term psychotherapy for depression (Beck 1964, 1991). Further work by Beck, in the 1970s and 1980s highlighted that the way we think about ‘self’, the world and others, has a major impact on both our emotions and behaviour (Beck 1976). CBT is now widely used as an evidence-based psychotherapeutic approach, based on the theoretical framework of behaviour therapy and cognitive therapy and is now the preferred approach for addressing many other mental health problems (DH 2012), including obsessive compulsive disorder, general anxiety disorder, substance misuse, eating disorders and post-traumatic stress disorder (PTSD) (Beck 1995). A detailed examination of the theory and practice of CBT follows later in this chapter. Contemporary CBT has developed significantly over the last few decades and now encompasses additional theoretical frameworks, referred to as the third wave of behaviour therapy (Hayes 2005). The more recent additions to CBT include dialectical behaviour therapy (DBT) (Linehan 1993a); acceptance and commitment therapy (ACT) (Hayes et al. 1999); mindfulness-based cognitive therapy (MBCT) (Segal et al. 2002); and mindfulness-based stress reduction (MBSR) (Kabat-Zinn 1991); all of which provide further evidence-based therapies. This new generation of therapies is no longer necessarily the domain of psychology, which was the profession originally providing CBT. There are now many other clinical professions utilizing CBT approaches in their therapy, including occupational therapists (Duncan 2003). Another cognitive approach developed by Jeffrey Young in the mid-1980s is schema therapy, which focuses more specifically on the individual’s schema and changing behavioural responses (Young and Klosko 1993; Young et al. 2003). Schema are described as the emotional and cognitive patterns that developed early in life and which then repeat throughout life; they include memories, emotions, cognitions and internal body sensations. The goal of this therapy is to assist individuals to stop using maladaptive coping strategies, to get in touch with their core feelings and to detach from their self-defeating schema. What follows is an overview of the new generation of cognition-based therapies. Dialectical behaviour therapy (DBT) was originally developed by Marsha Linehan (1993a), as a comprehensive cognitive behavioural approach ‘for the treatment of chronically suicidal individuals’ (Dimeff and Linehan 2001, p. 10) who also met the criteria for borderline personality disorder (BPD). It has also now been extended to other mental health problems, including substance misuse, eating disorders and suicidal/depressed adolescents. DBT is used in community settings, in hospital settings and prisons. It differs from CBT, in that it combines the basic behavioural techniques with Eastern mindfulness practices. Mindfulness is the awareness that emerges through paying attention on purpose, in the present moment, and non-judgementally to things as they are. (Williams et al. 2007, p. 47) Linehan (1993a) recognized that severe emotion regulation problems led to cognitive distortions, automatic assumptions, rigid beliefs and dichotomous thinking. It also became apparent that there were many dilemmas facing both individuals with BPD and their therapists, including a lack of understanding of the nature of BPD, poor therapeutic relationships, frequent therapist burnout and limited change in inappropriate behaviours. Consequently, Linehan (1993a) ensured that the treatment package included individual therapy, group skills training and a weekly consultation for the therapists. Thus ensuring there was an educative element, consistency, therapist support and adherence to DBT principles. Occupational therapists will recognize the strengths of DBT and particularly identify with the skills training modules which are, in essence, skills for life, and will see this format as comparable with skills training in occupational therapy. Acceptance and commitment therapy (ACT) is a mindfulness-based behavioural therapy, which differs from traditional CBT in that, rather than trying to teach people to have greater control of their thoughts, feelings, sensations and memories, it teaches them to notice thoughts and judgements and to accept situations as they are, in the moment. Similar to CBT, it involves experiential exercises and values guided behavioural interventions (Harris 2008). Mindfulness-based cognitive therapy was developed as a therapeutic approach by Segal et al. (2002), in response to the need for an effective, evidence-based treatment and relapse prevention method for depression. Similar to CBT, it is time-limited, collaborative, requires active participation of the service user, explores new ways of thinking and experiencing and the acceptance of things as they are, in the moment. It consists of an 8-week programme based on the stress reduction programme for the management of pain using mindfulness meditation (Kabat-Zinn 1994). Kabat-Zinn (2004) initially developed the mindfulness-based stress reduction (MBSR) programme for individuals with chronic pain in the USA and, following the success of the 8-week programme, extended it to other chronic physical or life-limiting illnesses where stress and pain were intrinsically linked together. As above, this approach consists of experiential mindfulness exercises, active collaboration and commitment from participants. The mindfulness-based approaches have been welcomed by many professions, not only as a treatment approach for service users but also as a stress-reduction programme for staff. Such is the wide recognition of the MBSR programme that it is also used in the corporate world for stress reduction of staff (Fries 2007). Schema therapy involves two phases of treatment. The first phase focuses on helping the individual identify schemas, to understand their origin in both childhood and adolescence and then to relate them to the current problem. The second phase uses cognitive, experiential/behavioural and interpersonal strategies to ‘heal’ schemas and to replace maladaptive coping strategies with more adaptive/appropriate behavioural responses (Young et al. 2003). Other cognitive approaches with people with a primary diagnosis of schizophrenia are beginning to gather momentum. McGurk et al. (2007) and Roberts and Penn (2008) have explored the relationship between the introduction of a cognitive intervention and changes in cognitive functioning in individuals with schizophrenia. Cognitive remediation therapy (CRT) (McGurk et al. 2007) and social cognition and interaction training (SCIT) (Roberts and Penn 2008) show evidence of improvement in cognitive functioning, notably memory – which has an impact on occupational participation and performance. This kind of research is still in its infancy but if the evidence demonstrates that the use of cognitive approaches is able to effect change and improve quality of life for individuals then occupational therapists are well placed to contribute to this research agenda. Occupational therapists may also benefit from exploring the effect of combining cognitive work with psychosocial education and regular occupational therapy interventions focusing on structure and meaningful occupation and life roles (Creek and Lougher 2008). While accepting the extensive influence of CBT, DBT, ACT, MBSR and increasingly MBCT, it is fundamental to the professional identity of occupational therapists that they maintain their core occupational focus. Duncan (2006) challenged the use of CBT by occupational therapists but also recommended the use of cognitive behavioural principles within an occupational therapy context (Duncan 2003). To this end, the following section will discuss the theoretical framework of CBT. CBT combines both cognitive and behavioural techniques. Behaviour therapy was developed from work by the Russian physiologist, Ivan Pavlov, in the 1920s, based on animal behaviour in which he identified, through experimentation, how behaviours could be influenced by the environment; this became known as classical conditioning (Hawton et al. 1998). Building on this early work, American psychologist BF Skinner recognized that it was possible to increase or decrease the frequency of the behaviour occurring, depending on the specific event immediately following the behaviour. Skinner realized that both positive and negative consequences could reinforce the behaviour. He referred to this as operant conditioning (Hawton et al. 1998). This traditional behavioural approach was widely acknowledged in mental healthcare over the 1970s and 1980s. In recognition of the importance of increasing the appropriate behaviours and decreasing inappropriate behaviours, the ‘RAID’ (reinforce appropriate, implode disruptive) approach to the management of extreme behaviour (Davies 2001) was developed using contingency management as the key component. The term ‘implode’, here, literally means to cause to collapse inwards, because the intent is to discourage disruptive behaviour by ignoring or giving minimal response to it. Contingency management is based on the fact ‘that the consequences of our behaviour influence what we learn’ (Koerner 2012, p. 104), thus how one responds to either appropriate or inappropriate behaviour will influence the likelihood of the behaviour recurring. As a result, many therapeutic programmes may now include it as a behavioural treatment approach, not only to enhance the effectiveness of CBT but also to assist the staff working in a more positive and constructive therapeutic manner with a complex and challenging patient group (Long et al. 2008). CBT involves behavioural experimentation. This requires the individual to practice new behaviour changes learnt within therapy or through using a CBT workbook. It is collaborative, involving full and active participation of the client and therapist. Indeed, there is great emphasis placed on this therapeutic relationship, which is perceived to be integral to the outcome of therapy. CBT focuses on five key areas: thoughts, behaviours, emotion/mood, physiological responses and the environment. Each of the five areas impacts on the other areas. CBT focuses on the fact that by changing one’s thinking, one can change one’s emotions and the responses one makes (Greenberger and Padesky 1995). Beck et al. (1979) identified three levels of cognition: full consciousness, automatic thoughts, and core schema. Full consciousness is defined as a state in which rational decisions are made with full awareness. Automatic thoughts are those that ‘pop into one’s head’. In healthy individuals, they can be either positive and constructive or negative and judgemental. In depression, these thoughts are more frequently negative, critical and often illogical and are known as ‘negative automatic thoughts’ (NATs). Conversely, in anxiety disorders, automatic thoughts often involve overestimation of risk in situations and underestimation of ability to cope (Wright et al. 2003). It is important to recognize these automatic thoughts when assessing the individual, since they will frequently have a direct effect on how they manage their daily routines. When automatic thoughts inappropriately impact an individual’s behaviour, the therapist can begin to challenge the thoughts with the individual and encourage new alternative ways of thinking. This involves trying new approaches to different situations and environments. Linehan (1993b) describes ‘acting opposite to the current emotion’, which involves observing one’s thoughts, judgements and acting opposite to the emotion. For example, when feeling frightened – unless there is a real threat to one’s life – this would mean noticing the thoughts and judgements arising in the situation, but then approaching, rather than avoiding the fear-inducing situation. This process is not the same as simply turning negative thoughts into positive thoughts. Challenging automatic thoughts is about gaining a wider perspective of situations, looking at new alternative views and identifying solutions to overcome problems. Schemas are at the deepest level of one’s thinking, as described earlier. They are absolute core beliefs which are shaped in early life and which continue to affect the way we see the world and see ourselves. Schemas are usually more difficult to challenge, given the length of time they have been held as fact. They may indeed be so entrenched that we are unaware of them. Consequently, they will affect our self-esteem and coping strategies. Such beliefs may include ‘I am bad’, or ‘I am good’, or ‘I am a horrible person’. Since schemas play such a major role in regulating an individual’s self-worth and subsequent behavioural coping strategies, they become a necessary focus for CBT interventions (Young and Klosko 1993). Current attention within CBT now focuses attention less on the levels of cognitions and more on the following phenomena – as depicted in Figure 15-1. ■ Trigger: the event prompting the cognitive response ■ Thoughts: the interpretations, assumptions and judgements that follow ■ Emotions ■ Behaviour. CBT has four characteristics that set it apart from other psychotherapeutic approaches, as follows: 2. It is time limited. There is an agreement between the individual and the therapist regarding the duration of treatment and the times for evaluating/reviewing therapy 3. It is collaborative intervention. Both the therapist and the individual work together to develop a shared understanding of the presenting problems and actively seek more effective ways of coping 4. It is problem-focused. The therapist identifies the individual’s problems and then arranges them (through negotiation with the service user) in hierarchical importance, in order to define a list of priorities and establish the focus of interventions. There is an on-going assessment process following the initial assessment, which includes gathering historical information, as well as current information regarding the presenting problem. A case formulation is generated collaboratively with the service user and their interpretations of their presenting problems, as well as using research and theory. In order to ensure therapeutic openness and clarity, psycho-education regarding CBT is provided for the service user. Following this, the interventions are agreed. These may involve individual work and activity-based work, such as exposure therapy, whereby an individual with agoraphobia, for example, may start with the small step of simply going out of the door but progress later to taking a bus into town. This engagement with specific activities underlines the close association that CBT has with occupational therapy. At the conclusion of the intervention, the therapist aims to empower the individual to become their own therapist, recognizing their triggers and developing their own coping mechanisms in order to establish relapse prevention strategies. In highlighting the general characteristics of CBT and in recognition of the third wave of behaviour therapies, it is unsurprising that many occupational therapists are attracted to the cognitive behavioural approach. It is therefore helpful to consider how CBT and occupational therapy can be integrated effectively. The term ‘cognitive behavioural therapy’ (CBT) is often loosely used in occupational therapy, which then leads to confusion and frustration for both occupational therapists and cognitive behavioural therapists. Duncan (2006) recognized this dilemma and suggested that ‘all forms of primarily didactic psychotherapy that use a CBT approach are referred to as CBT (or cognitive behavioural therapy), while the use of cognitive behavioural theory or practice within occupational therapy is referred to as employing a cognitive behavioural frame of reference’ (p. 225). Frames of reference, or approaches, provide a theoretical knowledge base that underpins therapeutic interventions, enabling the therapist to structure and evidence their intervention. The cognitive behavioural frame of reference provides a psychological structure but requires an additional specifically occupational perspective to assess or identify an individual’s occupational performance or functional ability. Certain occupational therapy models of practice recognize the value of combining frames of reference or approaches to gain greater insight into individuals’ problems and deficits. Forsyth and Kielhofner (2006), for example, stated that ‘occupational therapists using the Model of Human Occupation (MOHO) will also need to use other frameworks in order to understand and address performance capacity’ (p. 85). A combination of frameworks can therefore be used to support a fuller understanding of an individual’s occupational participation, and the cognitive behavioural theory is one such framework. However, it is imperative that occupational therapists use it with a clear appreciation of how they are integrating occupational and cognitive behavioural perspectives to understand an individual’s needs. Integrating assessment information and formulation will indicate areas for intervention. The occupational therapist and the individual must then work together to prioritize goals for therapy. Agreeing these can be a first step in the development of the therapeutic relationship, with the implicit aims being to understand each other’s formulation of presenting difficulties and to agree a way forward. Identifying levels of cognitive functioning should be undertaken through careful assessment of the individual’s presenting problems, developing an understanding of past functioning, along with current challenges. Using the knowledge of the past level of functioning, current context and future aspirations, the occupational therapist can work with the individual to clarify the impact of the impairment on a person’s occupational functioning. In terms of cognitive functioning, various occupational therapy models of practice have attracted attention over time, as the evidence base has developed. While Claudia Allen’s early Cognitive Disability Model and the later Functional Information Processing Model (Allen 1982; Allen et al. 2007) have been widely adopted in the USA, it has been suggested that limitations exist regarding their application in the UK, linked to the associated craft element and the fact that the terminology/instructions are American and differ from those generally used in the UK. Availability of the assessments has been problematic but they are now more readily available via websites (Pool 2006, p. 140). Similarly, the Model of Creative Ability (de Witt 2005), developed by Vona du Toit in the 1970s, has been widely used in South Africa but its use has only recently started to gain momentum in the UK (see Ch. 17 for a detailed look at this model). The Model of Human Occupation (MOHO) (Kielhofner 2008), which supports a person-centred approach and has a wide range of assessment tools and measures that have been developed to enhance the models application, has been used effectively in cognition-orientated practice (Lee and Harris 2010; Lee et al. 2011). The assessment of cognitive functioning is complex and a range of generic assessment tools exists to structure this process. The method of assessment is often through asking a range of questions for which the tools, such as The Occupational Circumstances Assessment Interview Rating Scale (Forsyth et al. 2005) and the Assessment of Motor and Process Skills (Fisher 2003, 2006), provide a range of standardized responses; or by carrying out specific tasks that have been standardized to provide a score system and a context to the scoring (Fisher 2003, 2006). For occupational therapists, the focus is on performance during meaningful occupation. It is also important that the therapist maintains an awareness of performance adaptation and the potential for a service user to disguise the impact of cognitive impairment on occupational performance where, for example, they may have achieved the desired outcome but modified or missed tasks in the process. This type of observational information can help the occupational therapist formulate the strengths and needs when developing an intervention plan. While unstructured observational assessments may be adequate and easy to carry out, there are several structured and standardized tools which can be used if more detailed information is required (see Table 15-1). Some use an observational or self-rating format, while others include a standardized database to allow for results moderation. Occupational therapists also use explorative questioning to enhance the information available; often speaking (with consent) to family and carers, as well as the individual.
Cognitive Approaches to Intervention
INTRODUCTION
COGNITIVE IMPAIRMENT
Organic Brain Syndrome
Mental Health Problems
Affective Spectrum Disorder
Autistic Spectrum Disorder
Dementia
Psychosis
COGNITIVE APPROACHES
Cognitive Behavioural Therapy
Dialectical Behaviour Therapy
Acceptance and Commitment Therapy
Mindfulness-Based Approaches
Schema Therapy
AN OVERVIEW OF THE THEORETICAL FRAMEWORK OF COGNITIVE BEHAVIOURAL THERAPY
GENERAL CHARACTERISTICS OF COGNITIVE BEHAVIOURAL THERAPY
The Cognitive Behavioural Frame of Reference in Occupational Therapy
Occupational Therapy and Cognitive Functioning
Assessing Cognitive Functioning: The Role of the Occupational Therapist
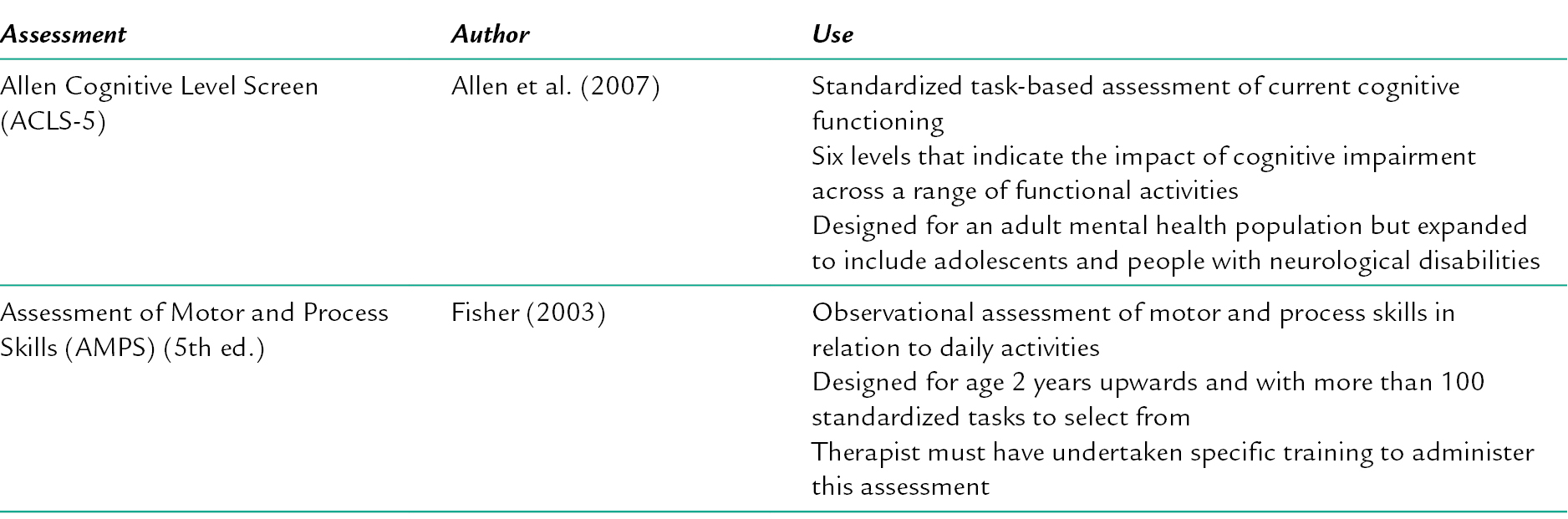
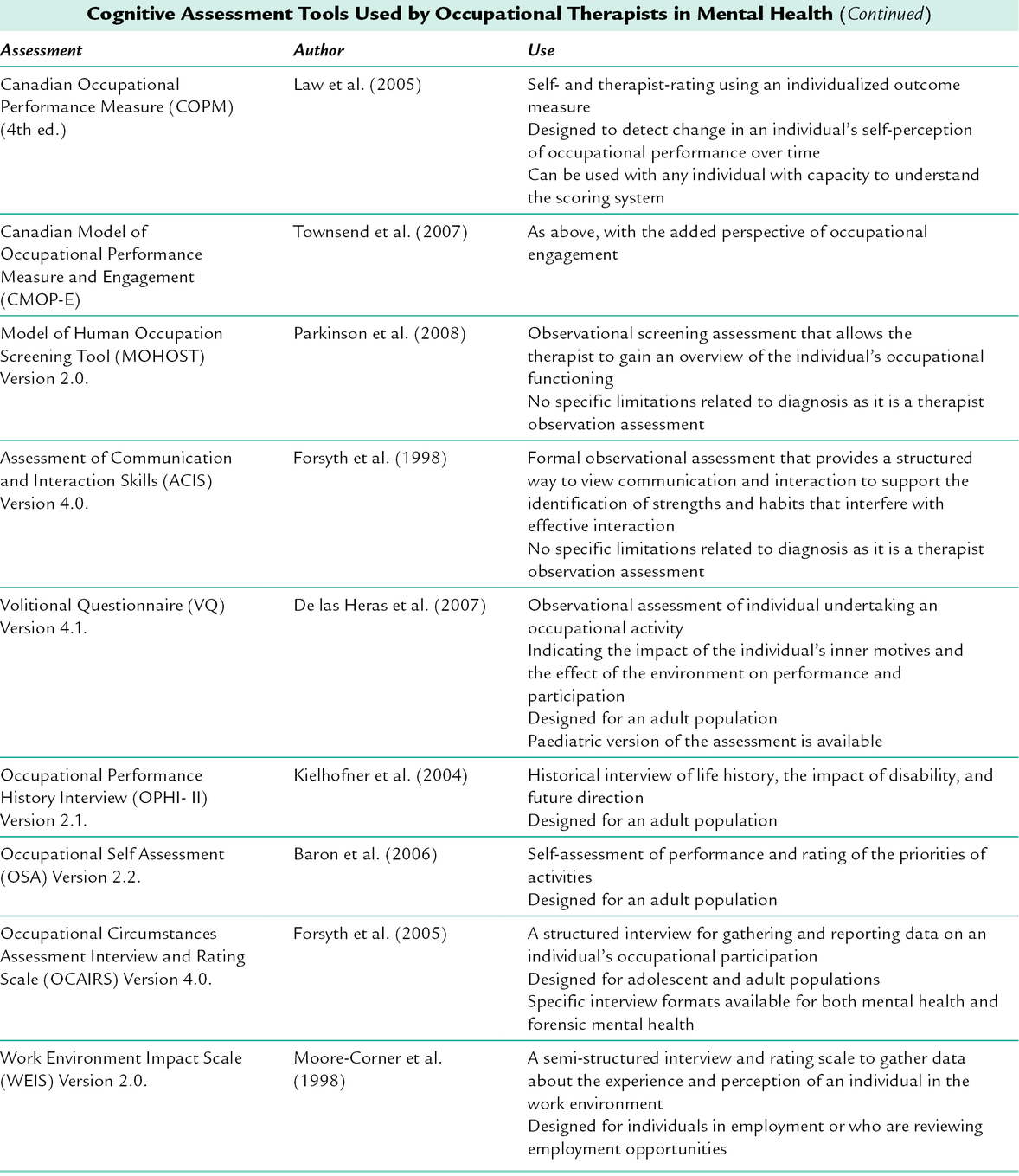
Assessment Tools
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree