Craniosynostosis
Craniosynostosis is the premature closure of one or more sutures of the cranial vault. Early fusion of cranial sutures will generally cause abnormal growth of the cranial vault and skull base, and it may affect brain growth and development.
Physicians as far back as Hippocrates and Galen recognized the relationship of the cranial sutures to skull deformities.1 By the 16th century, anatomists had described a wide range of cranial deformities associated with premature closure of cranial sutures.1–4 Andreas Vesalius, in his work De Humani Corporis Fabrica, illustrated both absent sutures and several abnormal skull shapes, which he described in terms of prominences2 (▶ Fig. 19.1). In 1791, von Sommerring was the first to describe bone growth in the skull as occurring primarily at suture lines, and to note that an abnormal head shape would expand in a plane parallel to a fused suture.5 In 1851, Virchow first described characteristic abnormal growth patterns with specific synostoses, and he classified the morphological descriptions still used today.6 The premise that normal skull growth tends to be in a plane perpendicular to the suture and abnormal growth is parallel to the fused suture is generally called Virchow’s law.
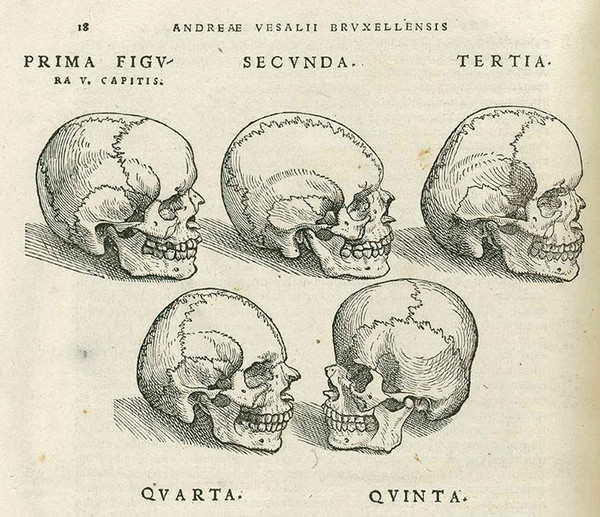
Fig. 19.1 Illustrations of abnormal skull shapes by Andreas Vesalius from De Humani Corporis Fabrica.
(Courtesy of Oregon Health & Science University.)
As our understanding has progressed, it appears that the relationship between sutures and skull growth is not as straightforward and linear as originally proposed. Moss, in 1959, was the first to appreciate the deterministic effect of the skull base on the cranial vault and proposed that the primary mechanisms driving cranial deformity originated at the cranial base, not the sutures.7 He noted that removal of a fused suture did not always alter abnormal skull growth, an observation that contributed to the development of more complex surgical procedures than simple strip craniectomies.
As a result of better understanding of the condition and newer technologies, the surgical treatment for craniosynostosis has undergone interesting trends. Early suturectomies in the late 19th and early 20th centuries were abandoned because of poor patient selection and a high mortality rate.8 In the mid-1900s, suturectomies were again popularized, but outcomes were variable and limited by early refusion and inconsistent results.1,9 The theories of Moss, combined with the pioneering work of Tessier in the 1970s, led to extensive cranial vault reconstruction procedures to correct synostosis that remain popular today. However, with new minimally invasive techniques and adjuvant therapies, such as helmets, springs, and internal distractors, a new era of treatment options is emerging.
19.1 Epidemiology and Etiology
Craniosynostosis affects 1 in every 2,000 to 2,500 live births.10,11 Single-suture synostoses are most frequently observed, with an increased frequency seen in children who have non-Hispanic white mothers.12,13 The sagittal suture is most commonly involved, accounting for 53 to 60% of all cases of craniosynostosis with a male-to-female ratio of 2:1. Coronal synostosis follows, accounting for 17 to 29% of cases and manifesting twice as frequently with unilateral involvement as with bilateral involvement. Metopic synostosis occurs in 4 to 10% of cases, and lambdoid synostosis is the least common, accounting for fewer than 2% of cases.10,14,15 Syndromic craniosynostosis, representing fewer than 5% of all cases, is discussed in a separate chapter.
The etiology of nonsyndromic craniosynostosis is incompletely understood, and most cases appear to be sporadic.16 Numerous factors have been implicated, ranging from genetic mutations and metabolic and hematologic syndromes to teratogens such as valproic acid and retinoic acid. Maternal smoking and advanced paternal age have also been implicated.17–20 It is likely that a combination of genetic factors and external forces mediates the pathway to suture fusion. More than 100 mutations have been identified in association with craniosynostosis, including mutations of the FGFR1–3, NELL1, MSX2, TWIST, and GLI3 genes.11,21 It is unknown how significant a role these genetic anomalies play in the development of synostosis, and genetic and molecular findings have had only minimal clinical impact thus far on the treatment of patients with this problem.
19.2 Physiology and Anatomy
The skull base and cranial vault originate from neural crest cells that surround the enlarging brain. At 5 to 6 weeks of gestation, dural condensations form, and islands of cartilage subsequently develop over the dura. These islands go on to become the osteoblastic ossification centers that form the calvarial bones. The junction of osteogenic fronts forms sutures, best described as sites of bony adaptation rather than as primary growth centers,22 by 16 weeks of gestation. The mechanistic forces that modulate bone growth at the sutures include underlying brain growth, interactions at the dural–calvarial interface, and external mechanical forces.23–25 Supporting a genetic underpinning to the condition, experimental studies have shown that compression of a suture, as with an external mechanical force, will cause bone resorption along the suture margin rather than suture fusion.26,27 Distraction of a suture, such as with elevated intracranial pressure (ICP), will lead to bone growth along the suture edge, with ensuing enlargement of the calvarial bones and cranial vault. After birth, the cranial vault grows most rapidly during the first year of life, with brain volume doubling during the first 6 months and again by age 2 years. The calvaria then continues to grow in a linear fashion until the age of 6 to 7 years, when growth via sutures is essentially complete.
Virchow’s initial hypothesis of skull deformity can be extrapolated to explain the characteristic skull shapes associated with individual forms of craniosynostosis. Delashaw et al redefined the mechanism with the following tenets: two cranial bones connected by a prematurely fused suture will act as a single bone plate, with reduced growth along the margins of that plate, and compensatory skull growth will occur symmetrically along sutures that are in line with a synostotic suture28 (▶ Fig. 19.2).
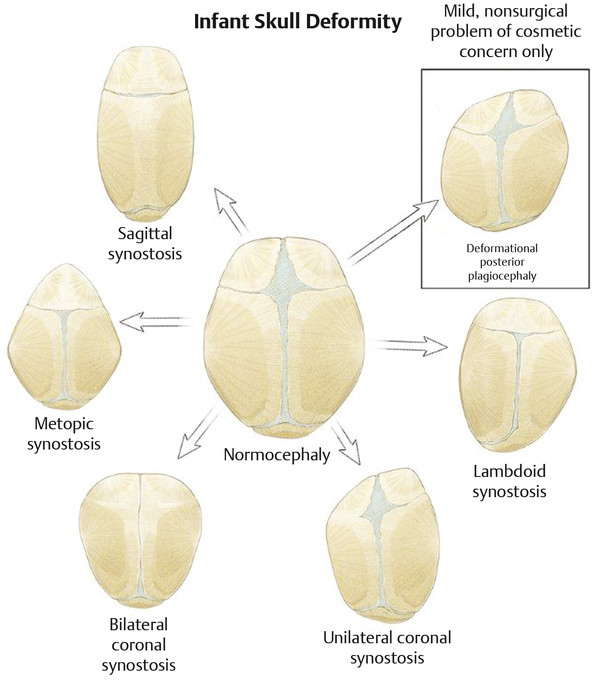
Fig. 19.2 Normal skull anatomy and pathologic skull conditions.
19.3 Diagnosis
The diagnosis, management, and treatment of patients with craniosynostosis can be quite variable, depending on the number of sutures involved and the severity of disease. For severe cases or those with syndromic associations like syndactyly, the initial diagnosis may be established in utero based on morphology. Nonsyndromic craniosynostosis will typically be diagnosed postnatally by observation of a characteristic skull shape. The deformity is generally visible at birth, although occasional mild deformities may be missed. Although the most apparent findings on physical examination will be characteristic calvarial shapes, perisutural ridging may also be noticed. Associated medical conditions, although uncommon in single-suture synostosis, may include midface hypoplasia, deafness, blindness, learning disabilities, speech impairments, swallowing dysfunction, nasopharyngeal airway obstruction, heart and lung abnormalities, and extremity abnormalities.
Radiographic imaging may be used to corroborate the physical examination findings or to rule out an associated intracranial abnormality, although it is rarely needed to establish the diagnosis. It is important to define clearly the questions to be addressed by any imaging and avoid unnecessary studies. Underlying intracranial pathology may be present in a significant number of patients with craniosynostosis,29 although it is not likely to have a major impact on treatment strategies.30
Skull X-rays are frequently obtained when a diagnosis of craniosynostosis is suspected, yet they have minimal diagnostic value beyond that of a detailed physical examination and are often misinterpreted. Three-dimensional computed tomography (CT) provides a comprehensive view of the suture as well as the overall head shape (▶ Fig. 19.3a,b) and will clearly confirm a diagnosis of craniosynostosis, although it should be used judiciously. Exposure to CT has been associated with subsequent malignancies,31,32 and all effort should be made to minimize the unnecessary exposure of infants to radiation. Sedation risks will also be added to the potential negative factors associated with neuroimaging. Three-dimensional CT should be reserved for those cases that require visualization of the skull base, involve multiple or complicated suture pathology, or have an unclear diagnosis. If the diagnosis of synostosis is clinically obvious and concern for brain pathology exists, the use of ultrasound or magnetic resonance (MR) imaging should be considered a safer alternative to CT.
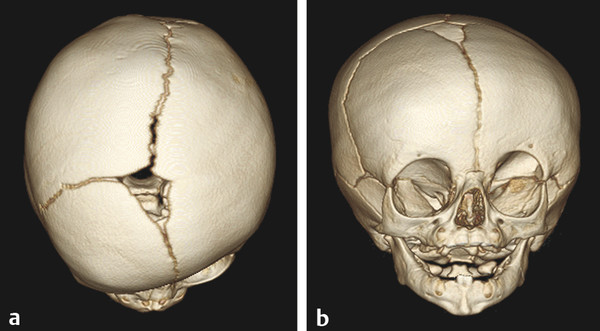
Fig. 19.3 Three-dimensional CT scans in a case of unilateral coronal synostosis showing in exquisite detail both (a) sutural closure and (b) facial deformity.
19.4 Indications for Surgical Treatment
There is wide variation in the management of craniosynostosis. No definitive data exist to guide optimal timing or type of surgical intervention, and treatment will vary based on age of the patient at presentation, location and number of synostoses, severity of deformity, and ultimately the preferences of the treating surgeon(s). In order to standardize the care of these children, the Centers for Disease Control and Prevention (CDC) brought together international specialists in all associated disciplines to establish and publish parameters of care.11,33 Common themes of that document include the complexity of the management of these children and the benefits of multidisciplinary care in craniofacial centers.
The two main indications for the surgical treatment of craniosynostosis are to correct the skull shape for aesthetic and psychosocial considerations and to make certain that there is adequate space for normal brain growth. From an aesthetic perspective, the deformities associated with craniosynostosis are generally progressive for the first year of life, and their social and psychological impact on affected children is in itself sufficiently concerning to justify treatment.34
The relationship between craniosynostosis and brain development is not completely understood. It has been postulated that global intracranial hypertension,35–39 focal brain hypoperfusion,40–42 and mechanical deformation of neuroanatomical structures43–47 may all play varying roles. Studies attempting to demonstrate a relationship between intellectual and behavioral disabilities and craniosynostosis have had varying and sometimes contradictory results.14,46–66 Some data have suggested a benefit to early surgical treatment; however, recent genetic studies have suggested that some genes implicated in craniosynostosis are also essential to brain growth,67 and it remains unclear if skull morphology is simply associated with or an influential factor in abnormal brain development.
A study assessing the neurodevelopment of infants both before and after surgical treatment for single-suture craniosynostosis found that developmental testing results were similar after surgical treatment and within a normal range when compared with those of controls.64 Surgical timing did not appear to affect patient scores. Although it appears that developmental scores remain generally normal and stable in the perioperative periods, differences become more apparent later in childhood. A recent multicenter study demonstrated consistently lower mean neurodevelopmental scores in 3-year-old children who had been treated for single-suture craniosynostosis when they were compared with controls,68 suggesting that these children are at risk for developing cognitive and behavioral disabilities in their school years, regardless of surgical correction.
Although the risk varies depending on the specific diagnosis, a small but significant percentage (4 to 14%) of patients with single-suture synostosis may develop intracranial hypertension,35,69,70 and the incidence is as high as 47 to 67% in patients with multiple involved sutures.35,69,71 The underlying pathologic mechanism responsible for elevated ICP is likely multifactorial but may include cephalocranial disproportion, venous outflow obstruction, upper airway obstruction, hydrocephalus, and narrowing of the cranial foramina.35,70,72–74 Intracranial hypertension may develop gradually, but it should be evident within the first 6 years of life, when brain growth is nearly complete.
The relationship of elevated ICP to cognitive outcomes is unclear. Renier et al performed psychometric testing and invasive ICP monitoring in children with craniosynostosis in a 1989 report from the Hôpital des Enfants Malades in Paris.69 Elevated ICP (> 15mm Hg) was found in 8% of patients with sagittal synostosis, 6% of those with metopic synostosis, and 12% of those with unilateral coronal synostosis. Patients who had multiple fused sutures or who presented after 1 year of age had higher rates of pathologically elevated ICP. A statistically significant relationship was found between ICP and cognitive capacity, with higher ICPs correlated to lower developmental quotients (DQs) and intelligence quotients (IQs). Other relevant reports in the literature have demonstrated improved behavior with resolution of papilledema,75,76 improved IQ and developmental progress following cranial vault expansion for documented intracranial hypertension,69 and poorer cognitive function in those children with elevated ICP presenting after the age of 3 years.69
19.5 Surgical Treatment
Surgical methods for correcting craniosynostosis-related skull deformities have evolved over time, and multiple techniques have been found to have acceptable results. Available data have yet to demonstrate a single best procedure for the treatment of synostosis, which would indicate that there are many acceptable methods for treating the condition. Treatment considerations should include patient age, severity of the disorder, and associated medical conditions. Intervention early in life has the advantage of utilizing the effects of the rapidly growing brain to reshape the skull, along with halting secondary deformities in the face, skull base, or cranial vault that occur over the first year of life. Generally, the procedures in young infants tend to be less invasive, but the increased surgical risk in smaller infants should be considered. Endoscopic techniques in which postoperative helmets are used to direct skull growth are generally best performed by 3 to 6 months of age, whereas spring- or distractor-mediated techniques can be used in older infants, as brain growth is no longer the driver of skull growth. Open cranial vault remodeling procedures are often delayed until 6 to 12 months because they are associated with greater blood loss and longer operative times, and many surgeons have observed an increased incidence of revision surgery in patients operated on before 6 months. Treatment options become more limited as a child grows older, and therefore early diagnosis and referral to a craniofacial center are important.
19.5.1 Open Reconstructions
In the 1970s, Tessier pioneered the technique that remains the standard of care to this day.77,78 Extensive surgical reconstruction was performed during which large segments of cranium were removed, remodeled, and stabilized with rigid fixation. This procedure had the advantages of establishing the desired skull shape and size intraoperatively, and of achieving predictable immediate outcomes. Disadvantages to these open procedures include significant blood loss, lengthy surgical times and hospital stays, and frequent need for postoperative intensive care unit monitoring. Because surgery is usually delayed until the patient is older in order to minimize operative morbidity, the cranial deformities can become more severe before intervention. The manipulation of large segments of the skull also disrupts the dural–calvarial interface, which may affect future growth and lead to less predictable results over time.
19.5.2 Minimally Invasive and Endoscopic Surgery
Endoscopic and minimally invasive treatments for craniosynostosis are growing in both popularity and demand by patients‘ families. Although early suture release surgeries failed to correct cranial deformities in a substantial percentage of patients because of rapid sutural refusion, external orthoses, internal springs, and distractors have negated this problem. Barone and Jimenez published their initial experience with endoscopic suturectomy and adjunctive postoperative orthotic treatment in 1999,79 and their data have been supported by others.80–82 In comparison with conventional open cranial vault remodeling, there are significant reductions in blood loss and need for transfusions, smaller incisions, shorter surgical times, shorter hospital stays, and overall decreased hospital costs. The smaller operations are more limited in spectrum, however, and older patients or those with severe cranial deformities may not be candidates.
The benefit of shorter operative times in these procedures may be profound; a recent report from Naumann et al demonstrated lower mean neurodevelopmental scores among children who had undergone lengthier operations and had greater exposure to inhaled anesthetics for cranial vault surgery for single-suture craniosynostosis during infancy.83
Postoperative skull-molding helmets are most commonly used as an adjunct to endoscopic strip craniectomies. Helmets have the advantage of being adjustable over time, and they have the capacity to modify skull growth in three dimensions. However, they are less effective in infants older than 3 to 6 months. Springs and distractors have the disadvantage of requiring an additional operation to remove them, but they allow predictable advancements in a single plane of growth and also can be used in older children because brain growth is no longer the essential driver of skull growth.
Regardless of surgical techniques, long-term follow-up is important in children treated for craniosynostosis; it should include observation of cranial vault growth and morphology as well as of neurocognitive and psychosocial development until at least 6 years of age.11,33 Perhaps the most useful tool for following a child with craniosynostosis is head circumference. If the growth rate falls, deformity recurs, or clinical symptoms ensue, the child should be evaluated with appropriate imaging studies and an ophthalmologic evaluation. Adjunct procedures may be necessary in a subpopulation of these patients, regardless of the type of initial treatment.
19.5.3 Surgical Techniques
The technique for surgical reconstruction should be tailored to the type of synostosis and the age of the patient, and each surgeon will develop certain nuances in the way the procedures are performed. Interestingly, despite the relatively wide variations in phenotypic presentations, the surgical approaches have many similarities. It would be beyond the scope of this chapter to describe each technique for each type of synostosis in great detail, as authors have described literally dozens of variations for each suture type. However, there are many broad concepts that are important for both minimally invasive and open techniques that are discussed here, with the salient features for particular sutures covered in the individual sections that follow.
Endoscopic Techniques
Like that of open suturectomy in the past, the main goal of minimally invasive techniques is to release the fused suture(s) without an attempt at major reconstruction or contour change at the time of surgery. This is especially true for metopic, coronal, and lambdoid sutures and also can hold true for sagittal synostosis, although some authors recommend fairly wide vertex craniectomy and parietal barrel staving for this condition. The incisions are generally limited to 2 cm, and it is important to avoid wide dissection of the soft tissues so as to avoid unnecessary bleeding. Bur holes are placed with a high-speed drill and then locally enlarged with a Kerrison rongeur. Once this is achieved, the periosteum is stripped from the outer surface of the bone, and the endoscope is used to strip the dura from the undersurface of the fused suture. The surgery is made particularly feasible by the ease with which dura separates from a fused suture. Finally, the craniectomy may be completed with heavy scissors, ultrasonic bone aspirators, or a high-speed drill. Bone edges can then be coated with wax or Gelfoam, with a pressure dressing placed after wound closure for several hours. Despite concerns about the risks for uncontrolled bleeding from torn venous sinuses, the experience of multiple authors has clearly shown this to be a safe technique with a much lower risk for bleeding than open operations.79,80,82,84 Within 1 week of the procedure, the infant is fitted with a cranial molding helmet. An orthotist and the craniofacial team follow the patient closely and make necessary adjustments to the helmet until the desired phenotype is achieved or the infant reaches 1 year of age.
Open Cranial Vault Reconstruction
These operations, pioneered by Tessier in the 1970s, are by and large variations of similar procedures. Indeed, metopic and coronal suture operations are very similar variations of what is commonly referred to as the fronto-orbital advancement. The patient is placed supine—except in the case of some types of sagittal synostosis, when a more posterior correction is anticipated—with the head stabilized in a horseshoe headrest. In all cases, the cranium is accessed via a bicoronal skin incision, which gives excellent access to any portion of the skull and is more cosmetically acceptable than a bifrontal incision. A zigzag incision is used in order to minimize the visibility of incisional scalp alopecia. Minimal hair shave tends to be necessary. Incisions in the anteroposterior plane, occasionally used for sagittal synostosis, are very difficult to work with if revision surgery is ever needed. The anterior and posterior scalp flaps are dissected in the subperiosteal plane to prevent anchoring of bone to periosteal tissue. The dissection is carried forward into the subperiorbital plane in order to allow bilateral orbital rim osteotomies. Once the skull is accessed, all cranial vault surgeries require the removal of large sections of bone to be replaced in a more anatomically normal position, either homotopically (bone replaced to a similar location) or heterotopically (segments of bone moved to different parts of the skull), based on the surgeon‘s preference. Bone is removed with high-speed drills, and the rate of dural tears should be low because of the integrity of the dura in children. Sagittal saws and osteotomes are useful for removal of the orbital bandeau, which requires cuts through the frontozygomatic process, roof of the orbits, and nasofrontal junction. Blood loss is often steady, but hemostasis should be achieved with the selective coagulation of emissary veins and the application of wax on bone edges. The advent of absorbable plates truly has simplified the surgery by making secure bone replacement readily achievable. Most commercially available plates resorb in 1 to 2 years. Titanium plates should not be used in infants, as they will migrate intracranially as the skull grows.85,86 Once all bone is secured, it is advisable to fill bone gaps with the patient’s own bone, often a particulate mixture taken from the inner cortical surface, as gaps often will not fill on their own.87,88 The incision is then closed with a subgaleal drain, and pressure wrap head dressing is applied. The specifics by suture site are discussed below.
Metopic Synostosis
Clinical Features
Metopic synostosis leads to a characteristic triangular skull morphology known as trigonocephaly. Severe cases will demonstrate ridging of the metopic suture (“keel” forehead), posterior displacement of the superolateral orbital rims, hypotelorism, flattening of the frontal bones, anterior displacement of the coronal sutures, compensatory bulging of the parieto-occipital region, and temporal narrowing. Normal closure of the metopic suture occurs by 9 months, although physiologic closure can occur as early as 3 months, and not all children with premature closure will develop trigonocephaly. Patients who present with only mild ridging of the suture are best treated with conservative measures only. Trigonocephaly has the highest rate of associated cognitive impairment among the single-suture synostoses.
Open Surgical Techniques
As described above, fronto-orbital advancement is used to normalize the forehead and remodel the supraorbital rim. A bifrontal craniotomy is performed with the posterior extent to the coronal suture. The orbital bar is removed in one piece and reconstructed into a more convex configuration with a midline osteotomy if necessary. To correct hypotelorism, the orbital bandeau can be widened with insertion of a bone strut between the two halves. The reshaped orbital rim is then fixed to the nasal bone and angled forward at the frontozygomatic suture.
The frontal bones are split along the midline and replaced in a widened fashion, with radial barrel staves used as needed to widen it. The remaining temporal parietal region should be barrel-staved and fractured laterally to flare out and match the newly replaced frontal bones.
Endoscopic Techniques
Infants younger than 6 months with trigonocephaly may be considered for an endoscopic strip craniectomy. In general, the results are quite good, although the ultimate frontal bone projection often falls slightly short of that achieved with the traditional fronto-orbital advancement.80 For a metopic procedure, the patient is placed supine with the head stabilized on a horseshoe headrest. One midline incision approximately 1.5 to 2.5 cm in length is made just posterior to the hairline, with an orientation perpendicular to the metopic suture (▶ Fig. 19.4). Often, two emissary veins will be encountered when the dura is stripped, but these are easily coagulated with bipolar cautery and divided. After the craniectomy, the ultrasonic bone aspirator is helpful in reaching around the frontal curvature to ensure that sufficient bone is removed at the nasofrontal juncture.

Fig. 19.4 Positioning of a child for endoscopic release of metopic synostosis.









