5 Cranial Nerves III, IV, and VI
Oculomotor, Trochlear, and Abducens Nerves: Ocular Mobility and Pupils
Cranial Nerve III: Oculomotor
Clinical Vignette
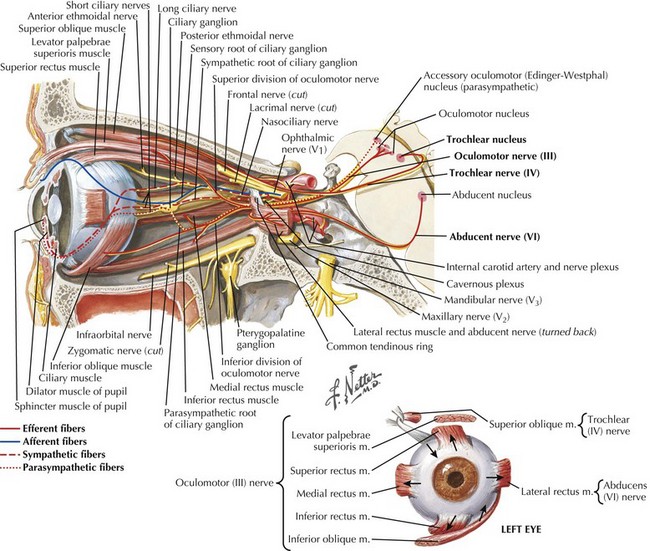
CN-III begins at its nucleus in the midline upper midbrain. The nucleus is a lepidopteroid collection of nine subnuclei located in the center of the rostral midbrain at the level of the superior colliculi (Fig. 5-1). The most ventral of these subnuclei is the central caudate nucleus, a midline structure that innervates both levator palpebrae muscles. Uniquely, axons from the medial subnuclei or columns decussate completely to innervate the contralateral superior rectus muscles. The other six subnuclei, three left-and-right pairs, innervate ipsilateral extraocular muscles. The ventral subnucleus, intermediate column, and dorsal subnucleus, respectively, control the medial rectus (eye adduction), inferior oblique (intorsion and some elevation), and inferior rectus (depression).
Etiology and Pathogenesis
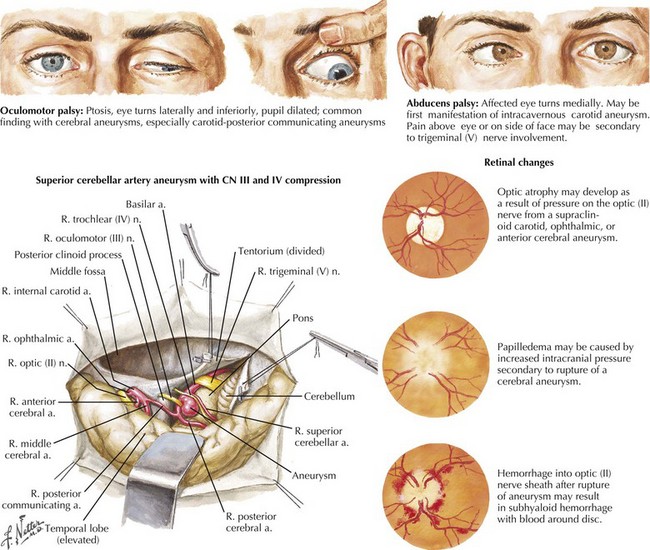
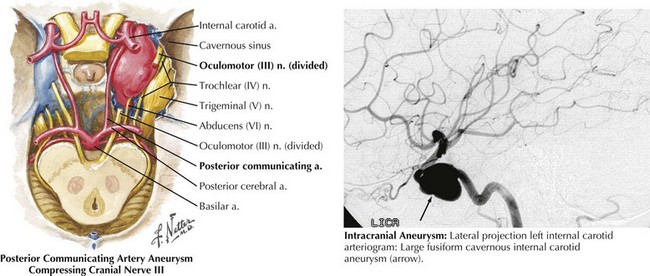
In the patient presenting with acute, severe headache and pupil-involved CN-III palsy, an expanding aneurysm, usually of the posterior communicating artery (p-com), is the most important cause (Fig. 5-2). The location of these aneurysms is the origin of p-com at the ICA (Fig. 5-3) and 90% of these aneurysms present with CN-III palsy. Aneurysm in other nearby arteries can likewise present as CN-III palsy, with up to 30% of acquired CN-III palsies being caused by aneurysms.
Management and Therapy
The management of symptomatic intracranial aneurysm is usually urgent, via endovascular or surgical intervention if the general state of the patient permits (see Chapter 57). Management of microvascular palsy usually centers on prevention of recurrent events via reduction of risk factors. Optimization of any causative disease, such as diabetes, is crucial, and daily aspirin is often recommended. Therapy for other underlying causes of CN-III palsy will vary, appropriate to etiology.
Cranial Nerve IV: Trochlear
Clinical Vignette
The superior oblique is chiefly a depressor of the globe and is most active when the eye is adducted and depressed. It has a secondary function of intorting the eye during ipsilateral head tilt and is a weak abductor of the eye in downgaze (Fig. 5-4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree